Multiple, non-syndromic BCCs involving a hypopigmented patch
Ahmad Al Aboud 1, Mohammad Hakim2, Fawaz Aljohani1, Ibrahim Alehibi2, Homaid Alotaibi2, Yusra Bindogji2, Rana Al Zaidi3, Tahani Alehibi4, Asma Almalki5
1, Mohammad Hakim2, Fawaz Aljohani1, Ibrahim Alehibi2, Homaid Alotaibi2, Yusra Bindogji2, Rana Al Zaidi3, Tahani Alehibi4, Asma Almalki5
1Department of Dermatology, King Abdullah Medical City, Makkah, Saudi Arabia, 2Department of Dermatology, King Faisal Hospital, Makkah, Saudi Arabia, 3Department of Pathology, King Faisal Hospital, Makkah, Saudi Arabia, 4Department of Emergency, King Faisal Hospital, Makkah, Saudi Arabia, 5Department of Education, King Faisal Hospital, Makkah, Saudi Arabia
Corresponding author: Ahmad Al Aboud, MD
How to cite this article: Al Aboud A, Hakim M, Aljohani F, Alehibi I, Alotaibi H, Bindogji Y, Al Zaidi R, Alehibi T, Almalki A. Multiple, non-syndromic BCCs involving a hypopigmented patch. Our Dermatol Online. 2022;13(e):e58.
Submission: 12.06.2022; Acceptance: 01.08.2022
DOI: 10.7241/ourd.2022e.58
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Basal cell carcinoma (BCC) is the most common human malignant neoplasm. It has a slowly progressive nature and a locally invasive behavior. Both genetic predisposition and exposure to environmental risks are involved in its pathogenesis. An ever-increasing annual incidence is observed. Multiple BCCs may be seen in some syndromes such as nevoid basal cell carcinoma syndrome (NBCCS), also known as Gorlin–Goltz syndrome. The occurrence of multiple, concurrent, non-syndromic BCCs is rare. Herein, we present a concise report of an observation of multiple, non-syndromic BCCs involving a hypopigmented patch on the forehead in an adult Afghani patient.
Key words: Basal Cell Carcinoma (BCC); Hypopigmentation; Isotopic Response
INTRODUCTION
Basal cell carcinoma (BCC) is the most common human cutaneous malignant epithelial neoplasm [1–3]. BCC occurs in sporadic (non-syndromic) and syndromic (hereditary) forms. In the first group, which comprises the vast majority of such cases, the affected individuals do not have any genodermatosis susceptible to developing cutaneous malignancies [2]. BCC is known to occur at the same skin location of neoplastic and non-neoplastic cutaneous conditions [3]. Multiple BCC’s might occur at the same time (synchronously) or as one following the other with a time gap [2]. Multiple BCCs may occur in a different skin location or in the same [2].
Here in, we report a case of multiple, non-syndromic BCCs involving a hypopigmented patch on the forehead.
CASE REPORT
A 39-year-old, male, Afghani patient, not known to have had a chronic medical problem before, presented with expanding, asymptomatic skin lesions on the forehead persistent for five months in an area of hypopigmentation.
The patient first developed the hypopigmentation, then developed the lesions and failed to remember exactly when he noticed the hypopigmented patch. The patient had a history of excessive sun exposure and most of his activities were outdoor. He had no personal or family history of vitiligo or skin tumors.
An examination revealed three plaques of various sizes involving a non-scaly hypopigmented patch on the right side of the forehead (Fig. 1a). No abnormalities were seen on the rest of the skin. The hair, nails, and mucous membranes were normal.
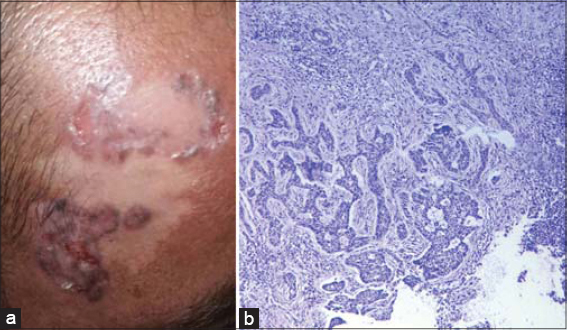 |
Figure 1: (a) Involvement of the hypopigmented patch on the forehead by multiple BCCs. (b) Infiltrative strands of basaloid cells in the dermis with a retraction artifact (H&E, 20×). |
Skin biopsies from the largest two plaques confirmed the diagnosis of BCC of an infiltrative type in both samples (Fig. 1b). The patient was scheduled for surgical excision.
DISCUSSION
Approx. 29% of patients with a first BCC will develop at least one more lesion during their lifetime. The candidate predictors for the development of multiple BCCs include a younger age and the superficial BCC subtype on the first diagnosis, the red hair phenotype, the initial or frequent tumor location on the trunk or on the upper limbs, and the male sex [2].
Multiple BCCs may be encountered in several genetic syndromes–for instance, Gorlin–Goltz syndrome, Bazex syndrome, and xeroderma pigmentosum–yet may also occur in patients with no genetic syndrome, as in our case.
According to the literature, the percentage of patients with more than one primary BCC varies from 7% to 46% [2,4]. Multiple BCCs occurring in the same location simultaneously is uncommon. This type of presentation has been named by the literature as multiple presentation phenotype/cluster initial [2,5].
In this case, no biopsy was performed for the third, small plaque (Fig. 1), yet we believe it was also a BCC, as in the case of the two larger plaques. It is difficult to be certain in our case, yet we think that the hypopigmented patch was nevoid in nature (nevus achromicus or nevus anemicus). The clinical and histopathological findings did not favor other possible causes of hypopigmentation, such as vitiligo, leprosy, or postinflammatory hypopigmentation.
BCC is known to complicate lesions of nevoid nature, such as nevus sebaceous.
Pineder et al. [6] reported a 24-year-old female with a BCC on the forehead masquerading as a vitiliginous patch. This case was obviously different from our case, and we know of no report of a similar presentation to our case.
BCC has also been reported to concurrently occur in the same skin location of several cutaneous conditions. This could be secondary to either the Koebner isomorphic response or the Wolf isotopic response in an immunocompromised district of the skin (Ruocco’s immunocompromised cutaneous district) [3,7].
It is likely that the hypopigmented patch in our case acted as an immunocompromised district of the skin (locus minoris resistentia) and primed the skin to the carcinogenic effect of ultraviolet light, and hence resulting in BCCs.
Further reports of similar observations may support this concept. We also encourage examining the skin areas affected by BCC for any possible local risk factor.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Cohen PR, Calame A. Multiple Skin Neoplasms at One Site (MUSK IN A NEST):A comprehensive review of basal cell carcinoma and benign or malignant “collision”tumors at the same cutaneous location. Clin Cosmet Investig Dermatol. 2020;29;13:731-41.
2. Bartos V. Development of multiple-lesion basal cell carcinoma of the skin:A comprehensive review. Sisli Etfal Hastan Tip Bul. 2019;19;53:323-8.
3. Cohen PR. Basal cell carcinoma associated with non-neoplastic cutaneous conditions:A comprehensive review. Dermatol Online J. 202115;27:13030/qt37k7465h.
4. Quigley C, Raghallaigh SN. Metastatic basal cell carcinoma:A report of two cases and a review of the literature. Our Dermatol Online. 2022;13:73-6.
5. Elloudi S, Oulehri A, Baybay H, Douhi Z, Mernissi FZ. Advanced basal cell carcinomas of the face:A Moroccan series. Our Dermatol Online. 2021;12:135-9.
6. Pineider J, Ken KM, Savory S, Nijhawan RI. Basal cell carcinoma masquerading as vitiligo in a young woman. JAAD Case Rep. 2020;16;6:584-6.
7. Tabosa GVBS, Stelini RF, Souza EM, Velho PENF, Cintra ML, Florence MEB. Immunocompromised cutaneous district, isotopic, and isopathic phenomena:Systematic review. J Cosmet Dermatol. 2021;20:410-6.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.