Bilateral nevus of Ota with palatal involvement, unilateral nevus of Ito, and a port-wine stain: A rare presentation
Alpana Mohta 1, Ramesh Kumar Kushwaha2, Pramila Kumari2, Manoj Kumar Shamra2, Suresh Kumar Jain2
1, Ramesh Kumar Kushwaha2, Pramila Kumari2, Manoj Kumar Shamra2, Suresh Kumar Jain2
1Department of Dermatology, Venereology and Leprosy, Sardar Patel Medical College, Bikaner, Rajasthan, India, 2Department of Dermatology, Venereology and Leprosy, GMC, Kota, India
Corresponding author: Alpana Mohta, MD
How to cite this article: Mohta A, Kushwaha RK, Kumari P, Shamra MK, Jain SK. Bilateral nevus of Ota with palatal involvement, unilateral nevus of Ito, and a port-wine stain: A rare presentation. Our Dermatol Online. 2022;13(2):197-201.
Submission: 31.07.2021; Acceptance: 28.10.2021
DOI: 10.7241/ourd.20222.20
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Nevus of Ota and nevus of Ito are dermal melanocytoses, usually presenting themselves as a bluish-black or grayish-brown, patchy, diffuse, or mottled pigmentation of the skin. They share a common pathogenic mechanism involving failure in the migration of melanocytes from the dermis to the epidermis and differ only in the sites of their distribution on the body. Nevus of Ota, often unilateral, may rarely be bilateral or may involve the oral mucosa. Even rarer is its association with nevus of Ito and other extracutaneous features. A port-wine stain is a form of congenital capillary malformation presenting itself as a pinkish-red to purple discoloration, most commonly of the unilateral head and neck area. Only 25% of cases occur on other sites of the body. The presence of a port-wine stain in conjunction with two different dermal nevi has been an exceedingly rarely reported entity. Herein, we report a 26-year-old male who presented himself with a bilateral nevus of Ota with oral mucosal involvement and associated with nevus of Ito and a port-wine stain.
Key words: Nevus of ota; Dermal nevi; Nevus of Ito; Palatal pigmentation; Port-wine stain
INTRODUCTION
Dermal melanocytoses comprise a broad group of congenital and acquired conditions characterized by scattered, spindle-shaped or dendritic melanocytes in the dermis resulting in a bluish-grey discoloration of the skin [1]. The various morphological forms include the Mongolian spot, blue nevus, nevus of Ota, nevus of Ito, Hori’s nevus (acquired bilateral nevus of Ota such as macules), and Sun’s nevus (acquired unilateral nevus of Ota such as macules) [1,2].
Nevus of Ota, first described by Masao Ota in 1939 as nevus fuscocaeruleus ophthalmomaxillaris [3], is usually unilateral, along the skin, and innervated by the first and second branches of the trigeminal nerve [4], with the involvement of the ipsilateral sclera in about two third of cases [5]. Other mucosal sites such as the palate and nasal mucosa may also be involved.
Nevus of Ito involves the supraclavicular, deltoid, and scapular areas and was first described by Minor Ito in 1954. The simultaneous presentation of nevus of Ota and nevus of Ito is a rarely reported entity [6].
The port-wine stain, another cause of discoloration of the skin, characterized by congenital vascular malformation due to the ectasia of the dermal capillaries, presents itself as non-involuting pinkish-red to purple macules.
Herein, we report the case of a male patient with an exceedingly rarer presentation of a bilateral nevus of Ota, a unilateral nevus of Ito, and a port-wine stain along with palatal lesions.
CASE REPORT
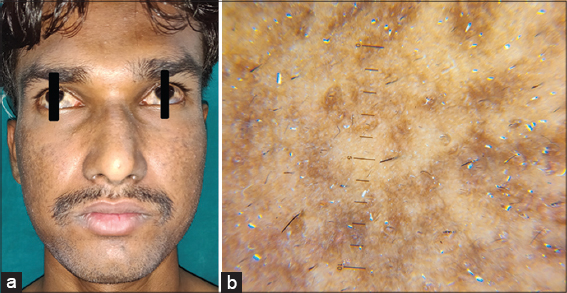
A 26-year-old male patient, born out of a non-consanguineous marriage, presented himself to us with an asymptomatic, bluish-grey pigmentation around the bilateral cheeks, eyelids, and eyes since birth. The lesions had been lighter in color until childhood but had gradually progressed until puberty; they became darker and more pigmented, then becoming stable. The patient also complained of developing similar, but lightly pigmented, grayish lesions on the right shoulder present for the last ten years. The patient also complained of diffusely distributed, red reddish patches on the central part of the back present since birth, which had increased proportionately in size with the growth of the patient until puberty. The patient sought medical consultation because of a cosmetic concern. No family history of similar lesions was present.
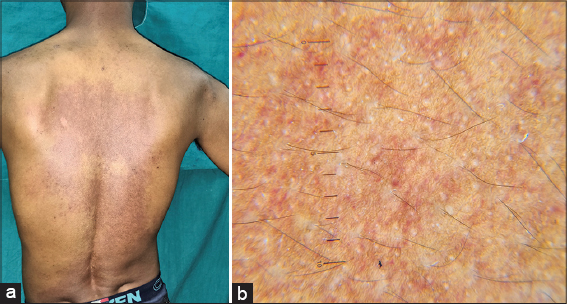
A mucocutaneous examination revealed the presence of bluish, mottled, pigmented macules present over the dorsum of the nose (Figs. 1a and 1b). The pigmentation involved the bilateral temples, eyelids, and periorbital and malar regions. The pigmentation extended medially to the bilateral ala and laterally to bilateral earlobes and helix along with bluish discoloraltion over unilateral hard palate (Fig. 2). A diffuse, ill-defined, lightly pigmented, large, grayish macule was present over the right scapular (Fig. 3a). There was no increased hair growth over the involved areas.
Over the back, there was a large, deep, red macule with ill-defined geographical borders distrusted over the center of the upper and middle back, right side of the middle back, and almost the entire territory of the lower back, extending all the way down to the lumbosacral area. The lesion was blanchable with some areas of normal skin in between the large macule. The lesion was diagnosed clinically as a port-wine stain (Fig. 3a).
An ophthalmological examination revealed a bluish-black pigmentation in the bilateral sclera. The conjunctiva and sclera showed a bilateral inferomedial and inferolateral bluish-black pigmentation around the limbus. There were no abnormalities detected on visual acuity and indirect gonioscopy.
The remaining examination of the oral mucosa was normal. There was no discoloration of the tympanic membrane on auditory examination.
The patient was clinically diagnosed as having a bilateral nevus of Ota along with a nevus of Ito with a port-wine stain.
A dermoscopic examination of the lesions on the face revealed bluish to brown, structureless areas (Fig. 1b). Similar features were seen in the macular lesions on the helix on dermoscopy. Also, on dermoscopy of the bluish lesion, on the right scapular area, there were similar bluish to brown, speckled areas, which were lighter in color (Fig. 4). An examination of the port-wine stain on the back revealed dotted and globular vessels as well as linear, dilated, and tortuous vessels along with pale circular areas around follicular hair openings (Fig. 3b).
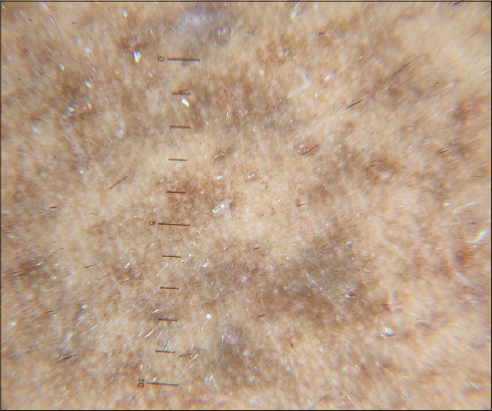 |
Figure 4: Bluish-gray macule on the right scapular. Light brown, structureless areas on the dermoscopy of the right scapular lesion. |
DISCUSSION
Nevus of Ota and nevus of Ito are forms of dermal melanocytosis having a common pathogenic mechanism of failure in the migration of melanocytes, arising from the neural crest to the epidermis. The bluish discoloration of the skin in deeper lesions seen in both of these conditions is due to an optical effect altering the perceived color of the brown pigment in the dermis. The incident visible light absorbed by the melanin in the dermis is dispersed in such a way that the diffuse reflectance in the longer (red) wavelength is reduced, leading to the appearance of the pigmented sites as bluish in color. This effect is called the Tyndall effect [6]. More superficial lesions, however, appear slate gray.
Oculodermal melanosis was first described by Hulke in 1861, followed by Masao Ota in 1939 [3]. Both nevus of Ota and nevus of Ito are much rarer in the white population than in Asians and Afro-Americans. Nevus of Ota has a prevalence falling between 0.014% and 0.034% in the Asian population [6], with a male-to-female ratio of 1:4.8. Most often, the onset is perinatal, yet it may rarely appear around puberty as well. Several factors may influence the intensity of the discoloration, such as puberty, menstruation, stress, ultraviolet light exposure, and changes in weather [7]. Nevus of Ota and nevus of Ito are typically unilateral but bilateral involvement has also been sometimes reported. In around 45% of cases, nevus of Ota occurs bilaterally [8], as in our case, where the closest differential diagnosis is Hori’s nevus. The two may be differentiated clinically as given in Table 1 [9].
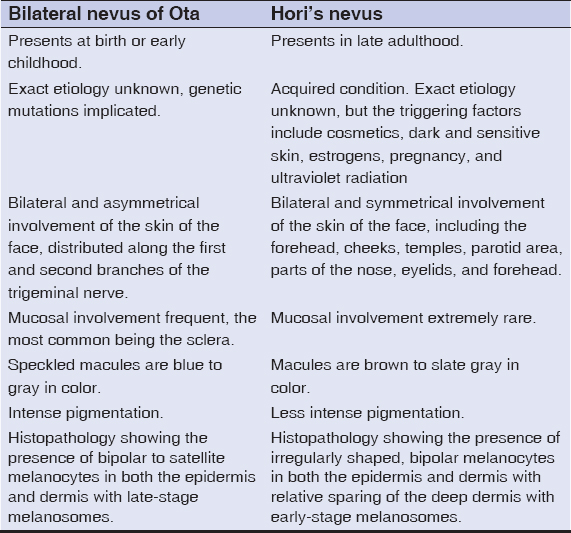 |
Table 1: Comparison of bilateral nevus of Ota and Hori’s nevus |
The extracutaneous lesions involve the eye (sclera, cornea, retina), tympanum, nasal mucosa, pharynx, and palate in descending order of prevalence. The palatal lesions are highly uncommon in nevus of Ota and have been reported to occur more often with bilateral cutaneous involvement and, to the best of our knowledge, apart from ours, only fifteen cases have been reported to date [10,11].
In 1939, Tanino classified nevus of Ota into four major subtypes: type 1 (mild), type 2 (moderate), type 3 (intense), and type 4 (bilateral). A further modification has been proposed by Mukhopadhyay [6] in 2013, with a proposal of including nevus of Ito in the classification by suggesting type 5 (nevus of Ito without nevus of Ota) and type 6 (nevus of Ito with nevus of Ota). According to Tanino’s classification, our case is type 4, whereas, according to the revised classification, our case should be type 6. However, in 2013, the Peking Union Medical College Hospital (PUMCH) proposed a different classification, according to which our case should be type V [12]. Patients with ocular involvement may have complications such as increased intraocular pressure with or without glaucoma, uveitis, cataracts, orbital melanomas, and retinitis pigmentosa. Our patient had no such changes but was advised biannual ophthalmic examination to prevent the development of these complications. Although the association of these two nevi is rare, there are some reports showing their simultaneous presence. Bilateral nevus of Ota with nevus of Ito is exceptionally uncommon, with only a handful of cases having been reported to date.
Histologically, these nevi show a normal epidermis, with the presence of dendritic melanocytes in the papillary and upper reticular dermis, which are surrounded by fibrous sheaths, unlike other dermal melanocytoses, such as blue nevus or Mongolian spots. There might also be the presence of dermal melanophages. Hirayami classified it into five subtypes based on the distribution of the dermal melanocytes as superficial (type S), superficial dominant (type SD), diffuse (type Di), deep dominant (type DD), and deep (type De). They correlate with the color of the nevus: the most brownish lesions are represented by type S or type SD, while the most bluish lesions by types Di, DD, or De. Furthermore, these types strongly correlate with the location of the nevus: types S and SD are more frequent on the cheeks, whereas types Di, DD, and De more frequently occur on the eyelids, temples, and forehead. Nevus of Ota may be associated with various other cutaneous, leptomeningeal conditions and ocular disorders.
A port-wine stain is a congenital capillary vascular malformation with an incidence of around 0.3% [13]. It appears clinically as a homogenous, pinkish-red to deep-purple lesion with a geographic contour. Around 75% of these capillary malformations are present on the head and neck with the majority of cases having the involvement along the distribution of the trigeminal nerve. The remaining 25% of cases may involve other areas of the body, such as the back, as in our case. They may occur in combination with other vascular malformations as part of a syndrome, such as Sturge–Weber syndrome, phakomatosis pigmentovascularis (PPV), Klippel–Trénaunay syndrome, or Servelle–Martorell syndrome [14].
Considerable cosmetic disfigurement may be caused by nevus of Ota and nevus of Ito with occasional emotional and psychological distress. The patient should be counseled on the benign nature of the condition, apart from cosmetic camouflage makeup. Otherwise, topical therapy has no value in the treatment. The first-line management is laser surgery, with Q-switched ruby laser (694 nm) surgery being the treatment of choice. Other lasers such as Q-switched alexandrite (755 nm) and Q-switched Nd: YAG lasers (1064 nm) may also be employed. Other surgical methods include dermabrasion (with or without other modalities, such as carbon dioxide snow), autologous epithelial grafting, cryotherapy, microsurgery, dermabrasion, and sequential dry ice epidermal peeling. As far as the port-wine stain is concerned, the current modality of choice is laser photocoagulation with pulsed dye laser (PDL) [15].
Although, in the past, port-wine stains have been reported with nevus of Ota, to the best of our knowledge, no case report has highlighted the concomitant presence of these two conditions together with nevus of Ito. We are reporting this case for the rarity of the association of these three conditions in the literature.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Fauconneau A, Beylot-Barry M, Vergier B, Robert-Barraud C, Doutre MS. Acquired dermal melanocytosis of the back in a Caucasian woman. Am J Dermatopathol. 2012;34:562-3.
2. Khouna A, Aburabie H, Dikhaye S, Zizi N. A late onset of nevus of Ota in a 38-year-old female. Our Dermatol Online. 2020;11(Supp. 3):13-4.
3. El Kadiri S, Bay Bay H, Chaoui R, Douhi Z, Elloudi S, Mernissi FZ. A new dermoscopic finding in Ota nevus. Our Dermatol Online. 2020;11(e):e11.1-e11.2.
4. Cohen AB. Pediatric Dermatology, 3rd ed. Philadelphia:Elsevier Mosby;2005. 45-146.
5. Paller AS, Mancini AJ. Hurwitz Clinical Pediatric Dermatology, 3rd ed. Philadelphia:Elsevier Saunders;2006. 297-9.
6. Mukhopadhyay AK. Unilateral nevus of Ota with bilateral nevus of Ito and palatal lesion:A case report with a proposed clinical modification of Tanino’s classification. Indian J Dermatol. 2013;58:286-9.
7. Tronnier M. Melanotic spots and melanocytic nevi. In:Burgdorf WH, Plewig G, Wolff HH, Landthaler M, editors. BraunFalco’s Dermatology, 3rd ed. Heidelberg:Springer;2009. 140-23.
8. Syed M MA, Amatya B, Alam S. Bilateral nevus of Ota. Pigment Int. 2018;5:120-2.
9. Bhat RM, Pinto HP, Dandekeri S, Ambil SM. Acquired bilateral nevus of Ota-like macules with Mucosal involvement:A new variant of Hori’s nevus. Indian J Dermatol. 2014;59:293-6.
10. Salunke AS, Nagargoje MV, Chavan RB, Bansal NM. Concomitant presence of bilateral nevus of Ota with unilateral nevus of Ito and halo nevus:A rare association. Int J Res Dermatol. 2017;3:538-40.
11. Adil M, Amin SS, Raj D, Alam M. Bilateral nevus of Ota with involvement of palate:A rare case report. Indian J Paediatr Dermatol. 2018;19:290-2.
12. Huang WH, Wang HW, Sun QN, Jin HZ, Liu YH, Ma DL, et al. A new classification of nevus of Ota. Chin Med J. 2013;126:3910-4.
13. Bansal S, Garg VK, Wadhwa B, Khurana N. Acquired port-wine stain in an adult male:First reported case from India with review of literature. Indian J Dermatol. 2015;60:104.
14. Sharma G, Nagpal A. Nevus of Ota with rare palatal involvement:A case report with emphasis on differential diagnosis. Case Rep Dent. 2011;2011:1-4.
15. Chowdhry S, Yadav N, Umrigar DD, Shukla A. Nevus of Ota with port-wine stain –A rare entity. J Pak Assoc Derma. 2017;27:293-7.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.