Progressive dermoscopy of palmoplantar syphilides
Ryme Dassouli , Zakia Douhi, Souad Choukri, Hanane Baybay, Sara Elloudi, Fatima Zahra Mernissi
, Zakia Douhi, Souad Choukri, Hanane Baybay, Sara Elloudi, Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Fès, Morocco
Corresponding author: Ryme Dassouli, MD
How to cite this article: Dassouli R, Douhi Z, Choukri S, Baybay H, Elloudi S, Mernissi FZ. Progressive dermoscopy of palmoplantar syphilides. Our Dermatol Online. 2022;13(e):e43.
Submission: 20.01.2022; Acceptance: 10.04.2022
DOI: 10.7241/ourd.2022e.43
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Syphilides are eruptions of secondary syphilis made of asymptomatic coppery papules whose palmoplantar localization is very suggestive [1]. However, in 30% of cases, they can take on other clinical presentations that can lead to diagnostic difficulty and therapeutic delay. We aim to highlight the use of the dermoscope as an auxiliary tool for the identification of palmar syphilides at the different evolutionary stages.
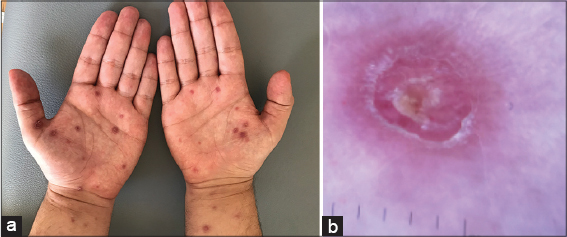
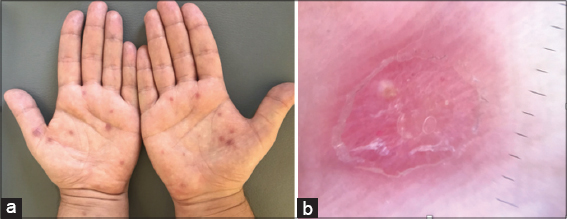
A 25-year-old patient with notions of homosexuality and unprotected sex presented with an asymptomatic reddish rash that was a week old. Dermatological examination found scattered copper-red papules on the face, trunk and palms of the hands. The palmar lesions were multiple made up of small raised copper-red papules surrounded by fine desquamation (Biett’s collarette) (Fig. 1a). Palmar dermoscopy described a pinkish-red lesion, dark in the center and gradually fading toward the periphery. Fine yellow-orange scales with a circular peripheral distribution surround the lesion. There is also an orange background to the lesion. In contrast, no vascular pattern was visualized (Fig. 1b). The rest of the somatic examination was normal. The workup revealed a positive syphilitic serology with a VDRL level of 1/64, a positive HIV serology. The patient was treated with 3 injections of depot penicillin. Clinical inspection of the palmar lesion in the week following the injection showed a collapse of the syphilids and disappearance of Biett’s collar (Fig. 2a). Dermoscopic examination showed a desquamation from the center to the periphery with attenuation of the reddish color and disappearance of the orange background (Fig. 2b).
Syphilis and HIV infection are common in HIV-infected patients and the reverse is also true. Syphilis produces genital lesions or an inflammatory response (macrophages and T cells) that promote HIV replication. There is a strong epidemiological association between HIV and syphilis. Several unusual manifestations of syphilis observed in the presence of concurrent HIV infection are increased severity of clinical manifestations, rapid progression of syphilis to the tertiary stage within weeks or months of initial infection [2].
Secondary syphilis occurs as a result of blood or lymphatic dissemination of Treponema Pallidum. It manifests as an asymptomatic morbilliform rash during the first bloom, and a few weeks later, the second bloom [3]. This stage is characterized by specific asymptomatic lesions called syphilis. Syphilis are bright coppery red papular lesions surrounded by a fine circular desquamation called Biett’s collar, they are symmetrical and diffuse on the face, trunk and limbs. Palmoplantar localization is rare but characteristic of the disease [4]. The clinical aspect sometimes takes on other presentations that can make the diagnosis difficult. Progressive dermoscopy is useful for the early identification of syphilis compared to other inflammatory diseases, thus allowing a better diagnostic orientation and an adequate therapeutic management. The main dermoscopic signs specific to palmar syphilis are Biett’s collar in the form of a thin circular border surrounded by an erythematous halo, the orange-yellow background which signifies extravasation of hemosiderin, and the vascular pattern which remains undetermined [5]. The dermoscopic evolution of syphilis in one week is marked by a progressive extension of the Biett’s collar towards the outside until the disappearance creating a tartar-like appearance, with a remarkable attenuation of the erythema and the orange background. This favorable evolution over a short period of time confirms the diagnosis of secondary syphilis and requires early treatment to avoid the evolution towards fatal and lasting complications of the disease [6].
Although its diagnostic value is currently limited for syphilis, progressive dermoscopy is useful in the differential diagnosis with other common inflammatory dermatoses. Early diagnosis of secondary syphilis and early treatment prevents fatal disease progression.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Bhugra P, Maiti A. Secondary Syphilis. N Engl J Med. 2020;383:1375.
2. Krishnan A, Samayam A, Patra AK. Syphilis:case series. Our Dermatol Online. 2019;10:286-8.
3. Li W, Barnes E, McNeil C, Palavecino E. Secondary syphilis mimicking sarcoidosis. Clin Case Rep. 2020;8:2237-9.
4. Mathur M, Acharya P, Karki A, Shah J, Kc N. Dermoscopic clues in the skin lesions of secondary syphilis. Clin Case Rep. 2019;7:431-4.
5. Errichetti E, Stinco G. Dermoscopy in differentiating palmar syphiloderm from palmar papular psoriasis. Int J STD AIDS. 2017;28:1461-3.
6. Errichetti E and Stinco G. Dermoscopy in general derma- tology:a practical overview. Dermatol Ther (Heidelb). 2016;6:471–507.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-4330-4429 http://orcid.org/0000-0003-4330-4429 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |



Comments are closed.