Bullous impetigo in a 6-year-old girl
Katarzyna Borowska1, Piotr Brzeziński 2
2
1Department of Histology and Embryology with Experimental Cytology Unit, Medical University of Lublin, Lublin, Poland, 2Department of Physiotherapy and Medical Emergency, Faculty of Health Sciences, Pomeranian Academy, Slupsk, Poland
Corresponding author: Piotr Brzeziński, MD PhD
Submission: 20.12.2021; Acceptance: 08.03.2022
DOI: 10.7241/ourd.2022e.31
Cite this article: Borowska K, Brzeziński B. Bullous impetigo in a 6-year-old girl. Our Dermatol Online. 2022;13(e):e31.
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Impetigo is a contagious superficial bacterial skin infection, predominantly affecting children. There are two types of impetigo: nonbullous and bullous. Bullous impetigo is caused by toxin-producing S. aureus. We present a case of bullous impetigo in a 6-year-old girl with skin lesions on the upper limbs.
Key words: Impetigo, Bullous, Nonbullous children
INTRODUCTION
Impetigo is a contagious superficial bacterial skin infection, predominantly affecting children [1].
There are two types of impetigo: nonbullous (i.e., impetigo contagiosa) and bullous. Nonbullous impetigo represents a host response to the infection, whereas a Staphylococcal toxin causes bullous impetigo and no host response is required to manifest clinical illness [2,3,4]. Bullous impetigo most commonly affects neonates but also can occur in older children and adults. Gupta observed bullosa impetigo in 12% among bacterial infections [5].
CASE REPORT
A 6-year-old girl with 5 days history of skin lesions on the upper limbs. Lesions in the type of blisters and erosions were located mainly in the area of the hand (Figs. 1a – 1c). It was associated with minimal itching and there were no constitutional symptoms.
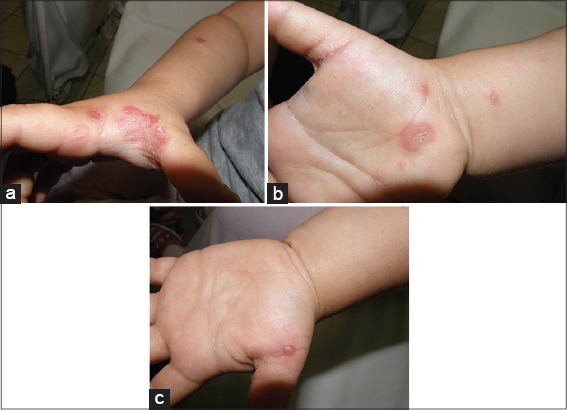 |
Figure 1: (a-c) Bullous impetigo in a 6-year old child. |
The interview shows that the girl suffers from atopic dermatitis; xerosis on the skin has been found.
Other mucosal and nail examinations were within normal limits. This therapy was discontinued, fusic acid and emollient therapy were introduced. A final diagnosis of bullous impetigo was made. The lesions subsided completely after 7 days of treatment.
DISCUSSION
Bullous impetigo is caused by toxin-producing S. aureus and is a localized form of staphylococcal scalded skin syndrome. Superficial vesicles progress to rapidly enlarging, flaccid bullae with sharp margins and no surrounding erythema. Systemic symptoms are not common but may include weakness, fever, and diarrhea [2,5]. In differential diagnosis of bullous impetigo stands out: bullous erythema multiforme, bullous lupus erythematosus or bullous pemphigoid.Ana Maria Abreu Velez et al., insist that chronic bullous dermatosis of childhood (CBDC) is frequently misdiagnosed as bullous impetigo [6]. Therefore, it is important to make an appropriate diagnosis and monitor patients.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Cole C, Gazewood J. Diagnosis and treatment of impetigo. Am Fam Physician. 2007;75:859-64.
2. Gupta M. Pattern of cutaneous infections in pediatric age group –A clinico-observational study. Our Dermatol Online. 2020;11:35-7.
3. Abreu Velez AV, Vasquez-Hincapie DA, Howard MS. Autoimmune basement membrane and subepidermal blistering diseases. Our Dermatol Online. 2013;4 (Suppl.3):647-62.
4. Dagan R, Bar David Y. Double-blind study comparing erythromycin and mupirocin for treatment of impetigo in children:implications of a high prevalence of erythromycin-resistant Staphylococcus aureus strains. Antimicrob Agents Chemother. 1992;36:287–90.
5. Dagan R. Staphylococcus aureus in impetigo. Am. J. Dis. Child. 1991;145:1223.
6. Koning S, van der Sande R, Verhagen AP, van Suijlekom-Smit LWA, Morris AD, Butler CC, et al. Interventions for impetigo. Cochrane Database Syst Rev. 2012;1:CD003261.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-0964-6169 http://orcid.org/0000-0003-0964-6169 http://orcid.org/0000-0001-6817-606X http://orcid.org/0000-0001-6817-606X |



Comments are closed.