Eruptive dermatofibromas in a pregnant woman
Dassouli Ryme , Sara Elloudi, Imane Couissi, Hanane Baybay, Zakia Douhi, Fatima Zahra Mernissi
, Sara Elloudi, Imane Couissi, Hanane Baybay, Zakia Douhi, Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Fès, Morocco
Corresponding author: Dassouli Ryme, MD
How to cite this article: Ryme D, Elloudi S, Couissi I, Baybay H, Douhi Z, Mernissi FZ. Eruptive dermatofibromas in a pregnant woman. Our Dermatol Online. 2022;13(e):e11.
Submission: 07.09.2021; Acceptance: 24.01.2022
DOI: 10.7241/ourd.2022e.11
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Dermatofibromas (DF) or benign fibrous histiocytofibromas represent one of the most common skin tumors. It is a soft tissue and bone tumor composed of fibroblastic and histiocytic components without nuclear pleomorphism or histological anaplasia. The eruptive form and the multiple form are 2 subunits of DF that are rare, their pathophysiology and the factors inducing its proliferation remain poorly understood. Autoimmune or neoplastic diseases are incriminated, but hormonal or toxic factors have never been elucidated. the pigmented network and the central whitish appearance is the most prominent dermoscopic pattern in the literature.
Key words: Eruptive dermatofibroma; Dermoscopy; Pregnancy
INTRODUCTION
Histiocytofibromas are frequent benign fibro-histiocytic tumors, most often solitary [1,2] and localized in the lower limbs of young or middle-aged women. Their multiple and eruptive character is rarely described, and they are often associated with dysimmune or neoplastic diseases [3]. We report the exceptional observation of eruptive histiocytofibromas (HCF-E) induced by pregnancy.
CASE REPORT
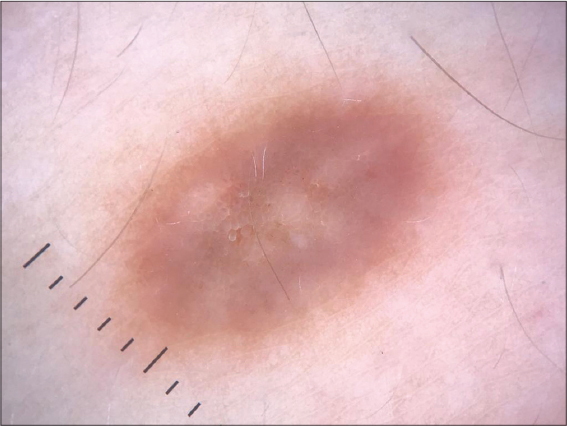
A 28-year-old woman, G2-P1, consulted during the 2nd trimester of her 2nd pregnancy for multiple infiltrated papules of the left lower extremity. The appearance of the first lesions coincided with the second trimester of her first pregnancy 2 years ago, complicated by a polymorphic pregnancy rash and preeclampsia. Their number and size increased throughout the pregnancy, in total one she had installed 5 papules, then remained stable after delivery. Two years later, during a second pregnancy also complicated by pre-eclampsia, the patient noted the development of two new similar lesions on the same limb and an increase in size of the old lesions, without any change in number after the delivery, and this with a 6-month delay. The clinical examination revealed the presence of 7 papules or nodules of 5 to 10 mm in diameter, brownish in color, firm in consistency and with a positive fetus sign when pinched. The lesions were linear on the anterior aspect of the left lower limb (Figs. 1 and 2). Dermoscopic analysis described a homogeneous brownish network with fine and tight meshes for the young lesions (Fig. 3), with a mixed pattern made of peripheral homogeneous brown network with central oval or ring-shaped whitish areas (Fig. 4). Histological examination of one lesion revealed the presence of a poorly limited dermal tumor proliferation composed of thick collagen bundles associated with spindle cells, with hyperplasia of the epidermis opposite, confirming the diagnosis of HCF. No treatment was proposed in the absence of aesthetic discomfort.
DISCUSSION
DFs (histiocytofibromas) are common and benign cutaneous fibro-histiocytic tumors. They are usually solitary lesions, located on the legs or less frequently on the trunk or arms of young adults, most often female, during the second half of life.
Dermoscopic analysis had described a homogeneous brownish network appearance taking the whole lesion of young HSF and a mixed pattern made of peripheral brownish network and oval whitish spots in the center, this pattern represents according to Kellati et all [4] the typical appearance of common fibrous dermatofibromas. It corresponds histologically to a pronounced fibrosis within the papillary dermis with hyperpigmented rete ridges at the edge of the DF [5], and probably develops at an advanced stage of tumor proliferation.
Multiple eruptive DF (MEFD) was first defined by the presence of at least 15 DFs in a single patient by Shapiro et al [6]. Ammirati et al. proposed to extend this definition to the development of more than five lesions in a period of less than four months to reflect the eruptive nature of this condition [7].
Although the number of papules in our patient did not exceed 15 lesions, but the development of more than 5 lesions in a period not exceeding 4 months with rapid growth during pregnancy suggests the eruptive character probably favored by hormonal stimulants.
An associated etiology is present in 70% of cases, most often autoimmune disease, hematological malignancies after administration of immunosuppressive drugs, solid tumors and more rarely during HIV infection or after organ transplantation [3–6].
In our case, the successive development of lesions during the 2 pregnancies, the absence of new lesions at a distance from the deliveries and the absence of overt immunosuppression plead for the inductive role of pregnancy. The development of HCF-E secondary to pregnancy has been reported in only 2 observations [2,3].
The pathophysiology of HCF-E remains unclear. Most of the cases concern women, suggesting a female sexual hormonal factor, in particular a favourable role of estrogens [2–9].
In our observation, the linear character of some lesions and the history of polymorphic pregnancy rash also suggest the role of pruritus in the genesis of the lesions.
During pre-eclampsia, oxidative stress and placental dysfunction release apoptotic flows into the maternal circulation and activate cytokines and certain factors inducing systemic inflammatory response [10]. The occurrence and growth of these lesions in our patient during the 2nd and 3rd trimester incriminates the role of toxins and placental flows in this benign dermal tumor proliferation. Or the systemic inflammatory state that it generates in the mother favors their appearance. More studies are needed to confirm the link between pre-eclampsia and HSF-E.
CONCLUSION
We report the original observation of HCF-E secondary to pregnancies complicated by polymorphic eruption of pregnancy and preeclampsia, suggesting the conjunction of hormonal, mechanical, and toxin predisposing factors.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Deb P, Singh V, Dutta V, Bhatoe HS, Chandran VM. Histiocytome fibreux benin intracranien primitif:a propos d’un cas inhabituel. J Cancer Res Ther. 2014;10:200 –2.
2. Giavedoni P, Combalia A, Pigem R, MascaróJM. Multiple eruptive dermatofibromas in a patient treated with brentuximab vedotin. Actas Dermosifiliogr (Engl Ed). 2019;110:419-20.
3. Pernet C, Dereure O, Guillot B, Bessis D. Histiocytofibromes multiples et éruptifs au cours de la grossesse. Ann Dermatol Vénéréol. 2013;140:S611.
4. Kelati A, Aqil N, Baybay H, Gallouj S, Mernissi FZ. Beyond classic dermoscopic patterns of dermatofibromas:a prospective research study. J Med Case Rep. 2017;11:266.
5. Queirós C, Uva L, Soares de Almeida L, Filipe P. Multiple eruptive dermatofibromas associated with pregnancy- a case and literature review. Dermatol Online J. 2019;25:13030.
6. Ben Rejeb S, Dhaoui A, Ben Ghachem D, Souissi A, Bellil K. Multiple eruptive dermatofibromas occuring in a patient under hemodialysis. Our Dermatol Online. 2016;7:412-4.
7. Zaouak A, Chamli A, Khanchel F, Hammami H, Fenniche S. Multiple eruptive dermatofibromas. Presse Med. 2019;48:1353-4.
8. Wang R, Li G, Nong L, Wang M. Multiple eruptive dermatofibromas aggravated by mycophenolate mofetil and pirfenidone in a patient with systemic sclerosis. Rheumatology (Oxford). 2020;59:4000-1.
9. Shaheen B, Saldanha G, Calonje E, Johnston GA. Multiple clustered dermatofibromas (fibrous histiocytomas):an atypical clinical variant of dermatofibroma. Clin Exp Dermatol. 2014;39:88-90.
10. Lecarpentier E, Fournier T, Guibourdenche J, Tsatsaris V. Physiopathologie de la pré-éclampsie. Presse Méd. 2016;45:631-7.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-4330-4429 http://orcid.org/0000-0003-4330-4429 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 |






Comments are closed.