A case of idiopathic granulomatous vasculitis with phlebitis and underlying subcutaneous necrotizing venulitis
Toshiyuki Yamamoto 1, Reiko Orikasa2, Ko-Ron Chen3
1, Reiko Orikasa2, Ko-Ron Chen3
1Department of Dermatology, Fukushima Medical University, Fukushima, Japan, 2Department of Dermatology, Ohta Nishinouchi General Hospital, Fukushima, Japan, 3Meguro Chen Dermatology Clinic, Tokyo, Japan
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Granulomatous vasculitis in skin lesions is rarely seen in non-infectious granulomatous diseases and other systemic disorders. Herein, we report a unique case of cutaneous vasculitis in which granulomatous phlebitis was observed in a muscular vein at the dermal–subcutaneous junction and necrotizing granulomatous venulitis in the underlying subcutaneous tissues.
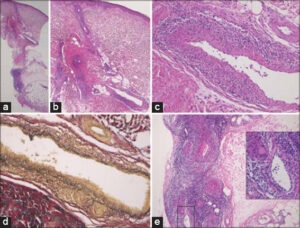
A 74-year-old female was referred to the dermatology clinic at Ota Nishinouchi General Hospital complaining of a painful, ulcerative lesion and numbness of the lower right extremity, which appeared one year earlier. She had hyperlipidemia, yet did not suffer from either diabetes mellitus or thyroiditis. A physical examination revealed an ulcer with an elevated, brownish border and ill-circumscribed, reddish infiltrated erythemas surrounding the concaved healed ulcerative lesion on the right shin (Fig. 1). A biopsy was taken from the erythematous plaque. The histopathological features found revealed degenerated collagen with surrounding vessels in the mid-dermis and a number of infiltrated inflammatory cells around the vessels at the dermal–subcutaneous junction (Figs. 2a and 2b). Higher magnification revealed several multi-nucleated giant cells and infiltration of inflammatory cells in the vascular wall (Fig. 2c). Elastica van Gieson stain confirmed that the vessel was a muscular vein with the partial destruction of the muscular layer, which was consistent with the features of granulomatous phlebitis (Fig. 2d). Naked epithelioid granulomas were additionally observed near granulomatous phlebitis. Immunohistochemistry revealed that histiocytes in and around the affected vessel wall were immunoreactive for CD68. In the subcutaneous tissue, the feature of necrotizing granulomatous venulitis was characterized by marked angiocentric infiltrate of histiocytes in and around the affected vessel wall mixed with neutrophils and lymphocytes and vessel wall fibrinoid necrosis (Fig. 2e). There was no eosinophil infiltration, and a dermal mucin deposition was not detected. On laboratory examination, the eosinophil ratio in the peripheral blood and the serum level of angiotensin-converting enzyme (ACE) were normal, and neither PR3-ANCA nor MPO-ANCA was detected. Ophthalmological and pulmonary examinations excluded sarcoidosis. Tuberculosis was excluded by chest X-ray, a chest CT scan, and a tuberculin test. In addition, the patient had no previous history of inflammatory bowel disease or intestinal symptoms. She was treated with topical difluprednate ointment, and the ulcer was completely epithelialized in three months.
The present case exhibited granulomatous phlebitis with naked epithelioid cell granulomas in the dermal–subcutaneous junction and subcutis. Furthermore, necrotizing granulomatous venulitis with fibrinoid necrosis and a predominantly angiocentric infiltration of histiocytes and giant cells in and around the vessel wall mixed with neutrophils and lymphocytes was observed in the underlying subcutis. Several cutaneous disorders that histologically show granulomatous vasculitis, including granulomatosis with polyangiitis, eosinophilic granulomatosis with polyangiitis, rheumatoid arthritis, giant cell arteritis, Crohn’s disease, granulomatous phlebitis, and the non-infectious granulomatous diseases appearing in pretibial sites such as sarcoidosis and necrobiosis lipoidica, should be differentiated from one another [1–5]. Although this case clinically resembled necrobiosis lipoidica and the histopathological findings of granulomatous phlebitis could also be found in necrobiosis lipoidica [4], the key histopathological findings, such as dermal collagen necrobiosis changes surrounded by histiocytes and giant cells suggesting necrobiosis lipoidica, were absent in this case. Both features of pretibial plaque lesion clinically and subcutaneous naked granuloma with granulomatous vasculitis histopathologically could be found in sarcoidosis [5], yet neither extracutaneous examinations nor serological findings suggesting sarcoidosis were observed. Other systemic disorders such as ANCA-associated granulomatous vasculitis, rheumatoid arthritis, and inflammatory bowel disease were excluded. The examination of tuberculosis revealed no abnormal findings. Thus, none of the possible triggers or associated diseases could be identified in this case. The patient is today under careful follow-up for the appearance of possible associated diseases.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Ackerman AB, Boer A, Bennin B, Gottlieb GJ. Histologic diagnosis of inflammatory skin diseases:an algorithmic method based on pattern analysis. Ardor Scribendi, 3rd Ed. pp425-431, Lea&Febiger, Philadelphia.
2. Sharma A, Dogra S, Sharma K. Granulomatous vasculitis. Dermatol Clin. 2015;33:475-87.
3. Marzano AV, Balice Y, Tavecchio S, Desimine C, Colombo A, Berti E. Granulomatous vasculitis. G Ital Dermatol Venereol. 2015;150:193-202.
4. Yamamoto T, Chen KR. Granulomatous phlebitis in necrobiosis lipoidica. Am J Dermatopathol. 2020;42:307-8.
5. Yamamoto T, Chen KR. Perforating plaque-type pretibial sarcoidosis with granulomatous phlebitis. Am J Dermatopathol. 2020;42:225-6.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-8390-2573 http://orcid.org/0000-0002-8390-2573 |





Comments are closed.