Association of pyoderma gangrenosum and rheumatoid polyarthritis in a young lady
Aida Oulehri , Zakia Douhi, Jihad Kassel, Hanane Baybay, Sara Elloudi, Fatima Zahra Mernissi
, Zakia Douhi, Jihad Kassel, Hanane Baybay, Sara Elloudi, Fatima Zahra Mernissi
Dermatology Department of the University Hospital Center Hassan II, Fez, Morocco
Corresponding author: Aida Oulehri, MD
How to cite this article: Oulehri A, Douhi Z, Kassel J, Baybay H, Elloudi S, Mernissi FZ. Association of pyoderma gangrenosum and rheumatoid polyarthritis in a young lady. Our Dermatol Online. 2022;13(e):e23.
Submission: 16.01.2021; Acceptance: 20.03.2021
DOI: 10.7241/ourd.2022e.23
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Pyoderma gangrenosum (PG) is a rare inflammatory skin disease, with an estimated incidence of 3–10 cases per million per year. PG affects individuals of all ages but is the most common in adults between the ages of 40–60 years, with an average age of onset of 44 years. PG is more common in females than in males, with a ratio of 3:1. Approx. 50% of patients with PG have other associated medical conditions. The strongest associations found have been with inflammatory bowel disease (IBD), followed by hematological malignancies and polyarthritis, which are often seronegative [1]. Although, in most cases, no morbid associations are reported [2].
PG is challenging to both diagnose and manage, and the treatment is directed at reducing the associated inflammation that is leading to ulceration. The choice of treatment depends on numerous factors, including the location, number, and size of the lesions, extracutaneous involvement, the presence of associated diseases, costs, and the side effects of treatment, as well as the patient’s comorbidities and preferences. The recognition and treatment of underlying diseases, such as inflammatory bowel disease or arthritis, is an important part of management, although a direct relationship between the severity of associated disease and PG remains an issue of debate [3].
A twenty-year-old female had been followed by rheumatology for ten years for severe erosive deforming seropositive rheumatoid arthritis, then on methotrexate 25 mg/week, Salazopyrin 2 g/day, and prednisone 7.5 mg/day. The patient reported the appearance of pustules evolving toward oozing and ulceration fifteen days before the consultation, following a fall from a staircase.
A dermatological examination revealed the presence of three deep well-circumscribed ulcerations on the left leg with a non-raised, erythematous, and purplish border (Fig. 1). An inflammatory laboratory test was positive, without hyperleukocytosis of PNN. A skin biopsy was performed and returned in favor of PG.
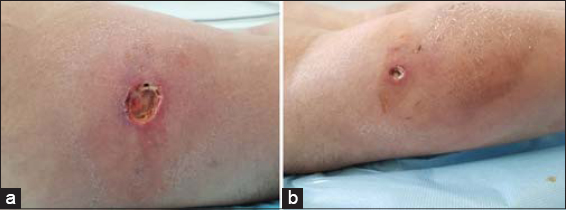 |
Figure 1: (a-b) Deep well-circumscribed ulcerations on the left leg with a non-raised, erythematous, and purplish border. |
Our case is special because of the patient’s young age and the very severe early nature of the rheumatic pathology, which preceded the GP by several years.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Ashchyan HJ, Nelson CA, Stephen S, James WD, Micheletti RG, Rosenbach M. Neutrophilic dermatoses:Pyoderma gangrenosum and other bowel- and arthritis-associated neutrophilic dermatoses. J Am Acad Dermatol. 2018;79:1009-22.
2. Chakiri R, Baybay H, Hatimi AE, Gallouj S, Harmouch T, Mernissi FZ. Clinical and histological patterns and treatment of pyoderma gangrenosum. Pan Afr Med J. 2020;36:59.
3. Alavi A, French LE, Davis MD, Brassard A, Kirsner RS. Pyoderma gangrenosum:An update on pathophysiology, diagnosis and treatment. Am J Clin Dermatol. 2017;18:355-72.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |



Comments are closed.