Secondary syphilis mimicking psoriasis vulgaris on the buttock
Ngo Binh Trinh , Giang Huong Tran
, Giang Huong Tran
1Department of Venereology, Ho Chi Minh City Hospital of Dermato-Venereology, Vietnam, 2Department of Pathology, University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam
Corresponding author: Ngo Binh Trinh, MD
Submission: 17.01.2022; Acceptance: 05.04.2022
DOI: 10.7241/ourd.20223.25
Cite this article: Trinh NB, Tran GH. Secondary syphilis mimicking psoriasis vulgaris on the buttock. Our Dermatol Online. 2022;13(3):326-327.
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Secondary syphilis is caused by Treponema pallidum, classically characterized by a diffuse, symmetric macular or papular eruption involving the entire trunk and extremities [1]. We, herein, describe a case of secondary syphilis mimicking psoriasis vulgaris in an unusual location and with specific histologic hallmarks.
A 28-year-old homosexual male presented with asymptomatic, erythematous patches of the buttock, which were misdiagnosed as psoriasis vulgaris for one month. He reported a history of sexual contact with an anonymous male four months prior to presentation. A clinical examination revealed multiple, well-defined, erythematous, scaling patches on the buttock (Fig. 1a). He had no regional lymphadenopathy. Other mucocutaneous manifestations were undetectable.
| Figure 1: Secondary syphilis on the buttock: (a) before treatment, (b) three months after treatment. |
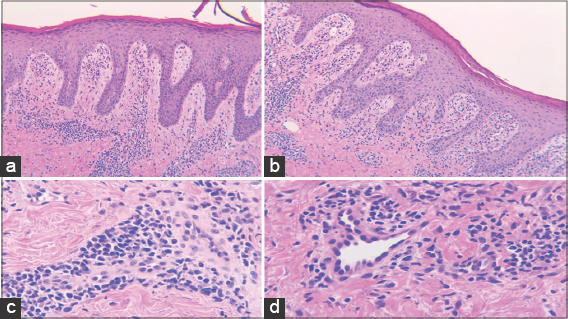
A laboratory evaluation yielded a reactive rapid plasma reagin (RPR) test with a dilution of 1:32 and positive Treponema pallidum hemagglutination (TPHA). Fungal microscopy of the buttock was negative. HIV antibody was negative. A biopsy of the lesion revealed psoriasiform epidermal hyperplasia, an elongated rete, a diffuse perivascular and interstitial dermal infiltrate of plasma cells, lymphocytes, and histiocytes (Figs. 2a and 2b). High power view of the inflammatory infiltrate revealed numerous plasma cells and epithelial swelling (Figs. 2c and 2d). No additional stains were performed due to the unavailability of stains. The histologic, clinical, and laboratory findings confirmed the diagnosis of secondary syphilis. A single dose of benzathine penicillin G at 2.4 million units was injected intramuscularly. Three months later, the RPR titer turned negative and the skin lesions resolved (Fig. 1b).
Psoriasiform rash is an atypical clinical manifestation of early secondary syphilis, which usually appears on the hand and feet [1,2]. Therefore, lesions as in our patient is rare.
The treatment of secondary syphilis is benzathine penicillin G 2.4 million units. Alternative treatment regimens include with tetracycline hydrochloride and erythromycin [1,3].
The differential diagnosis of psoriasiform secondary syphilis includes psoriasis vulgaris, lichen planus, and dermatophyte infection [4]. Psoriasis vulgaris is characterized by erythematous plaques with thickened, shiny scales on the elbows, knees, palms, and soles, especially positive Auspitz’s sign. Therefore, psoriasis vulgaris was excluded due to the negativity of Auspitz’s sign and the unusual location of the lesions. Lichen planus is histologically characterized by a band-like lymphocytic infiltration at the dermal–epidermal junction and a lack of plasma cells. A significant amount of plasma cells on the histological finding and the positive results for syphilis were found in our patient, thus lichen planus was excluded. Fungal microscopy was negative and the diagnosis of dermatophyte infection was also excluded. Based on a previous history of homosexual contact, clinical lesions, serological tests, and a good response to benzathine penicillin G treatment, we confirmed the diagnosis of secondary syphilis.
A psoriasiform lesion is a rare manifestation of secondary syphilis, which may be misdiagnosed with other skin disorders.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Cather JC, Cather JC, Menter MA. Psoriasiform lesions on trunk and palms. Proc (Bayl Univ Med Cent). 2003;16:236-8.
2. LleóMI, Escribano PC, Prieto BM. Atypical cutaneous manifestations in syphilis. Actas Dermo-Sifiliog. 2016;107:275-83.
3. Krishnan A, Samayam A, Patra AK. Syphilis:Case series. Our Dermatol Online. 2019;10:286-8.
4. Tamer F. Remember the great imitator 'syphilis’in oral lesions. Our Dermatol Online. 2018;9:397-8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-3829-3115 http://orcid.org/0000-0002-3829-3115 |




Comments are closed.