Frequency of skin infections and tumors among patients with psoriasis
Khalifa E. Sharquie 1, Fatema A. Al-Jaralla2, Mohammed A. Abulhail3
1, Fatema A. Al-Jaralla2, Mohammed A. Abulhail3
1Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board of Dermatology&Venereology, Dermatology center, Medical city, Baghdad, Iraq, 2Department of Dermatology, College of Medicine, University of Baghdad, Baghdad, Iraq, 3Dermatology Center, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq
Corresponding author: Prof. Khalifa E. Sharquie, MD PhD
How to cite this article: Sharquie KE, Al-Jaralla FA, Abulhail MA. Frequency of skin infections and tumors among patients with psoriasis. Our Dermatol Online. 2022;13(2):126-131.
Submission: 19.07.2021; Acceptance: 19.11.2021
DOI: 10.7241/ourd.20222.2
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Autoimmune diseases are a vast array of organ-specific and systemic diseases whose pathogenesis results from the activation of B and T lymphocytes reacting against the body’s own tissues. Psoriasis is a common, chronic, inflammatory, autoimmune, and proliferative condition of the skin with genetic, immunological, and environmental influences. The objective of the study was to find the frequency of skin infections and tumors in patients with psoriasis with and without immunosuppression in comparison with healthy controls.
Patients and Methods: An observational, analytic, cross-sectional, controlled study in which a hundred psoriasis patients without treatment and a hundred psoriasis patients on systemic immunosuppression for at least six months were included and compared with two hundred healthy individuals in terms of infections and tumors in the Center of Dermatology in Baghdad, Iraq, from March 1, 2019, through November 1, 2020.
Results: Psoriasis patients without therapy (group A) and those on systemic therapy (group B) had statistically significant less infection rates than the control group, as 23% of group A and 21% of group B had no infections, while only 6% of controls had no infections (P = 0.0001 for both groups), whereas individuals who were free of tumors both benign or malignant were significantly more numerous in group A (63%) and group B (62%) than in the control group (40.5%) (P = 0.0002 and P = 0.0008, respectively).
Conclusion: Patients with psoriasis are less susceptible to infections and tumors than the general population. However, psoriasis is less protective than other autoimmune diseases such as pemphigus vulgaris, lupus erythematosus, and vitiligo.
Key words: autoimmune diseases; psoriasis; infections; tumors
INTRODUCTION
Autoimmune diseases are a group of organ-specific as well as systemic diseases whose pathogenesis results from the activation of B and T lymphocytes reacting against antigens of the body’s own tissues [1,2].
Psoriasis is a common, chronic, disfiguring, inflammatory, autoimmune, and proliferative condition of the skin in which multiple etiological factors are involved, such as genetic, immunological, and environmental influences [3,4].
ASSOCIATION BETWEEN AUTOIMMUNE DISEASES AND SKIN INFECTION AND TUMORS
Sharquie et al. have conducted and published a number of studies that found that autoimmune diseases such as pemphigus, systemic lupus erythematosus, and vitiligo had protection against skin tumors and infections, although these diseases were treated by immunosuppressive drugs for a long period of time [5].
Vitiligo demonstrates a protective effect against the development of skin tumors and photosensitivity, and the absence of melanin in the epidermis is not a significant risk factor for the development of skin tumors [6]. In addition, vitiligo has been causally associated with a reduced risk of several cancers, suggesting that vitiligo as an autoimmune disease may play a role in the suppression of cancer, and these findings are well correlated with the presence of p53 [7,8].
Psoriatic plaques are rarely complicated by recurrent infections with bacterial, viral, and fungal pathogens, as only 7% of patients with psoriasis have bacterial or viral skin infections, as compared with 30% of patients with atopic dermatitis [7].
Psoriasis lesions are seldomly impetiginized. This resistance to secondary bacterial infection may be explained by the increased production of skin-derived antimicrobial peptides, for instance, defensins [8].
PSORIASIS AND VITILIGO AS CLOSE RELATIVES
Both vitiligo and psoriasis are inflammatory autoimmune diseases in which Th1 helper cells play a role in their pathogeneses and have genetic elements [3,9].
A study from China found that rs9468925 in HLA-C/HLA-B is associated with both psoriasis and vitiligo, providing the first important evidence that two major skin diseases share a common genetic locus in the MHC and a basis for elucidating the molecular mechanism of skin disorders [10]. Additionally, a meta-analysis revealed that psoriasis and vitiligo are associated with each other [11].
Furthermore, in 2017, Sharquie et al. conducted the first clinical study, which showed that vitiligo and psoriasis are closely linked diseases, as both commonly occur in the same patients and their families. Patients may show psoriasis first, then progress into vitiligo, or the same patch may contain lesions of both psoriasis and vitiligo [3].
In addition, psoriasis has been associated with autoimmune diseases other than vitiligo [12].
Therefore, the objective of this work was to evaluate the frequency of infections and tumors among patients with psoriasis and healthy controls and to be compared with other studies that included the frequency of these infections and tumors among other autoimmune diseases such as pemphigus and vitiligo.
PATIENTS AND METHOD
An observational, analytic, cross-sectional, controlled study was conducted during a period of twenty months, starting on March 1, 2019, and ending on November 1, 2020. Formal consent was taken from each patient after fully explaining the goals and nature of our study. In addition, ethical approval was taken from the Scientific Council of Dermatology and Venereology/Arab Board of Health Specializations. Two hundred patients with psoriasis—110 females (55%) and 90 males (45%)—were evaluated. The patients were seen in the Center of Dermatology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq.
The patients were divided into two groups. Group A included 100 patients with psoriasis—53 females (53%) and 47 males (47%)—with their ages ranging from 5 to 66 years; these patients had taken no medications for their psoriasis. Group B included 100 patients with psoriasis—57 females (57%) and 43 males (43%)—with their ages ranging from 7 years to 64 years; these patients were on continuous systemic therapy for at least the last six months, excluding patients on systemic retinoids or apremilast.
INCLUSION CRITERIA FOR GROUP A
Patients with a diagnosis of psoriasis for at least six months, not on any form of therapy for their psoriasis currently or in the past.
EXCLUSION CRITERIA FOR GROUP A
- Patients taking any oral or parenteral immunosup pressants for psoriasis or other diseases during their lifetime or topical therapies.
- Pregnant females.
- Associated diabetes mellitus.
- Any other associated immunosuppressive condition.
- Patients on or previously exposed to phototherapy.
INCLUSION CRITERIA FOR GROUP B
Patients with a diagnosis of psoriasis on continuous systemic immunosuppressive therapy for at least the last six months.
EXCLUSION CRITERIA FOR GROUP B
- Patients with any interruption of systemic therapy in the last six months.
- Patients on a systemic retinoid or apremilast.
- Pregnant females.
- Any associated immunosuppressive diseases.
- Patients with diabetes mellitus.
- Patients on or previously exposed to phototherapy.
In addition, two hundred apparently normal individuals—93 males (46.5%) and 107 females (53.5%)—were included as controls, with their ages ranging from 4 to 67 years; these were non-diabetic and had no history of taking any immunosuppressing drugs during their lifetime.
A full history was taken from each patient and control, including age, sex, duration of disease, and a detailed history of treatment protocols. A physical examination was performed, including a complete skin examination for both the covered and exposed skin for dermatological tumors, infections, and other skin lesions, as well as an examination of the nails, hair, and mucous membranes. The affected body surface area was assessed and the calculation of the PASI score for the patients with psoriasis with an Android application (Psoriasis Calc) was performed.
Calculations were performed with Microsoft Excel 2013. Categorical variables were expressed as frequencies and percentages, and continuous variables as means and standard deviations. The chi-square test was used to assess the significance of the relationship between two categorical variables, while ANOVA was used to evaluate the differences among three groups and P values, with values ≤ 0.05 considered statistically significant. The results are demonstrated in tables and/or graphs.
RESULTS
This study was conducted to demonstrate the frequency of skin infections and tumors in psoriatic patients without therapy (group A) and those on systemic therapy (group B) in comparison with healthy controls.
Demographic Data
Group A included 100 psoriasis patients without treatment—47 (47%) males and 53 (53%) females—with their age ranging from 5 to 66 years; they had had psoriasis for a mean of 64.61 months (SD = 75.046; ranging from 6 to 360 months), their mean psoriasis area and severity index (PASI score) was 7.9595 (SD = 7; range: 1–33), their mean body surface area was 12.44% (SD = 17; range = 1–90%), and their mean age was 36.9 years (SD = 14.8).
Group B included 100 psoriasis patients—43 (43%) males and 57 (57%) females—with their age ranging from 7 to 64 years; the mean duration of their psoriasis was 81.72 months (SD = 70.30; range = 12–360 months), their mean PASI score was 8.59 (SD = 10.58; range = 1–70); their mean body surface area was 10.3% (SD = 14; range: 1–90%), and their mean age was 40.63 years (SD = 11.87). They had been on systemic therapy for at least six months (73 patients were on etanercept, 24 were on methotrexate, two were on a combination of methotrexate and etanercept, and one was on a combination of methotrexate and cyclosporine).
The control group included 200 apparently healthy individuals—93 (46.5%) males and 107 (53.5%) females—with their age ranging from 4 to 67 years; their mean age was 38.96 years (SD = 12.9).
FREQUENCY OF INFECTIONS
Psoriatic patients without therapy and those on systemic therapy, in general, showed a smaller statistically significant infection rate than the control group, as 23% of psoriatic patients without therapy (group A) and 21% of psoriatic patients on systemic therapy (group B) had no infections, while only 6% of the controls had no infections. Table 1 presents details on the different infections. However, as per the analysis of variance (ANOVA) comparing mild, moderate, and severe psoriasis within each group, there was no statistically significant correlation between the severity of psoriasis and the frequency of infection across both groups (P = 0.49 for group A; P = 0.34 for group B).
 |
Table 1: The distribution of skin infections in psoriatic patients without treatment (group A) and on systemic drugs (group B) in comparison with controls. |
FREQUENCY OF TUMORS
Individuals free of tumors (benign or malignant) were significantly more numerous in groups A and B than in the control group (63% of group A were free of tumors, 61% of group B were free of tumors, 40.5% of the controls were free of tumors; P = 0.0002 for group A, P = 0.0008 for group B). Table 2 presents details on the different infections.
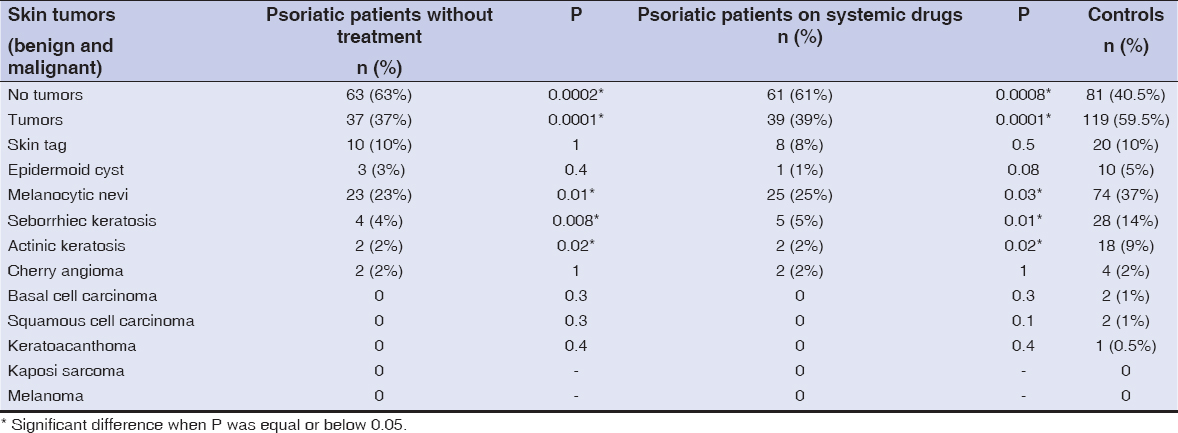 |
Table 2: The distribution of benign and malignant skin tumors in psoriatic patients (without therapy and with systemic therapy) and controls. |
However, as per ANOVA comparing mild, moderate, and severe psoriasis within each group, there was no statistically significant correlation between the severity of psoriasis and the frequency of tumors across both groups (P = 0.08 for both groups).
DISCUSSION
There are clinical studies supporting the theory stating that autoimmune diseases present less frequent infections and tumors in comparison with healthy controls. In 2014, Sharquie et al. were the first to document that patients with pemphigus vulgaris are less susceptible to infections and tumors compared with patients with renal transplants and healthy controls [5].
Moreover, Sharquie et al., by subsequent studies, also showed that patients with lupus erythematosus and with alopecia areata are less susceptible to infections and tumors compared with renal transplant patients and healthy individuals [1].
Similarly, Sharquie et al. revealed that the severity of vitiligo is closely correlated with the frequency of viral warts and tumors, as patients with mild vitiligo had more frequent warts and tumors than patients with severe vitiligo [6]. They noticed that patients with localized vitiligo had 44.5% of warts and tumors, in contrast to patients with generalized vitiligo, who had 10% of warts and tumors. On the other hand, patients with universal vitiligo had only 2%. Control individuals had 66.2% of warts and tumors [6].
Further studies demonstrated that vitiligo and psoriasis are closely linked diseases [3,13]. These interesting findings had encouraged us to conduct the present work. The results of this study confirmed that 78% of psoriatic patients have a history of infections, as compared with 94% of controls with a history of infections, and this is a statistically significant finding (P = 0.0001).
In addition, patients with psoriasis had statistically significantly fewer tumors collectively (38%) when compared with controls (59.5%) (P = 0.0001).
In comparison with vitiligo patients in Sharquie’s study [1], psoriatic patients showed a higher frequency of infections (78% in psoriatic patients vs. 10% in vitiligo patients; P = 0.0001) and a higher frequency of tumors (38% in psoriatic patients vs. 9% in vitiligo patients; P = 0.0001). Accordingly, vitiligo patients are more immune to infections and tumors than patients with psoriasis.
In comparison with pemphigus vulgaris in the previous study [1], psoriasis also appears to be less protective against infections (the infection rate was 78% in psoriatic patients vs. 18% in patients with pemphigus vulgaris; P = 0.0087) and less protective against tumors (the tumor rate was 38% in psoriatic patients vs. 20% in patients with pemphigus vulgaris; P = 0.0001). Accordingly, patients with pemphigus vulgaris are more immune to infections and tumors than patients with psoriasis.
Moreover, in comparison with patients with lupus erythematosus in the previous study [1], psoriasis appears to be less protective against infections (the infection rate was 78% in psoriatic patients vs. 56% in patients with lupus erythematosus; P = 0.0002) and less protective against tumors (the tumor rate was 38% in psoriatic patients vs. 16% in patients with lupus erythematosus; P = 0.0014). Accordingly, patients with lupus erythematosus are more immune to infections and tumors than patients with psoriasis.
Hence, when these autoimmune diseases are compared with one another, the findings appear to be that vitiligo, pemphigus vulgaris, and lupus erythematosus are more protective than psoriasis against infections and tumors (Fig. 1).
 |
Figure 1: Comparison of the frequencies of infections and tumors among different autoimmune skin diseases. |
The question to be raised is why these autoimmune diseases are protective against infections and tumors. This cannot be easily explained and documented. We may, however, put forth some ideas based on the results of the previous studies. For instance, the overexpression of the p53 gene in vitiliginous areas confers protection in cases of vitiligo [14].
With regard to psoriasis, these findings may also be applied, as it is considered an autoimmune disease. In addition, a recent study conducted in Berlin by Kerstin et al. found that psoriatic patients are immune to viral infections due to the presence of antiviral peptides, and the level of these antiviral peptides correlates directly with the level of interleukin-29 produced by Th17 cells [15].
CONCLUSION
Patients with psoriasis, as an autoimmune disease, are less susceptible to infections and tumors than the general population. However, other autoimmune diseases such as pemphigus vulgaris, lupus erythematosus, and vitiligo are more protective than psoriasis. A further study assessing the frequency of the p53 marker in the skin of patients with psoriasis is highly recommended.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Sharquie KE, Noaimi AA, Burhan ZT. The frequency of skin tumors and infections in patients with autoimmune diseases. J Cosmet Dermatol Sci Appl. 2016;6:140-7.
2. Smith DA, Germolec DR. Introduction to immunology and autoimmunity. Environ Health Perspect. 1999;107(Suppl 5):661-5.
3. Sharquie KE, Salman HA, Yaseen AK. Psoriasis and vitiligo are close relatives. Clin Cosmet Investig Dermatol. 2017;10:341-5.
4. van de Kerkhof PCM, Nestle FO. Psoriasis. In:Bolognia JL, Schafeer JV, Cerroni L Dermatology. 4th edition. Philadelphia:Elsevier;2018. 138.
5. Sharquie KE, Noaimi AA, Al?Jobori AA. Skin tumors and skin infections in kidney transplant recipients vs. patients with pemphigus vulgaris. Int J Dermatol. 2014;53:288-93.
6. Sharquie K, Noaimi A, Murtada S. Frequency of benign and malignant tumors in localized vitiligo in comparison to generalized and universal vitiligo. J Cosmet Dermatol Sci Appl. 2016;06:133-9.
7. Elfatoiki FZ, El Azhari M, El Kettani A, Serhier Z, Othmani MB, Timinouni M, et al. Psoriasis and staphylococcus aureus skin colonization in Moroccan patients. Pan Afr Med J. 2016;23:33.
8. van de Kerkhof PCM, Nestle FO. psoriasis. In:Bolognia JL, Schafeer JV, Cerroni L Dermatology. 4th edition. Elsevier;2018. 149.
9. Das D, Akhtar S, Kurra S, Gupta S, Sharma A. Emerging role of immune cell network in autoimmune skin disorders:An update on pemphigus, vitiligo and psoriasis. Cytokine Growth Factor Rev. 2019;45:35-44.
10. Zhu K-J, Lv Y-M, Yin X-Y, Wang Z-X, Sun L-D, He S-M, et al. Psoriasis regression analysis of MHC loci identifies shared genetic variants with vitiligo. PloS One. 2011;6:e23089.
11. Yen H, Chi C-C. Association Between psoriasis and vitiligo:A systematic review and meta-analysis. Am J Clin Dermatol. 2019;20:31-40.
12. Wu JJ, Nguyen TU, Poon K-YT, Herrinton LJ. The association of psoriasis with autoimmune diseases. J Am Acad Dermatol. 2012;67:924-30.
13. Sharquie KE, Sharquie IK, Al Hamza AN. Psoriasis, pityriasis alba, and vitiligo (PPV) are a triad of one disease:New observation. Our Dermatol Online. 2021;12:314-23.
14. Sharquie KE, Noaimi AA. Vitiligo:Skin Malignancies and Tumor Suppressive Marker P53. J Pigment Disord [Internet]. 2014 [cited 2020 Jun 20];01(01). Available from:https://www.omicsgroup.org/journals/vitiligo-skin-malignancies-and-tumor-suppressive-marker-p-jpd.1000104-3Ee3.php?aid=27579
15. Wolk K, Witte K, Witte E, Raftery M, Kokolakis G, Philipp S, et al. IL-29 Is Produced by TH17 cells and mediates the cutaneous antiviral competence in psoriasis. Sci Transl Med. 2013;5:204ra129-204ra129.
Notes
Source of Support: Self-funded study.
Conflict of Interest: We have no conflict of interest.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-0265-2040 http://orcid.org/0000-0002-0265-2040 http://orcid.org/0000-0001-9932-7043 http://orcid.org/0000-0001-9932-7043 http://orcid.org/0000-0002-9018-0599 http://orcid.org/0000-0002-9018-0599 |



Comments are closed.