The role of peripheral arterial occlusive disease in the healing of venous ulcers
Blagoja Vasilev1, Mirela Vasileva 2, Stojka Vasileva2
2, Stojka Vasileva2
1Cardiology Department, Clinical Hospital Shtip, North Macedonia, 2Dermatovenerology Department, Clinical Hospital Shtip, North Macedonia
Corresponding author: Mirela Vasileva, MD, PhD
Submission: 18.02.2022; Acceptance: 04.04.2022
DOI: 10.7241/ourd.20223.8
Cite this article: Vasilev B, Vasileva M, Vasileva S. The role of peripheral arterial occlusive disease in the healing of venous ulcers. Our Dermatol Online. 2022;13(3):280-282.
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: The biggest challenge in patients with chronic venous insufficiency is venous ulcers that occur in stage 6 of the CEAP classification. In general, acute ulcers have a 71–80% chance of healing, while chronic ulcers only have a 22% chance of healing. Our clinical practice has shown that patients diagnosed with peripheral arterial occlusive disease have a much longer duration of the disease and a more difficult treatment of venous ulcers than patients with normal arterial circulation.
Materials and Methods: The study included 105 patients with CVI and a developed leg ulcer. Among these, twenty patients were diagnosed with peripheral arterial occlusive disease. All patients were followed for more than twelve weeks.
Results: Peripheral arterial occlusive disease was significantly more common in patients with delayed healing than in patients with normal venous ulcer healing: 18 (30%) vs. 2 (4.4%). for twelve weeks or longer, and it was statistically significant for p = 0.00097.
Conclusion: Peripheral arterial occlusive disease has been shown to be an important indicator of venous epithelial wound healing. The establishment of good arterial circulation is closely related to the course of treatment of chronic venous ulcers.
Key words: ulcers; peripheral arterial disease; venous insufficiency
INTRODUCTION
By changing the body position from horizontal to vertical, blood flow through the legs increases from 8% to 23%. The establishment of new physical and hemodynamic conditions in the blood vessels of the legs are the main factors for the appearance of varicose veins [1–3].
Chronic venous insufficiency (CVI) is highly common nowadays and belongs to the group of diseases considered the most widespread. The frequency of CVI is quite controversial, according to several studies in which different data is presented. Thus, it may be said that it is present in 5–25% of the population depending on which part of the world is concerned [4–6].
The biggest challenge in patients with CVI is venous ulcers that occur in stage 6 of the CEAP classification. The problem with venous ulcers is the frequent resistance to therapy and the transition to chronic [7,8]. These ulcers may last for years and significantly reduce the quality of life of the patient [9,10]. Today, there is a number of studies seeking to find the factor that leads to the emergence of treatment resistance and novel types of solutions.
In general, acute ulcers (lasting three months or less) have a 71–80% chance of healing, while chronic ulcers only have a 22% chance of healing after six months of treatment [11,12]. Patients resistant to conservative therapies need to undergo the surgical treatment of their venous ulcers. Wound debridement has long been employed to improve the condition and facilitate healing. During the procedure, a curette or scissors may be used for sharp debridement, or it may be enzymatic, mechanical, autolytic, or biological with larvae, which is the least commonly employed type of ulcer treatment.
Most necrotic tissue wounds should be evaluated for arterial failure as venous ulcers rarely require much debridement [13].
Our clinical practice has shown that patients diagnosed with peripheral arterial occlusive disease have a much longer duration of the disease and a more difficult treatment of venous ulcers than patients with normal arterial circulation.
MATERIALS AND METHODS
The study included 105 patients with CVI and a developed leg ulcer. Among these, twenty patients were diagnosed with peripheral arterial occlusive disease. All patients were followed for more than twelve weeks. The patients were divided into two groups according to the duration of the venous ulcer: normal wound closure up to twelve weeks and a duration longer than twelve weeks.
All patients underwent the same type of therapy consisting of wound dressing, venotonics, and compression therapy in patients not diagnosed with peripheral arterial occlusive disease.
RESULTS
Peripheral arterial occlusive disease was significantly more common in patients with delayed healing than in patients with normal venous ulcer healing – 18 (30%) vs 2 (4.4%). of 12 weeks or 12 weeks and longer, and it was statistically significant for p = 0.00097 (Table 1); (Fig. 1).
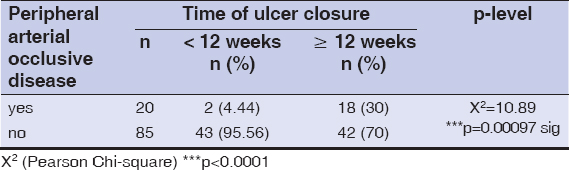 |
Table 1: Normal and delayed ulcer healing: distribution. |
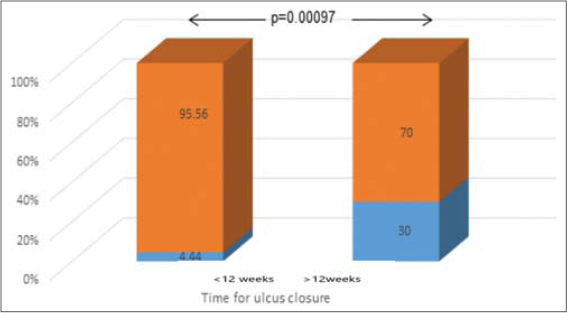 |
Figure 1: Frequency of peripheral arterial occlusive disease in patients with normal and delayed ulcer healing. |
With peripheral arterial occlusive disease, ulcer closure took between four to twelve weeks in two (7.7%) patients and twelve weeks or more in eighteen (30%) patients. Patients with ulcer closure shorter than four weeks did not have peripheral arterial occlusive disease. The test difference in the distribution of the patients with and without peripheral arterial occlusive disease was confirmed as statistically significant between the groups with rapidly delayed venous ulcer healing (p = 0.0066) and between the groups with normal and delayed healing (p = 0.025). The patients with delayed venous ulcer healing were significantly more likely to have peripheral arterial occlusive disease when compared to patients with rapid and normal healing. (Table 2) (Fig. 2).
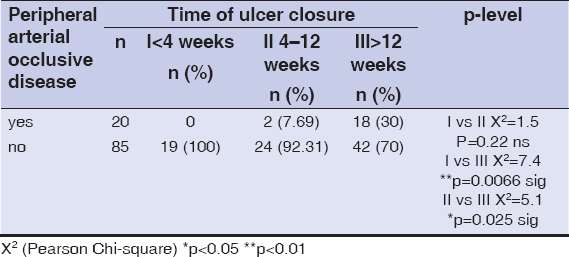 |
Table 2: Rapid, normal, and delayed ulcer healing: distribution according to peripheral arterial occlusive disease |
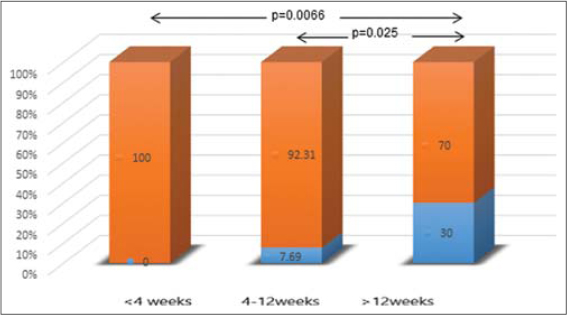 |
Figure 2: Frequency of peripheral arterial occlusive disease in patients with rapid, normal, and delayed ulcer healing. |
DISCUSSION
No patients diagnosed with peripheral arterial occlusive disease were observed in the group of rapidly closing ulcers up to four weeks after the beginning of treatment. The use of pentoxifylline in these patients has been shown to be reasonable and with a high degree of acceleration in the healing process of venous ulcers [14,15]. The absence of peripheral arterial occlusive disease and chronic leg wounds accelerates wound healing and significantly reduces the chances of amputation in patients with the disease present, as opposed to those with normal arterial circulation. This shows us the importance of simultaneous treatment of diseases and early taking of therapeutic measures to solve circulatory problems.
CONCLUSION
Peripheral arterial occlusive disease has been shown to be an important indicator of venous epithelial wound healing. Delayed wound healing affects the quality of life of these patients, given the need for long-term hospitalizations and the inability to perform daily responsibilities normally. Patients are also financially affected, given the cost of treatment and daily dressings. Peripheral arterial occlusive disease has been shown to be an important predictive factor in the duration of venous ulcers. The simultaneous treatment of both diseases is especially important. The establishment of good arterial circulation is closely related to the course of treatment of chronic venous ulcers. Improving circulation also means faster granulation of the wound, so it is especially important for these patients to be given a multidisciplinary approach to problem-solving.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Recek C. Calf pump activity influencing venous hemodynamics in the lower extremity. Int J Angiol. 2013;22:23-30.
2. Franz A, Berndt F, Raabe J, Harmsen JF, Zilkens C, Behringer M. Invasive assessment of hemodynamic, metabolic and ionic consequences during blood flow restriction training. Front Physiol. 2020;11:617668.
3. Youn YJ, Lee J. Chronic venous insufficiency and varicose veins of the lower extremities. Korean J Intern Med. 2019;34:269-83.
4. Lohr JM, Bush RL. Venous disease in women:Epidemiology, manifestations, and treatment. J Vasc Surg. 2013;57:37S-45S.
5. Kirsten N, Mohr N, Gensel F, Alhumam A, Bruning G, Augustin M. Population-based epidemiologic study in venous diseases in Germany:Prevalence, comorbidity, and medical needs in a cohort of 19,104 workers. Vasc Health Risk Manag. 2021;17:679-87.
6. Elamrawy S, Darwish I, Moustafa S, Elshaer N, Ahmed N. Epidemiological, life style, and occupational factors associated with lower limb varicose veins:A case control study. J Egypt Public Health Assoc. 2021;6;96.
7. Raffetto JD. Pathophysiology of wound healing and alterations in venous leg ulcers-review. Phlebology. 2016;31:56-62.
8. Mansilha A, Sousa J. Pathophysiological mechanisms of chronic venous disease and implications for venoactive drug therapy. Int J Mol Sci. 2018;19:1669.
9. Szewczyk MT, Mościcka P, JawieńA, Cwajda-Białasik J, Cierzniakowska K, Ślusarz R, et al. Quality of life in patients with leg ulcers or skin lesions:A pilot study. Postepy Dermatol Alergol. 2015;32:465-9.
10. Vishwanath V. Quality of life:Venous leg ulcers. Indian Dermatol Online J. 2014;5:397-9.
11. Kranke P, Bennett MH, Martyn-St James M, Schnabel A, Debus SE, Weibel S. Hyperbaric oxygen therapy for chronic wounds. Cochrane Database Syst Rev. 2015;2015:CD004123.
12. Raffetto JD, Ligi D, Maniscalco R, Khalil RA, Mannello F. Why venous leg ulcers have difficulty healing:Overview on pathophysiology, clinical consequences, and treatment. J Clin Med. 2020;10:29.
13. Manna B, Nahirniak P, Morrison CA. Wound Debridement. 2021 Sep 6. In:StatPearls [Internet]. Treasure Island (FL):StatPearls Publishing;2022. PMID:29939659.
14. de Oliveira Carvalho PE, Magolbo NG, De Aquino RF, Weller CD. Oral aspirin for treating venous leg ulcers. Cochrane Database Syst Rev. 2016;2:CD009432.
15. Jull AB, Arroll B, Parag V, Waters J. Pentoxifylline for treating venous leg ulcers. Cochrane Database Syst Rev. 2012;12:CD001733.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-6807-5557 http://orcid.org/0000-0002-6807-5557 |



Comments are closed.