Pyoderma gangrenosum: About a pediatric presentation
Jihad Kassel 1, Zakia Douhi1, Chaymae Jroundi1, Hanane Baybay1, Sara Elloudi1, Fatima-Zahra Mernissi1, Chaïmâa Benghabrit2, Kenza Elmkadem2, Sana Abourazzak2, Sana Chaouki2, Moustapha Hida2
1, Zakia Douhi1, Chaymae Jroundi1, Hanane Baybay1, Sara Elloudi1, Fatima-Zahra Mernissi1, Chaïmâa Benghabrit2, Kenza Elmkadem2, Sana Abourazzak2, Sana Chaouki2, Moustapha Hida2
1Department of Dermatology, University Hospital Hassan II, Fes, Morocco, 2Department of Pediatrics, University Hospital Hassan II, Fes, Morocco
Corresponding author: Jihad Kassel, MD
Submission: 02.01.2022; Acceptance: 29.03.2022
DOI: 10.7241/ourd.2022e.41
Cite this article: Kassel J, Douhi Z, Jroundi C, Baybay H, Elloudi S, Mernissi FZ, Benghabrit C, Elmkadem K, Abourazzak S, Chaouki S, Hida M. Pyoderma gangrenosum: About a pediatric presentation. Our Dermatol Online. 2022;13(e):e41.
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir;
Pyoderma Gangrenosum (PG) is a neutrophilic dermatosis that was first described by Brunsting et al. in 1930 [1]. The pathogenesis is poorly understood, several diseases and conditions associated with PG have been described such as Crohn’s disease, ulcerative colitis, polyarthritis, diabetes, myelodysplastic syndromes or myeloid leukemia, monoclonal gammopathy, and systemic lupus erythematosus [2]. Several cases have also been reported after surgery [3]. Pyoderma gangrenosum is very rare in children, with a percentage of only 4%, the most common presentation of PG in children is disseminated ulcerative lesions. The face, groin, thighs, and buttocks are most commonly affected [4]. Other sites affected are the upper and lower extremities [3]. In contrast, involvement of the trunk is less frequently reported. PG usually begins as papules and pustules that rapidly enlarge and eventually become confluent. Progression is to painful ulcers with a central area of necrosis surrounded with an erythematous halo [5]. Extracutaneous manifestations described with PG involve the lungs, eyes, and musculoskeletal system [1]. PG is a diagnosis of elimination, after exclusion of other ulcerative processes. Histopathologic examination shows a dense inflammatory infiltrate of polymorphonuclear leukocytes associated with fibrinoid necrosis of the vessel wall [2]. Treatment is based primarily on systemic corticosteroid therapy, cyclosporine, and dapsone [5]. We report a case of PG in a 3-month-old child.
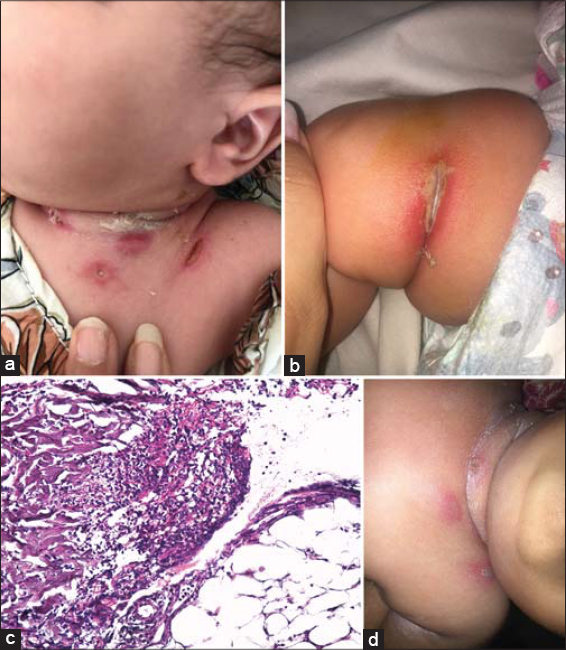
A 3-month-old female child with no previous pathologic history was admitted to the pediatric department. Our opinion was sought for lesions that appeared a week ago on the thigh and neck with a fever. The mother reported that initially the lesions were pustules with subsequent appearance of nodules and ulcerations. Clinical examination revealed indurated subcutaneous nodules, as well as well-limited oval ulcerations with a deep, fibrinous, slightly infiltrated base and erythema at the periphery of the lesion located at the level of the neck and thigh folds (Figs. 1a – 1b). The initial biological evaluation showed anemia, the Blast test was negative, and bacterial and fungal cultures of the skin lesions and blood cultures were repeatedly negative. We suspected ecthyma gangrenosum, cutaneous manifestations of a hematological malignancy, panniculitis, Langerhans cell histiocytosis and pyoderma gangrenosum. We performed a skin biopsy which showed a hyperacanthosis epidermis and dense polymorphic inflammatory infiltrates extending to the hypodermis demonstrating a PG (Fig. 1c). The patient was treated with corticosteroids with a good evolution (Fig. 1d).
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Kechichian E, Haber R, Mourad N, El Khoury R, Jabbour S, Tomb R. Pediatric pyoderma gangrenosum:a systematic review and update. Int J Dermatol. 2017;56:486-95.
2. Carneiro FR, Santos MA, Sousa BA, Nascimento Cdo S, Amin GA, Moutinho AT. Pyoderma gangrenosum in a newborn–case report. An Bras Dermatol. 2013;88(6 Suppl 1):173-5.
3. Mella JR, Maselli AM, Guo L. A Deceptive Diagnosis:Pyoderma Gangrenosum After Breast Surgery-A Case Series and Literature Review. Ann Plast Surg. 2019;83(4S Suppl 1):S21-S30.
4. Torrelo A, Colmenero I, Serrano C, Vilanova A, Naranjo R, Zambrano A. Pyoderma gangrenosum in an infant. Pediatr Dermatol. 2006;23:338-41.
5. Berger N, Ebenhoch M, Salzmann M. Postoperative Pyoderma Gangrenosum in Children:The Case Report of a 13-Year-Old Boy With Pyoderma Gangrenosum After Hip Reconstruction Surgery and a Review of the Literature. J Pediatr Orthop. 2017;37:e379-83.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |



Comments are closed.