Painful nail: What is your diagnosis?
Ibtissam Al Faker , Farah Marraha, Salim Gallouj
, Farah Marraha, Salim Gallouj
Department of Dermatology University Hospital Center of Tanger, Tetouan, Al Hoceima Faculty of Medicine and Pharmacy Tangier Abdelmalek Essaadi University Tangier – Morocco
Corresponding author: Ibtissam Al Faker, MD
Submission: 27.04.2021; Acceptance: 04.09.2021
DOI: 10.7241/ourd.2021e.73
Cite this article: Al Faker I, Marraha F, Gallouj S. Painful nail: What is your diagnosis? Our Dermatol Online. 2021;12(e):e73.
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
A glomus tumor is a rare benign neoplasia; which involves a thermoregulatory microvascular system, the glomus body. It is often found in the subungual tissue. Eccrine angiomatous Hamartoma (EAH) is a rare proliferation of vascular and eccrine structures. We present an original case by its location, clinical examination (pain is the main symptom with onycholysis) and its misleading appearance on MRI. The treatment consists of surgical excision of the tumor with good evolution. We will insist on the histological exam of the piece, which is the key to the diagnosis.
Key words: Nail, Hamartoma, Glomus tumor, Sweat glands, Blood vessel
INTRODUCTION
Eccrine angiomatous hamartoma (EAH) is a rare, benign vascular and eccrine malformation. It can be congenital or appear later in childhood as solitary nodules or red, brown, bluish, purplish or even flesh-coloured plaques [1] the preferred location is extremities, face, trunk and scalp; it is usually asymptomatic but signs such as pain, focal hyperhidrosis and hypertrichosis are sometimes associated.
We report a case of EAH with atypical presentation and localization.
OBSERVATION
A 59 years old women woman having as medical history of arterial hypertension and hypercholesterolemia, arrived at our department for an exquisite pain of the right big toe with excessive sweating for 4 months, this pain is exacerbated on palpation with positive love’s sign. The clinical examination of the big toe is unremarkable, both skin and nail, except for a distal onycholysis (Fig. 1). The rest of the clinical exam is normal.
 |
Figure 1: Distal onycholysis with mild hyperkeratosis. |
Dermoscopy shows an erythematous area, yellow line with slight subungual hyperkeratosis (Figs. 2a and 2b).
 |
Figure 2: (a,b) – Dermoscopic aspect: erythematous area, yellow line with slight subungual hyperkeratosis. |
MRI exploration was in favor of tumor proliferation under the medial subungual of the big toe measuring 13 mm long axis, initially suggesting a glomus tumor (Fig. 3).
 |
Figure 3: Big toe MRI (T2) shows tumor proliferation under the medial subungual of the big toe measuring 13 mm long axis. |
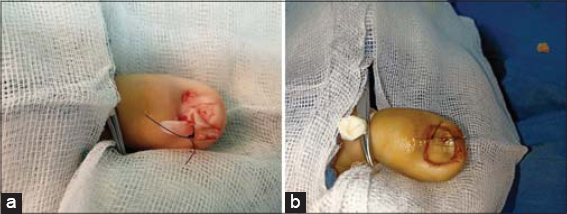
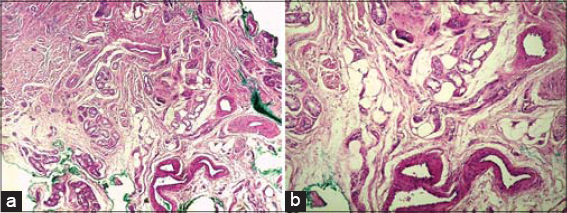
Surgical removal of the tumor (Figs. 4a and 4b) was performed to make an end to pain and to determine the histological nature (Figs. 5a and 5b) of the tumor suspected on MRI; the result was satisfactory and the evolution was marked by the absence of pain (Fig. 6a) and onychomycosis after 1 year (Fig. 6b).
DISCUSSION
EAH is a rare benign skin tumor characterized histologically by the proliferation of eccrine glands and vascular elements. The term EAH was cited by Heyman et al [2] in 1968, but the disease was first described by Lotzbeck in 1859 as an angioma-like tumor on the cheek of a child, which is characterized by numerous eccrine glands and prominent blood vessels [3].
Although it is rare, almost a hundred cases have been reported in the literature [4], EAH usually presents at birth or during early childhood, but currently, it is seen more and more in adolescents and adults.
Some authors have proposed a physio pathological explanation for this disease which considers it as a biochemical fault in the interactions between the differentiated epithelium and the underlying mesenchyme giving rise to an abnormal proliferation of the annexed vascular structures [5]. A second theory explains the occurrence of this disease blames trauma as a causal factor [4].
Clinically, it takes several aspects, the physical examination may show papules, nodules or plaques which gradually increase in size with age and which may vary in color from red to flesh-colored skin; pain, local hyperhidrosis and hypertrichosis help to make a diagnosis of EAH, but they are not always present; in our patient, the exquisite pain was the main reason for her consultation. The lesions are usually single and unilateral, however, a few cases have been reported in the literature with multiple and bilateral lesions [4,6]. Although lesions predominate in the distal extremities and palmoplantar regions, involvement of the face, neck, trunk, abdomen, back and sacral region can be encountered [7].
We report a unique case given its atypical localization, subungual, which, to our knowledge, is described only once a time in the literature but with nodules and destruction of the nail [8], and given the absence of any cutaneous lesion, and finally because it was mimicking a glomus tumor on MRI reason why it was misdiagnosed.
Histologically, EAH houses the middle and deep dermis, it is characterized by numerous hyperplastic lobules of sweat glands and accompanied by vascular proliferation made up of small capillaries and dilated venular vessels. The differential diagnosis includes vascular malformations, telangiectatic macular mastocytosis, glomus tumor, smooth muscle hamartoma, eccrine nevus and sweat angioma [9], the diagnosis is confirmed by pathological exam that must be requested systematically for any operative piece.
EAH usually does not require treatment, however simple surgical removal is recommended for pain, progressive enlargement, excessive hyperhidrosis, or cosmetic reasons. The available effective treatment alternatives are laser, botulinum toxin type A injection and intralesional sclerotherapy [4].
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Pelle MT, Pride HB, Tyler WB. Eccrine angiomatous hamartoma. J Am Acad Dermatol. 2002;47:429-35.
2. Heyman AB, Harris H, Brownstein MH. Eccrine angiomatous hamartoma. NY State J. Med. 1968;68:2803–6.
3. Lotzbeck C. Ein Fall von Schweissdrüsen-geschwulst an der Wange. Virchows Arch Pathol Anat. 1859;16:160.
4. Alexander C, McCarthy EF, Puttgen KB, Deune EG. Bilateral eccrine angiomatous hamartoma with symmetric volar wrist nodules:a case report. JBJS Case Conn. 2019;9:e20.
5. Larralde M, Bazzolo E, Boggio P, Abad ME, SantosMuñoz A. Eccrine angiomatous hamartoma:report of five congenital cases. Pediatr Dermatol. 2009;26:316-9.
6. Verma S, Thakur BK, Mishra J. Eccrine angiomatous hamartoma:multiple, symmetrical swellings on forearms of a 10-year-old girl. Journal of the Eur Acad Dermatol Venereol. 2015;29:1847-8.
7. Lin YT, Chen CM, Yang CH, Chuang YH. Eccrine angiomatous hamartoma:a retrospective study of 15 cases. Chang Gung Med J. 2012;35:167-7.
8. Sezer E, Koseoglu RD, Filiz N. Eccrine angiomatous hamartoma of the fingers with nail destruction. British J Dermatol. 2006;154:1002-4.
9. Lopez V, Pinazo I, Santonja N, Jorda E. Eccrine agiomnatous hamartoma in a child. Pediatr Dermatol. 2010;27:548-9.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-8134-2579 http://orcid.org/0000-0001-8134-2579 http://orcid.org/0000-0002-4465-954X http://orcid.org/0000-0002-4465-954X |




Comments are closed.