Leser–Trélat syndrome: What does it hide?
Dassouli Ryme , Zakia Douhi, Kenza Tahri, Hanane Baybay, Sara Elloudi, Fatima Zahra Mernissi
, Zakia Douhi, Kenza Tahri, Hanane Baybay, Sara Elloudi, Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Corresponding author: Dassouli Ryme, MD
Submission: 07.09.2021; Acceptance: 05.05.2022
DOI: 10.7241/ourd.20223.30
Cite this article: Ryme D, Douhi Z, Tahri K, Baybay H, Elloudi S, Mernissi FZ. Leser–Trélat syndrome: What does it hide? Our Dermatol Online. 2022;13(3):336-337
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Seborrheic keratoses (SKs) are common, benign, non-melanocytic epidermal tumors [1]. Still, they may be suspicious of other, more serious underlying conditions.
Leser–Trélat syndrome may be considered a paraneoplastic condition characterized by the sudden onset of multiple SKs [2]. Herein, we report two cases of malignancy revealed by eruptive KS.
The first case, an 83-year-old male with no notable pathological history, presented for two years with rapidly evolving lesions of the trunk over a six-month period. The patient also noticed for three months melena with transit disorders, justifying a consultation in which the diagnosis of sigmoid tumor was reached and the patient was referred for surgery.
A clinical examination revealed multiple, sessile, exophytic tumors of round or oval appearance, 1 to 3 cm in diameter, well-delimited. The surface of the lesions was verrucous, brownish-black, with numerous, black, keratotic plugs (Fig. 1a). A dermoscopic examination revealed a cerebral appearance with pseudocysts and pseudocomedones (Fig. 1b). The diagnosis of seborrheic keratosis was thus reached.
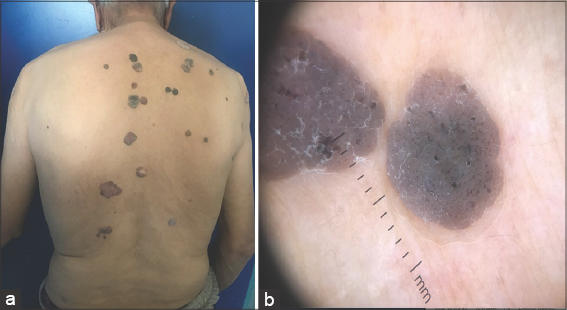 |
Figure 1: (a)Tumors with a round or oval appearance, well-defined, localized on the trunk. (b) Cerebral aspect with pseudocysts and pseudocomedones. |
The second case was an 84-year-old male, a chronic smoker, who was hospitalized at the oncology department for a squamous cell carcinoma of the lung, which had been evolving for one year and which had been treated with carboplatin and paclitaxel. The patient consulted for pruritic lesions of the trunk that appeared two years previously with rapid growth and extension.
A dermatological examination revealed multiple, brownish, exophytic plaques and tumors with sessile bases, round or oval in appearance, ranging in size from 0.5 to 4 cm, scattered on the trunk, axillary region, and face (Fig. 2). Dermoscopy found brownish lesions with a cerebral appearance and good border demarcation, pseudocysts and pseudocomedones, and a coral-like appearance. These were multiple seborrheic keratoses in a subject with pulmonary neoplasia. The diagnosis of Leser–Trélat syndrome was retained, although the patient was unwilling to treat the lesions.
 |
Figure 2: Multiple, brownish papules and plaques on the face and trunk. |
The Leser–Trélat sign (LTS) is considered a relatively rare paraneoplastic skin marker of internal malignancy. To date, there have been no standardized or quantified diagnostic criteria defining the Leser–Trélat sign, yet the familiar definition includes an increase in the number and/or size of seborrheic keratoses (SKs) [3].
SKs primarily affect the chest and back, followed by the extremities, face, abdomen, neck, and axilla. Pruritus and inflammation are common [4].
The LTS is most frequently associated with adenocarcinomas (gastrointestinal in 32% of cases), followed by lymphoproliferative disorders in 20% and, more rarely, with carcinomas of the breast, lung, liver, kidney, prostate, ovary, and nasopharynx [5]. In addition, mycosis fungoides, Sézary syndrome, and plasmacytoma have been described in association with this paraneoplastic disorder [6].
The exact underlying pathogenesis remains unknown. More recent observations have shown a correlation between the release of TGF-alpha and EGF from malignant cells and the rapid proliferation of keratinocytes in the lesional syndrome [7].
A careful search for an underlying malignancy should be undertaken. A physical examination with a complete blood count, serum biochemistry, chest X-ray, mammogram, Pap smear, PSA screening, upper GI endoscopy, and colonoscopy is required during this examination [5–7].
Curettage is the first choice of treatment. After the removal of the internal neoplasm, the regression of seborrheic keratoses is observed [7].
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Karadag AS, Parish LC. The status of the seborrheic keratosis. Clin Dermatol. 2018;36:275-7.
2. Silva JA, Mesquita Kde C, Igreja AC, Lucas IC, Freitas AF, Oliveira SM, et al. Paraneoplastic cutaneous manifestations:Concepts and updates. An Bras Dermatol. 2013;88:9-22.
3. Gori N, Esposito I, Del Regno L, D’Amore A, Peris K, Di Stefani A. Leser–Trélat sign as a rare manifestation of cutaneous melanoma. Dermatol Reports. 2020;12:?.
4. Bernett CN, Schmieder GJ. Leser–Trélat sign. Trasure Island (FL):StatPearls;2020.
5. Wollina U. Recent advances in managing and understanding seborrheic keratosis. F1000Res. 2019;8:F1000.
6. Narala S, Cohen PR. Cutaneous T-cell lymphoma-associated Leser–Trélat sign:Report and world literature review. Dermatol Online J. 2017;23:13030/qt0w01b1t3.
7. Asri H, Soualhi M. The sign of Leser–Tre-lat:Think in the adenocarcinoma of the lung. Pan Afr Med J. 2018;30:270.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-4330-4429 http://orcid.org/0000-0003-4330-4429 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |



Comments are closed.