The role of patch and photopatch tests in facial melanoses: A cross-sectional, observational study
Kaur Sachdeep , Kaur Tejinder, Malhotra Suresh Kumar
, Kaur Tejinder, Malhotra Suresh Kumar
Department of Dermatology,Venereology and Leprosy, Government Medical College, Amritsar, India
Corresponding author: Kaur Sachdeep, MD
How to cite this article: Sachdeep K, Tejinder K, Suresh K. The role of patch and photopatch tests in facial melanoses: A cross-sectional, observational study. Our Dermatol Online. 2022;13(2):132-137.
Submission: 28.11.2021; Acceptance: 08.02.2022
DOI: 10.7241/ourd.20222.3
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Facial pigmentation includes various entities such as melasma, lichen planus pigmentosus (LPP), and pigmented contact dermatitis. The pathogenesis may involve certain allergens, which may be responsible for causing a disturbance in the dermoepidermal junction. The elimination of such inciting allergens may aid in the successful treatment of these patients.
Objective: The aim was to detect contact allergens with patch and photopatch testing in facial pigmentary disorders.
Methods: Fifty patients with facial pigmentary disorders were enrolled. After taking a demographic profile and detailed clinical history and performing an examination, patch and photopatch testing was done using a common suspected allergen series.
Results: Out of the fifty patients tested, 28 (56%) showed a positive patch test, while 2 (4%) showed a positive photopatch test. The most common allergen found was a fragrance mix in 17 (34%) patients, followed by paraphenylenediamine (PPD) in 11 (22%). Other allergens showing positivity were nickel sulfate, benzocaine, parthenium, benzophenone-3, octyl methoxycinnamate, etc.
Conclusion: Patients with facial pigmentation may have an underlying component of contact dermatitis, which may be a causative or aggravating factor. The avoidance of these allergens may help in increasing the efficacy of treatment in these patients.
Key words: Patch testing; Photopatch testing; Melasma; Lichen planus pigmentosus; Pigmented contact dermatitis
INTRODUCTION
Facial hyperpigmentation has always been a significant therapeutic challenge. Melasma is the most common cause, others being ashy dermatosis, Riehl’s melanosis, lichen planus pigmentosus, drug-induced, post-inflammatory hyperpigmentation, etc. Most of these conditions are inflammatory, causing a disturbance in the dermoepidermal junction, leading to the deposition of melanin in the dermis. This points toward the role of some allergens in the pathogenesis. Ultraviolet light in sunrays may interact with certain chemicals such as sunscreens and cosmetics to form allergens and provoke a delayed type of hypersensitivity. All these mechanisms may lead to clinically visible hyperpigmentation. Patch testing and photopatch testing form the cornerstone of the diagnosis of contact and photocontact allergies. In this study, we utilized both of these techniques and attempted to find the common allergens that may have a causative or aggravating influence on facial pigmentation.
MATERIALS AND METHODS
For the present study, fifty cases of facial hyperpigmentation presenting to the outpatient department of a tertiary-care hospital were enrolled. The study period was over two years. The diagnosis was based on the clinical appearance of lesions and was provisional. Malar, centrofacial, or mandibular pigmentation (brown or gray) was diagnosed as melasma. The involvement of the forehead and the preauricular and neck areas with brown or dark brown pigmentation with a history suggestive of some allergen exposure on or near the face was classified as pigmented contact dermatitis. The involvement of the face, neck, and extrafacial sites such as the arms and back with grayish to violaceous hues of pigmentation were diagnosed as lichen planus pigmentosus. A history suggestive of an inflammatory event preceding the onset of pigmentation was diagnosed as post-inflammatory pigmentation. Patient selection was non-consecutive and was performed according to the following criteria. Patients with facial pigmentation and an age above eighteen years were included. Pregnant or breastfeeding females and patients with extensive eczema on the back, on oral steroids (> 15–20 mg daily) or immunosuppressive drugs in the month preceding the test, with a history of topical steroid application on the back in the eight days prior to the test, or with a history of other photosensitive conditions such as systemic lupus erythematosus or systemic conditions with abnormal skin hyperpigmentation such as thyroid disease and Addison’s disease were excluded from the study. Antihistamines, if any, were withdrawn at least seven days before testing. After taking pre-informed written consent, demographic details, a clinical history, details of the application of any cosmetic product (such as oils) over the face and scalp, and a history of drug intake were recorded.
Patch and Photopatch Testing
A total of nineteen allergens were tested (Table 1). Twelve of these were obtained from the Indian Standard Battery and Cosmetic and Fragrance Series approved by the Contact and Occupational Dermatoses Forum of India (CODFI). The rest of the allergens, that is, sunscreens and drug-related allergens, were prepared in the pharmacology laboratory of the institute from raw material obtained from HiMedia Laboratories, Mumbai. Readymade aluminum patch test chambers were employed to load the allergens. Allergens were applied in duplicate sets to the mid-upper back avoiding the paravertebral groove. After keeping them in position for 48 hours, the chambers were removed. Subsequently, one site was covered with a light-impermeable occlusive dressing while the other was irradiated with a broad-spectrum UVA source at a dose of 5 J/cm2). The grading of the results was conducted twice, before irradiation and 48 hours after irradiation, using the International Contact Dermatitis Research Group (ICDRG) scoring system. The relevance was recorded using the COADEX system (current, old or past, actively sensitized, do not know, and exposed or cross-reaction).
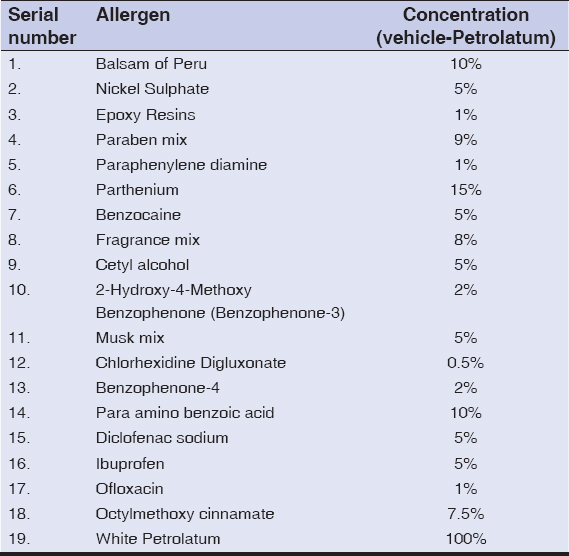 |
Table I: List of allergens and their concentration |
The interpretation of photopatch testing was performed according to standard photopatch criteria. That is, if only the irradiated side showed a positive reaction, it was labeled as a photoallergic reaction. If both sides showed a positive reaction, with the irradiated side showing a greater than 1+ positivity, it was termed contact dermatitis with photoaggravation. If both sides showed an equal reaction after irradiation, a contact allergy was the result.
Statistical evaluation was done with the chi-squared test.
Ethics Statement
The present study was conducted after taking approval from the Institutional Ethics Committee. All clinical investigations were conducted according to the principles of the Declaration of Helsinki.
RESULTS
Demographic and Clinical Profile
Out of the fifty patients, 41 (82%) were females and 9 (18%) were males. The age of the patients ranged from 21 to 53 years, with a mean age of 38 years. Out of the fifty patients, the most were housewives, that is, 26 (52%), 7 (14%) were teachers, and 3 (6%) were nurses. The rest were various skilled workers. Out of 36 married females, 13 (36%) gave a positive history of facial pigmentation during the previous pregnancy. The duration of facial pigmentation varied from less than six months to more than ten years. A history of drug intake was present in 22 (44%) patients, with the most taking various analgesics, including non-steroidal anti-inflammatory drugs (NSAIDS). Seasonal variation was present in 38%, with 13 patients (26%) giving a history of summer aggravation. 72% (36) of the patients gave a history of cosmetic use. A history of mustard oil application was present in 25 (50%), amla oil in 21 (42%), hair dye in 28(56%), henna application to the scalp in 21 (42%), perfume application in 15 (30%), and an allergy to artificial jewelry in 10 (20%). A majority of the patients belonged to Fitzpatrick skin type IV (70%), followed by type III (30%). Regarding the color of pigmentation, 30 (60%) patients had dark brown pigmentation, followed by 12 with light brown (24%) as well as 4 with bluish and 4 with mixed pigmentation (8%). Among the clinical patterns, a centrofacial pattern was the leading in 22 (44%) patients, followed by a malar pattern in 9 (18%). Other sites of pigmentation were various periorbital, temple, mandibular, forehead, perioral, preauricular, and nasal patterns in the rest 38% of the patients. Extrafacial pigmentation was present in 10 (20%) patients, that is, V of the neck, nape of the neck, back, arms, and forearms.
Clinical Diagnosis
Melasma was the most common clinical diagnosis in 33 (66%) patients, followed by pigmented contact dermatitis in 10 (20%), lichen planus pigmentosus in 6 (12%), and post-inflammatory pigmentation in 1 (2%).
Patch and Photopatch Test Results
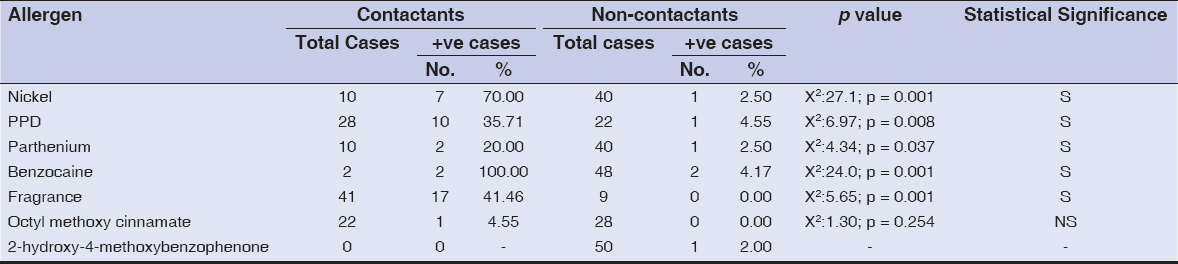
Out of the fifty patients, 28 (56%) showed a positive patch test. A total of 45 patch tests were positive. One was doubtful. The most common allergen showing patch test positivity was the fragrance mix in 17 patients (34%), followed by paraphenylenediamine (PPD) in 11 (22%). Fig. 1 shows the results of the patch test. Out of the 28 patients showing patch test positivity, 17 patients showed positivity to only one allergen, 6 patients showed positivity to two allergens, and 5 patients showed positivity to three or more allergens. Table 2 shows positive patch tests amongst contactants vs non-contactants and the statistical analysis of the same. The comparison of a positive patch test with a positive history of contact with the allergen was found to be statistically significant in most of the allergens, except octyl methoxycinnamate. The relevance was old (O) in 8, exposed (E) in 31, and difficult to assess (D) in 6.
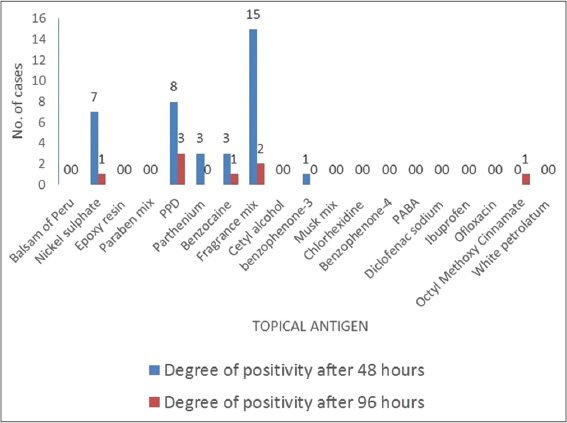 |
Figure 1: Results of patch testing, with the fragrance mix being the leading allergen, followed by PPD and nickel sulfate. |
Two patients (4%) showed photopatch positivity to a total of five antigens: epoxy resin, benzophenone-3, a musk mix, chlorhexidine, and benzophenone-4 (Fig. 2). One patient showed photoaggravation to a fragrance mix with the degree of sensitivity increasing from + to ++ after photo exposure. The relevance was difficult to assess in all.
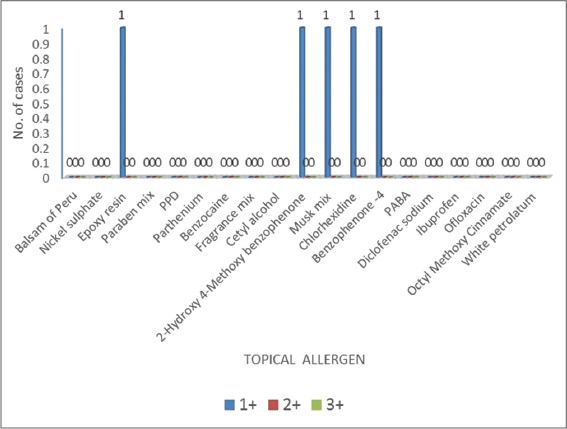 |
Figure 2: Results of photopatch testing with each photopatch test positive to epoxy resin, 2-hydroxy 4-methoxy benzophenone-4. |
Provisional Diagnosis vs. Positive Patch Tests
Fig. 3 shows a comparison between provisional diagnosis based on clinical examination and actual cases with positive patch tests.
 |
Figure 3: Graph showing the comparison of clinical diagnosis vs. positive patch tests in our cases. |
DISCUSSION
Cosmetic dermatitis is on the rise nowadays and has various presentations, with facial pigmentation being one. Patch testing is an important tool for the diagnosis of underlying allergens causing dermatitis. The role of sun exposure is crucial as a causative and aggravating factor, since some allergens become activated only by exposure to sunlight. The combined role of sunlight and allergens may be detected with photopatch testing. The standard patch test series as well as a cosmetic series are able to detect more than 80% of the allergens responsible for dermatoses [1]. The age of the patients in the present study ranged from 21 to 53 years. This is comparable to studies by Bhattarai et al. [2]. Our study showed a female preponderance (82%). This is comparable to studies by Bhattarai et al., Krupa Shankar et al., and Goh et al., who showed a female preponderance ranging from 67.9% to 80.13% [2–4]. This may be explained by the more cosmetic and aesthetic concerns in females. Housewives were the leading group in our study (52%). This was in accordance with a study by Sardesai et al. conducted in 2013, in which 62% of melasma patients were housewives [5]. Although sun exposure was not a significant factor among housewives, exposure to chronic infrared radiation while working in front of a gas stove could have been an aggravating factor. Thirty-six percent of married females gave a history of facial pigmentation during pregnancy. This could be attributed to the role of hormonal factors, especially in melasma. These findings are close to results in studies by Sanchez et al. and Tamega et al., who reported the incidence of melasma in previous pregnancies in 30–32% of subjects [5,6].
Seventy-two percent of patients gave a history of the use of one cosmetic or another in the form, for instance, of over-the-counter fairness creams. The exact composition of these cosmetics was unavailable, which was a hindrance to the specific testing of their ingredients. Prabha et al. determined cosmetic contact dermatitis to be an important causative factor in melasma [7].
A history of amla oil and mustard oil application was present in 42% and 50% of the patients, respectively. Mustard oil contains allyl isothiocyanate and other photosensitizing substances, which further aggravate the hyperpigmentation on the face [8,9].
Fragrances were the leading allergen in our study in 17 (34%) patients (Fig. 4) and were proven to be a cause of cosmetic dermatitis in 30–40% of the cases in previous studies [10,11]. All these patients gave a history of the application of perfumes or OTC cosmetics with fragrances as ingredients. An important fact is that, although some cosmetics are labeled as fragrance-free, they contain some added covert fragrances to mask their original odor. Since these fragrances are also present in household products such as room fresheners, soaps, toothpaste, and haircare products, the wide use of these products in everyday chores makes tracing the source difficult.
 |
Figure 4: Positive patch test (‘++’) to the fragrance mix. |
Twenty-eight cases gave a history of the application of hair dyes, yet only ten showed positivity to PPD (Fig. 5). One patient in our study applied only henna to the scalp, yet showed positivity to PPD. Past reports of contact sensitivity to henna tattoos have shown that PPD is added to enhance the final color [12–14]. This could be the reason why a patch test to PPD was positive in the patient who had never applied synthetic dyes yet had used henna. Nickel alloy is present in artificial jewelry, which is widely popular among females in our country. It is also present in cosmetics, utensils, metallic objects, coins, foods, dental crowns, etc. Tienthavorn et al. found nickel to be the most common allergen in a study on patients with LPP, pigmented CD, and erythema dyschromicum perstans [10]. In our study, eight patients showed a positive patch test to nickel sulfate (Fig. 6), among which seven had a history of allergy to artificial jewelry.
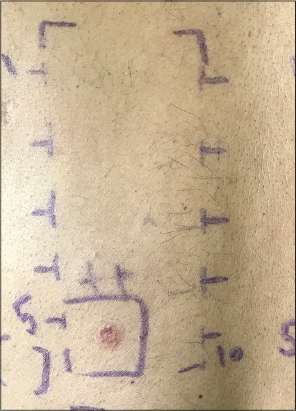 |
Figure 5: Positive patch test (‘++’) to paraphenylenediamine. |
 |
Figure 6: Positive patch test (‘++’) to nickel sulfate. |
The occupation of the patient was significant as four patients showed patch test positivity to benzocaine, among which two were nurses by profession working in an operation theater, and possible exposure in the workplace may be an explanation for prior sensitization. Both patients showed positivity to PPD as well. Thus, cross-reactivity between the two may be another explanation for positivity in these patients [15].
Musk ambrette is a fragrance fixative employed both by the food and cosmetic industries. In past, it was found to be the leading allergen in photopatch studies, now replaced by sunscreen agents. Benzophenone-3 was found to be the leading allergen in photopatch testing carried out in Thailand and Bagota [16,17]. UV filters such as benzophenone-4, benzophenone-3, and cinnamates have largely replaced PABA (para-aminobenzoic acid) in sunscreens. These have also replaced musk ambrette in being the leading photoallergens in Western studies [18].
Photopatch tests were positive in two (4%) of the fifty patients in our study. One showed photopatch positivity to three allergens—a musk mix, chlorhexidine, and benzophenone-4 (Fig. 7)—while the other showed positivity to epoxy resin and benzophenone-3.
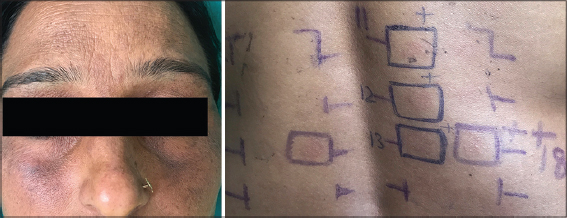 |
Figure 7: Centrofacial pigmentation in a patient with a patch test ‘+’ positive to octyl methoxycinnamate and a photopatch test positive ‘+’ each to the musk mix, chlorhexidine, and benzophenone-4. |
The lower incidence of photopatch positivity to these in our study may be attributed to the less frequent routine use of sunscreen by people in India as well as to the low availability of photopatch allergen series. No definite correlation between a history of exposure and patch test results was found. Polysensitivity may be because of cross-reactivity, simultaneous exposure to multiple allergens in predisposed individuals, or non-specific hyperreactivity.
It is of concern that 51.5% of cases clinically diagnosed as melasma showed positive patch tests to various allergens. Similarly, 50% of the patients clinically diagnosed with LPP showed positive patch tests (Fig. 3). This suggests that underlying dermatitis is an important factor and may not manifest with classical symptoms and signs since the amount of allergen to which a person is exposed is very low. It causes a disturbance in the dermoepidermal junction (DEJ), which is sufficient to cause basal membrane damage and pigment incontinence, clinically visible as hyperpigmentation.
The limitations of the present study were that we did not correlate histopathology with clinical features, since the patients were reluctant to facial biopsy. The number of allergens tested was small due to the low availability of photopatch series in India, thus a wider series should have been included.
CONCLUSION
In patients with facial pigmentation, clinical diagnosis alone is insufficient, and further histopathology and patch testing are needed to exclude pigmented CD. The elimination of these allergens aids in the better management of these patients.
The authors certify that written consent was taken regarding the publication of images of lesions for research purposes without disclosing the identity of the patients. The patients understood that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
ABBREVIATIONS
LPP (lichen planus pigmentosus), CD (contact dermatitis).
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. de Groot AC, Beverdam EG, Ayong CT, Coenraads PJ, Nater JP. The role of contact allergy in the spectrum of adverse effects caused by cosmetics and toiletries. Contact Dermatitis. 1988;19:195-201.
2. Bhattarai S, Pradhan K, Sharma S, Rajouria EA. Clinical patterns and epidemiological characteristics of melasma in a tertiary care hospital of Nepal. Pigment Int. 2017;4:35.
3. KrupaShankar DS, Somani VK, Kohli M, Sharad J, Ganjoo A, Kandhari S, et al. A cross-sectional, multicentric clinico-epidemiological study of melasma in India. Dermatol Ther. 2014;4:71-81.
4. Goh CL, Dlova CN. A retrospective study on the clinical presentation and treatment outcome of melasma in a tertiary dermatological referral centre in Singapore. Singapore Med J. 1999;40:455-8.
5. Sardesai V, Kolte J, Srinivas B. A clinical study of melasma and a comparison of the therapeutic effect of certain currently available topical modalities for its treatment. Indian J Dermatol. 2013;58:239.
6. Tamega Ade A, Miot LD, Bonfietti C, Gige TC, Marques ME, Miot HA. Clinical patterns and epidemiological characteristics of facial melasma in Brazilian women. J Eur Acad Dermatol Venereol. 2013;27:151-6.
7. Prabha N, Mahajan VK, Mehta KS, Chauhan PS, Gupta M. Cosmetic contact sensitivity in patients with melasma:Results of a pilot study. Dermatol Res Pract. 2014;2014:316219.
8. Sharma A, Verma AK, Gupta RK, Neelabh, Dwivedi PD. a comprehensive review on mustard-induced allergy and implications for human health. Clin Rev Allergy Immunol. 2019;57:39-54.
9. Kamra N, Kumar S, Mahajan B. Melasma in North Indians:A clinical, epidemiological, and etiological study. Pigment Int. 2014;1:95.
10. Tienthavorn T, Tresukosol P, Sudtikoonaseth P. Patch testing and histopathology in Thai patients with hyperpigmentation due to erythema dyschromicum perstans, lichen planus pigmentosus, and pigmented contact dermatitis. Asian Pac J Allergy Immunol. 2014;32:185-92.
11. Alani JI, Davis MD, Yiannias JA. Allergy to cosmetics:A literature review. Dermatitis. 2013;24:283-90.
12. Hald M, MennéT, Johansen JD, Zachariae C. Severe occupational contact dermatitis caused by black rubber as a consequence of p-phenylenediamine allergy resulting from a temporary henna tattoo. Contact Dermatitis. 2013;68:377-9.
13. Calogiuri G, Di Leo E, Butani L, Pizzimenti S, Incorvaia C, Macchia L, et al. Hypersensitivity reactions due to black henna tattoos and their components:Are the clinical pictures related to the immune pathomechanism?Clin Mol Allergy. 2017;15:8.
14. Gupta M. Pigmented contact dermatitis to p-paraphenylenediamine in a textile factory worker. Our Dermatol Online. 2017;8:424-6.
15. Gilissen L, Goossens A. Frequency and trends of contact allergy to and iatrogenic contact dermatitis caused by topical drugs over a 25-year period. Contact Dermatitis. 2016;75:290-302.
16. Chaiyabutr C, Sukakul T, Limphoka P, Kumpangsin T, Boonchai W. Photopatch testing in a tropical country, Thailand:20 years’experience. Photodermatol Photoimmunol Photomed. 2021;37:28-33.
17. Valbuena Mesa MC, Hoyos Jiménez EV. Photopatch testing in Bogota (Colombia):2011-2013. Contact Dermatitis. 2016;74:11-7.
18. Chuah SY, Leow YH, Goon AT, Theng CT, Chong WS. Photopatch testing in Asians:A 5-year experience in Singapore. Photodermatol Photoimmunol Photomed. 2013;29:116-20.
Notes
Source of Support: Nil,
Conflict of Interest: No conflicts of interest
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.