Cutaneous B-cell lymphoma mimicking a keloid: Dermoscopy-assisted diagnosis
Uzair Khursheed Dar 1, Yasmeen Jabeen Bhat1, Rohi Wani2
1, Yasmeen Jabeen Bhat1, Rohi Wani2
1Department of Dermatology, Venereology and Leprosy, Govt. Medical College Srinagar, J & K, India, 2Department of Pathology, Govt. Medical College Srinagar, J & K, India.
Corresponding author: Uzair Khursheed Dar, MD
Submission: 19.12.2021; Acceptance: 03.03.2022
DOI: 10.7241/ourd.20223.12
Cite this article: Dar UK, Bhat YJ, Wani R. Cutaneous B-cell lymphoma mimicking a keloid: Dermoscopy-assisted diagnosis. Our Dermatol Online. 2022;13(3):293-295.
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Primary cutaneous lymphomas are lymphoproliferative disorders having multiple heterogenous subtypes with a primary cutaneous manifestation in the absence of systemic involvement of the lymph nodes, bone marrow, or visceral organs at the time of diagnosis. Herein, we report the case of a 75-year-old male who presented with a single plaque on the back mimicking a keloid. Clinical and dermoscopic examinations led to the suspicion of a cutaneous malignancy, while histopathology and IHC confirmed a primary cutaneous B-cell non-Hodgkin’s lymphoma. The lesion responded well to a R-CHOP chemotherapy regimen.
Key words: Skin cancer; Keloid; Dermoscopy
INTRODUCTION
Cutaneous lymphomas are a distinct subset of non-Hodgkin’s lymphomas. They are cancers of the lymphocytes primarily involving the skin. The skin is the most common site of extranodal involvement, after the gastrointestinal tract, in non-Hodgkin’s lymphomas [1].
Classification is based on the type of lymphocyte: B-lymphocyte (B-cell) or T-lymphocyte (T-cell). Cutaneous T-cell lymphoma (CTCL) is the most common type of cutaneous lymphoma, typically presenting with red, scaly patches or thickened plaques of skin that often mimic eczema or chronic dermatitis. B-cell lymphoma is much less common and accounts for 20–25% of cases [2]. Primary cutaneous B-cell lymphomas (PCBCLs) are B-cell lymphomas that originate in the skin and are present at the time of diagnosis without evidence of extracutaneous disease [3].
There are three types of primary cutaneous B-cell lymphoma: primary cutaneous marginal zone lymphoma (pcMZL), primary cutaneous follicle center lymphoma (pcFCL), and primary cutaneous diffuse large B-cell lymphoma (pcDLBCL) [4]. Classically, pcMZL presents as solitary or clustered deep-seated, red-to-violaceous, indurated plaques, nodules, or tumors. pcFCL is characterized by slow-growing, 2–5 cm in diameter, firm, smooth, erythematous-to-violaceous plaques, nodules, or tumors that rarely ulcerate and often have telangiectasias. pcDLBCL commonly presents as 2–5 cm erythematous-to-violaceous tumors or nodules on the leg, with 10–15% on non-leg locations [5].
CASE REPORT
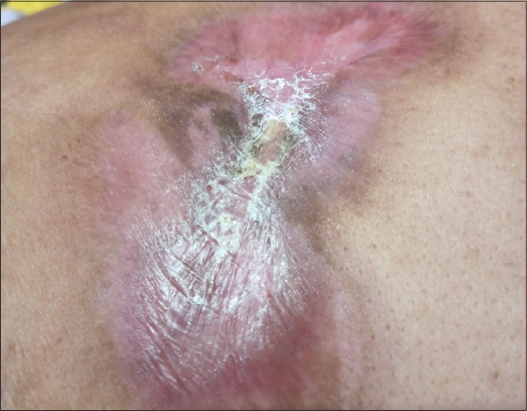
A 75-year-old male with a medical history of type 2 diabetes mellitus and hypertension presented with a single, oval, reddish plaque, 11 × 10 cm in size, on the upper right back present for two months (Fig. 1a). It started as a papule and rapidly progressed in size over one month. The patient had no other symptoms, and general and systemic examinations revealed no abnormalities. The plaque was non-tender, firm in consistency, and was not fixed to the underlying structures. Dermoscopy was performed and showed a salmon-colored background with prominent, large, and serpentine vessels (Fig. 1b). An edge biopsy was taken from the lesion following the initial dermoscopic examination. The lesion ulcerated after several days of taking the biopsy, which favored the diagnosis of B-cell lymphoma (Fig. 1c). A further dermoscopic examination of the margins revealed multiple pseudopod vessels (spermatozoa-shaped) (Fig. 1d).
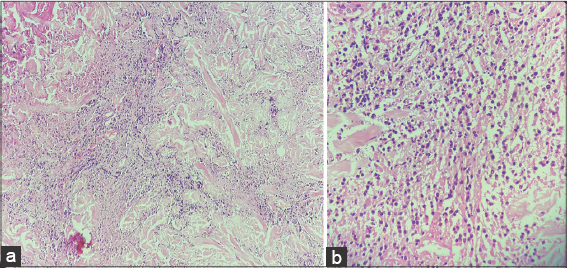
Hematological and biochemical investigations were within normal limits. Ultrasonography of the abdomen and pelvis was unremarkable. Histopathology of the biopsy revealed diffuse infiltration of the dermis by atypical cells with pleomorphic nuclei, coarse chromatin, and conspicuous nuclei with areas of necrosis and ulceration. Spongiosis, parakeratosis, and increased collagenization were present on microscopic examination (Figs. 2a and 2b). Immunohistochemistry revealed atypical cells that tested positive for LCA and CD20 and negative for CD3, TdT, Cyclin D1, CD10, and CD43. Whole-body PET-CT failed to show any extracutaneous involvement, and a diagnosis of high-grade primary cutaneous B-cell lymphoma was reached, following which the patient was initiated on a systemic R-CHOP chemotherapy regimen, to which the lesion responded (Fig. 3).
DISCUSSION
Primary cutaneous B-cell lymphoma is characterized by clonal proliferation of B-cells primarily involving the skin. The absence of extracutaneous disease is a necessary condition for the diagnosis of PCBCL to be confirmed after a six-month follow-up to exclude a nodal non-Hodgkin’s lymphoma (NHL) with secondary cutaneous involvement [6]. The differential diagnosis includes metastasis of small cell carcinoma, Merkel cell carcinoma, sarcoma, and pseudolymphoma. On dermoscopy, Merkel cell carcinomas show a polymorphic vascular pattern, composed of milky-red clods and areas in association with one or more additional vascular structures, such as serpentine or arborizing vessels [7]. Cutaneous sarcomas may present with a total delicate pigment network with the variable presence of multiple hypopigmented areas in piloleiomyomas, a pinkish-red tumor with vessels, white structures, the absence of ulceration in angioleiomyomas, an asymmetric, multilobulated tumor with linear-irregular or polymorphic-atypical vessels, and white structures in leiomyosarcomas [8]. Cutaneous band T-cell lymphomas, as well as pseudolymphomas, may look alike under dermoscopy [9].
Morphology and IHC aid in the diagnosis. In this case, we came across a tumor mimicking a keloid, yet a detailed history and clinical and dermoscopic examinations made us suspect this to be a case of cutaneous malignancy, which was confirmed by histopathological examination and IHC.
CONCLUSION
The aim of reporting this case was to present a rarely found cutaneous malignancy with high chances of a wrong diagnosis and incorrect treatment if dermoscopy does not assist in the suspicion, which became confirmed by histopathological and immunohistochemical findings.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Slimani Y, Hali F, El Fatoiki F-Z, Skali HD, Beliamime I, Marnissi F, et al. Triple-negative diffuse large B-cell lymphoma:A distinct entity. Our Dermatol Online. 2021;12:427-9.
2. Mishra S, Shelly D, VinuBalraam KV, Bharadwaj R. Primary Cutaneous B-cell lymphomas:Case report of two cases. Indian J Dermatol. 2017;62:675.
3. Di Martino Ortiz B, Riveros R, Rodríguez L, Aguilar S, Rodríguez M, Knopfelmacher O, et al. [Diffuse primary B-cell lymphoma of large B-cell, leg-type. A case report]. Our Dermatol Online. 2019;10:151-5.
4. Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375-90.
5. Goyal A, LeBlanc RE, Carter JB. Cutaneous B-cell lymphoma. Hematol Oncol Clin North Am. 2019;33:149-61.
6. Selva RL, Violetti SA, Delfino C, Grandi V, Cicchelli S, Tomasini C, et al. A literature revision in primary cutaneous B-cell lymphoma. Indian J Dermatol. 2017;62:146-57.
7. Elloudi S, Mernissi FZ. Dermoscopic appearance of a rare localization of Merckel carcinoma. Our Dermatol Online. 2021;12:e68.
8. Zaballos P, del Pozo L, Argenziano G, Medina C, Lacarrubba F, Ferrer B. Dermoscopy of cutaneous smooth muscleneoplasms:A morphological study of 136 cases. J Eur Acad Dermatol Venereol. 2019;33:693-9.
9. Geller S, Navarrete-Dechent C, Myskowski PL. Dermoscopy in lymphoproliferative disorders-experience from a cutaneous lymphoma clinic in a tertiary cancer center. J Am Acad Dermatol. 2019;80:e171-2.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.