Pigmented eccrine poroma in collision with seborrheic keratosis: Dermoscopic description and histological correlation
Ryme Dassouli 1, Zakia Douhi1, Kenza Tahiri Joutei1, Hanane BayBay1, Sara Elloudi1, Mouna Rimani2, Fatima Zahra Mernissi1
1, Zakia Douhi1, Kenza Tahiri Joutei1, Hanane BayBay1, Sara Elloudi1, Mouna Rimani2, Fatima Zahra Mernissi1
1Department of Dermatology, University Hospital Hassan II, Fes, Morocco, 2Hassan Anatomical Pathology Center – Rabat, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Poromas are rare, benign neoplasms arising from the terminal ductal portion of the sweat glands. They are mainly characterized by flesh-colored or pink papules or nodules, usually located at the extremities. The pigmented variant is rare. Collisions with other benign epithelial tumors have been reported. The clinical appearance may be confused with several benign or malignant tumor pathologies, yet thanks to dermoscopy, which is a non-invasive means of exploration, some signs are highly useful in the diagnosis and in suspecting the collision of two distinct tumors before proceeding to histological confirmation. Herein, we report the original case of a collision between pigmented eccrine poroma of the leg and seborrheic keratosis.
Key words: Pigmented poroma; Collision; Dermoscopy; Histology; Seborrheic keratosis
INTRODUCTION
Poromas were first described in 1956 by Pinkus, Goldman, and Login as tumors of eccrine sweat glands, although there are also reports of exocrine differentiation [1]. It is a rare pathological condition that usually appears between the fourth and sixth decades of life. Further studies on this rare pigmented variant of eccrine poroma may shed new light on the identification of specific dermoscopic features [2]. Collision tumors correspond to the coexistence of two histologically distinct tumors composing a single mass [3]. Herein, we report a tumor composed of pigmented eccrine poroma in collision with seborrheic keratosis.
Case Report
A 62-year-old patient, without a notable pathological antecedent, presented a lesion of the right leg for two years increasing very gradually in size, becoming pruritic and not painful. No notion of trauma or bleeding was reported.
A dermatological examination revealed a pigmented nodule, roughly oval, with irregular contours and a firm consistency, 2 cm in length, located on the external surface of the right leg. The lower half of the lesion was surrounded by a detached epidermal collar on its inner side (Fig. 1).
 |
Figure 1: Pigmented nodule, roughly oval, with irregular contours surrounded by an epidermal collar, 2 cm in length, located on the external aspect of the right leg. |
A dermoscopic examination showed well-circumscribed, milky-red areas surrounded by brownish interlacing, reminding in its globality the aspect of frog eggs, vascular structures within it, poorly visualized with rounded ends, some of which had a globular aspect. There were also bright, whitish streaks in places, grayish-white areas without structure, and scattered, blackish dots and globules. This aspect was in collision with a homogeneous, brownish structure with a coral-like appearance and mordant borders, interspersed by some homogeneous, brownish globules (Fig. 2).
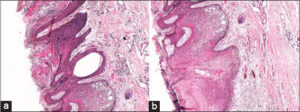
The patient underwent an excisional biopsy. An anatomopathological study was in favor of a collision tumor associating a pigmented eccrine poroma with a hyperkeratotic and pigmented seborrheic keratosis. A microscopic study of the horizontal sections revealed an intraepidermal proliferation with endophytic development realizing wide, tongue-like trabeculae composed of round, monomorphic basaloid cells with focally enlarged nuclei without exaggerated mitotic activity, and thick columns extending and anastomosing at the level of the reticular dermis. The proliferation was rich in melanin pigments. There were also dilated ductular structures lined with cuboid cells with patchy squamous differentiation. The stroma was fibrous and richly vascularized (Figs. 3a and 3b). This lesion collided intimately with a seborrheic keratosis. The borders were non-tumoral. The patient had no recurrence after the excision on two years of follow-up.
DISCUSSION
Eccrine poroma (EP) is a relatively common benign adnexal tumor that accounts for 10% of all sweat gland tumors. EP usually occurs on the soles and lateral surfaces of the feet, which are the sites of a higher concentration of eccrine sweat glands, yet it may also be found on other anatomical sites. It appears more frequently in adults between the fourth and sixth decade of life. Its pathogenesis is unknown, yet may be related to trauma, radiation, or scarring [4].
The pigmented variant of EP often consists of a firm, pigmented nodule with a smooth or keratotic surface, sometimes slightly pedunculated, up to 2 cm in diameter [4,5]. It is frequently confused clinically with seborrheic keratosis, epithelialized pyogenic granuloma, pigmented basal cell carcinoma (BCC), squamous cell carcinoma (SCC), angiofibroma, and cutaneous melanoma [4–6].
Pigmented EP appears to be more common in darker phototypes and in non-acral locations. Indeed, it has been suggested that melanocytes in the palmar and plantar regions show reduced migration, proliferation, and survival activity [7]. Histologically and immunohistochemically, it has been observed that the expression of melanocyte-stimulating factors by tumor cells is associated with melanocyte colonization only by non-acral pigmented poromas [6].
Some articles describe the dermoscopic features of pigmented PE. As the number of published articles is small, specific indices or patterns of non-pigmented PEs have not been established [4,8].
The main dermoscopic clues described in the literature of non-pigmented PE are the following: white, intertwining areas around vessels, areas without a pinkish-white structure, vascular structures composed of irregular glomerular or calyx vessels, hairpin vessels, irregular vessels, and branched vessels with rounded ends [9].
More recently, it has been shown that pigmented eccrine poroma may mimic several benign and malignant tumors also from a dermoscopic point of view [6–9]. Ovoid nests and bluish-gray dots were observed, in addition to tree-like vascular structures. a bluish-white central spot, which may occur in hairpin vessel melanoma in keratinized forms mimicking SKs [10]. In our case, the milky-red lagoons separated by brownish, intertwining, and poorly visualized vascular structures within it made us suspect pigmented eccrine poroma. These structures collided dermoscopically with a clear dermoscopic pattern of seborrheic keratosis with its well-demarcated appearance of bitten borders and coral-like fingerprints. The first diagnosis evoked in our case was pigmented eccrine poroma in collision with a KS, the histopathological study had confirmed our diagnosis.
Dermatopathologically it is a proliferation originating from the lower part of the epidermis from where it extends into the dermis forming large banded anastomoses, composed of epithelial cells of cuboidal appearance connected by intercellular bridges [9–11]. It has been observed that deeper tumors resembled pigmented BCC to a greater extent and that those with hyperkeratosis were similar to KS [10,11]. In our reported case, the grayish-white areas were consistent with hyperkeratosis. The black dots and globules were equivalent to aggregates of melanin pigments intra-epidermally and within the basaloid cells. The bluish-red lacunae were swollen dermal papillae and dilated vascular spaces in the papillary dermis. The brownish intertwining corresponded to the large, tongue-like trabeculae and columns arising from endophytic proliferation from the dermal–epidermal interface extending and anastomosing into the dermis. The whitish streaks corresponded to dermal lamellar fibroplasia [12].
The characteristic feature described was well-circumscribed, reddish lacunae with separation of the mesh bands, reminiscent of frog egg aggregates. This characteristic feature on dermoscopy was explained by the histopathological features observed in the horizontal sections: island-like, edematous stroma containing numerous microvessels embedded in a mass of melanin, pigment-rich poroid cells in a mesh-like pattern forming columns, realizing dermal and dermo-epidermal anastomoses.
The diagnosis of eccrine poroma is routinely reached by histopathology. Because of the diversity of findings, the surgical removal of the lesion is always recommended [7,12].
CONCLUSION
Although the diagnosis of eccrine poroma remains histopathologic, we highlight the role of dermoscopy as a non-invasive means in the diagnosis of poromas as well as its crucial usefulness in the suspicion of a collision with another distinct lesion.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Elboukhari K, El Kadiri S, Benkirane S, Mernissi FZ. Adnexal benign tumor with deroupting dermoscopy. Our Dermatol Online. 2020;11:e87.1-2.
2. Bloom BS, Kamino H, Hale CS, Pomeranz MK. Collision tumor of eccrine poroma, seborrheic keratosis, and a viral wart. Dermatol Online J. 2014;20:13030.
3. Chessa MA, Patrizi A, Baraldi C, Fanti PA, Barisani A, Vaccari S. Dermoscopic-histopathological correlation of eccrine poroma:An observational study. Dermatol Pract Concept. 2019;9:283-91.
4. Bombonato C, Piana S, Moscarella E, Lallas A, Argenziano G, Longo C. Pigmented eccrine poroma:Dermoscopic and confocal features. Dermatol Pract Concept. 2016;6:59-62.
5. Espinosa AE, Ortega BC, Venegas RQ, Ramírez RG. Dermoscopy of non-pigmented eccrine poromas:Study of Mexican cases. Dermatol Pract Concept. 2013;3:25-8.
6. Almeida FC, Cavalcanti SM, Medeiros AC, Teixeira MA. Pigmented eccrine poroma:Report of an atypical case with the use of dermoscopy. An Bras Dermatol. 2013;88:803-6.
7. Lallas A, Chellini PR, Guimarães MG, Cordeiro N, Apalla Z, Longo C, et al. Eccrine poroma:The great dermoscopic imitator. J Eur Acad Dermatol Venereol. 2016;30:e61-3.
8. Marchetti MA, Marino ML, Virmani P, Dusza SW, Marghoob AA, Nazzaro G, et al. Dermoscopic features and patterns of poromas:A multicentre observational case-control study conducted by the International Dermoscopy Society. J Eur Acad Dermatol Venereol. 2018;32:1263-71.
9. Takada T. Diagnostic features of a non-pigmented eccrine poroma with a collarette:Histopathological and dermoscopic correlation. Clin Case Rep. 2021;9:1601-4.
10. Chong Y, Song D-H, Jang K-T, Park KH, Lee EJ. Concurrent occurrence of seborrheic keratosis and melanocytic nevus in the same lesion. Our Dermatol Online. 2014;5:179-82.
11. Zaballos P, Gómez-Martín I, Martin JM, Bañuls J. Dermoscopy of adnexal tumors. Dermatol Clin. 2018;36:397-412.
12. Rafiei R, Eftekhari H, Daryakar A, Nickhah N, Rafiee B. Eccrine porocarcinoma:A case report and brief review of the literature. Our Dermatol Online. 2016;7:391-3.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-4330-4429 http://orcid.org/0000-0003-4330-4429 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |





Comments are closed.