Acroangiodermatitis or pseudo-Kaposi’s sarcoma: A challenging diagnosis
Hanan Ragragui Ouasmin 1, Soraya Aouali1, Nada Zizi1,2, Siham Dikhaye1,2
1, Soraya Aouali1, Nada Zizi1,2, Siham Dikhaye1,2
1Department of Dermatology, Venerology and Allergology, Mohammed the VIth University Hospital Center of Oujda, Morocco, 2Laboratory of Epidemiology, Clinical Research and Public Health, Faculty of Medicine and Pharmacy, Mohammed the first university of Oujda, Morocco
Corresponding author: Hanan Ragragui Ouasmin, MD
How to cite this article: Ouasmin HR, Aouali S, Zizi N, Dikhaye S. Acroangiodermatitis or pseudo-Kaposi’s sarcoma: a challenging diagnosis. Our Dermatol Online. 2021;12(e):e72.
Submission: 02.06.2021; Acceptance: 12.08.2021
DOI: 10.7241/ourd.2021e.72
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Acroangiodermatitis (AAD), also referred to as pseudo-Kaposi’s sarcoma, is a vascular-proliferative disease characterized by reactive proliferation of small blood vessels in response to congenital or acquired vascular lesions. There are mainly two clinical variants of acroangiodermatitis; STEWART-BLUEFARB syndrome and the Malian type. There is clinical and histological similarity with Kaposi’s sarcoma hence the interest of immunohistochemical analysis. We report the case of a 40-year-old man with cutaneous lesions localized on the lower limbs. Clinical, dermoscopic, histological and immunohistochemical investigation led to a diagnosis of Kaposi-like acroangiodermatitis.
Key words: Acroangiodermatitis; Pseudo-Kaposi’s sarcoma; Chronic venous insufficiency; Leg ulcer
INTRODUCTION
Acroangiodermatitis (AAD) is a rare angioproliferative disease usually of the lower limb manifesting with cutaneous lesions clinically similar to Kaposi’s sarcoma [1]. It is a benign hyperplasia of preexisting vasculature and may be associated with acquired or congenital arteriovenous malformations (AVM), or severe chronic venous insufficiency [2–3]. The diagnosis relies mainly on histologic findings [4].
CASE REPORT
We report the case of a 40-year-old man with a history of human immunodeficiency virus infection since 2011 under antiretroviral treatment, pulmonary tuberculosis treated in 2011 and 2017 and operated for varicose veins of the left lower limb 2 years ago.
On clinical examination, we noted the presence of confluent purple macular lesions, non-infiltrated, measuring 15 cm for the most voluminous, localized in the foot and the left leg, evolving over the last 3 years. The presence of an ulcer of the internal malleolus of the left foot and venous ectasia were also noted (Figs. 1a – 1c).
 |
Figure 1: Clinical aspect a:Plaques on the left leg suggestive of Kaposi’s sarcoma. b:Ulcer of the internal malleolus of the left foot.c:Venous ectasia of the left foot. |
Dermoscopic examination showed the presence of white rail lines, blue and red lacunae, whitish veil and some hemorrhagic crusts (Figs. 2a and 2b).
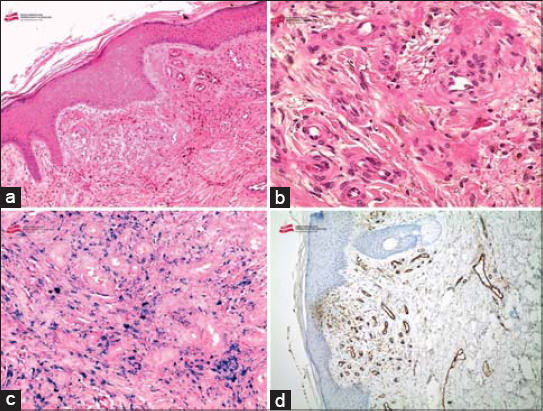
A skin biopsy with immunohistochemistry was performed, showing a dermal proliferation of small vessels, with regular contours, bordered by non-atypical layer of endothelial cells with a layer of pericytes. Extravasation of erythrocytes w as also noted. Immunohistochemistry showed the expression of CD31 antibody (Figs. 3a – 3d).
Examination of arterial and venous vasculature, including Echo-Doppler disclosed no evidence for an underlying arteriovenous malformation.
The patient was then prescribed topical corticosteroids, compression stockings and referred to vascular surgery department for follow-up of chronic venous insufficiency.
DISCUSSION
Acroangiodermatitis is a dermatological condition characterized by purple-colored nodules, plaques or patches, mostly on the extensor surfaces of lower extremities [1]. There are four clinical variants of AAD, the most common type; Mali is associated with venous hypertension; the Stewart-Bluefarb type is associated with congenital arteriovenous malformation (AVM); there is also a less frequent one in patients with chronic renal failure with acquired arteriovenous fistula and a form occurring in pregnant women [3–5].
The aetiology of AAD is not known. Proliferation of fibroblasts and small vessels secondary to high perfusion rate in tissues has been suggested. Another theory is that a PGE1 or heparin like factor, which has angiotensin promoting activity, is responsible for the development of this lesion. A possible role of micro trauma has been suggested by Pleger [1].
Histologically, AAD resembles Kaposi’s sarcoma as both conditions show a proliferation of small blood vessels and fibroblasts, extravasated erythrocytes and haemosiderin deposits within the dermis [1–2].
Dermoscopic features included white rail lines, red and blue lacunae, whitish veil, hemorrhagic crusts, pinkish homogeneous areas and prominent vascularization [4].
Differential diagnosis of acroangiodermatitis includes, first of all, Kaposi sarcoma, although clinical findings of these conditions are similar, there are differences in histologic features [4].
Therapy for acroangiodermatitis includes external compression as the best therapeutic method, in combination with topical antibiotics or topical corticosteroids for early stage lesions. Other therapeutically successful treatment regimens were also described: oral Erythromycin in the dose of 500 mg four times a day or Dapsone in the dose of 50 mg twice a day for 3 months combined with a compression therapy [4,5].
CONCLUSION
Acroangiodermatitis is a rare, benign condition associated with chronic venous insufficiency and may progress to foot ulcers. Appropriate recognition of acroangiodermatitis is important for the disease prognosis in individual patients.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Samad A, Doddos S. Acroangiodermatitis:review of the literature and report of a case associated with symmetrical foot ulcers. Eur J Vasc Endovasc Surg. 2002;24:558-60.
2. LugovićL, PusićJ, Situm M, Buljan M, Bulat V, SebetićK, et al. Acroangiodermatitis (pseudo-Kaposi sarcoma):three case reports. Acta Dermatovenerol Croat. 2007;15:152-7.
3. Archie M, Khademi S, Aungst D, Nouvong A, Freeman S, Gelabert H, et al. A Rare Case of Acroangiodermatitis Associated with a congenital arteriovenous malformation (Stewart–Bluefarb Syndrome) in a young veteran:case report and review of the literature. Ann Vasc Surg. 2015;29:1448.e5-10.
4. Paganelli A, Bassoli S, Roncati L, Bigi L, Ciardo S, Pellacani G. Pseudo Kaposi sarcoma:report of a case investigated by dermoscopy, reflectance confocal microscopy and optical coherence tomography. J Eur Acad Dermatol Venereol. 2018;32:e429-32.
5. Ewelina Rebizak A, Węglowska J, Luczak K. Pseudo-Kaposi sarcoma. Dermatol Rev/Przeg Dermatol. 2018;4:554-7.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-3233-4051 http://orcid.org/0000-0002-3233-4051 http://orcid.org/0000-0001-7687-0158 http://orcid.org/0000-0001-7687-0158 |




Comments are closed.