Autoeczematization Id reaction following candidal diaper dermatitis
Shikhar Ganjoo 1, Tulika Gupta2
1, Tulika Gupta2
1Department of Dermatology & STD, Shree Guru Gobind Singh Tricentenary Medical College and Hospital, Gurugram, India, 2Department of Ophthalmology, Shree Guru Gobind Singh Tricentenary Medical College and Hospital, Gurugram, India
Corresponding author: Shikhar Ganjoo, MD
How to cite this article: Ganjoo S, Gupta T. Autoeczematization Id reaction following candidal diaper dermatitis. Our Dermatol Online. 2022;13(2):187-189.
Submission: 30.08.2021; Acceptance: 30.01.2022
DOI: 10.7241/ourd.20222.17
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Id reactions are secondary inflammatory reactions that develop from a remote, localized immunological insult. They may be caused by various fungal, bacterial, viral, and parasitic infections. Diaper dermatitis with psoriasiform Id eruptions is a rarely reported phenomenon. Herein, we report the case of an infant who developed candidal diaper dermatitis followed by generalized psoriasiform Id eruptions. Most authors report the resolution of diaper area lesions with topical antifungals with or without steroids and Id eruptions with topical steroids alone. Our patient showed complete resolution of all lesions with oral fluconazole alone.
Key words: Id reaction; Candidal rash; Diaper dermatitis; Psoriasiform ID; Fluconazole
INTRODUCTION
Id reactions exhibit multiple clinical presentations, including localized or widespread vesicular lesions, maculopapular or scarlatiniform eruptions, erythema nodosum, erythema multiforme, erythema annulare centrifugum, Sweet’s syndrome, guttate psoriasis, and autoimmune bullous disease. The mechanisms underlying Id reactions vary depending on the type of clinical presentation. Fergusson et al. studied 52 cases of diaper dermatitis with psoriasiform Id eruptions and found Candida albicans to be a causative agent [1]. Other causes include infantile seborrheic eczema, psoriasis, atopic dermatitis, and ammoniacal diaper dermatitis [2]. The patient initially presents with intensely erythematous, papulo-squamous eruption with satellite lesions and pustules. A secondary generalized psoriasiform eruption occurs days to weeks later.
CASE REPORT
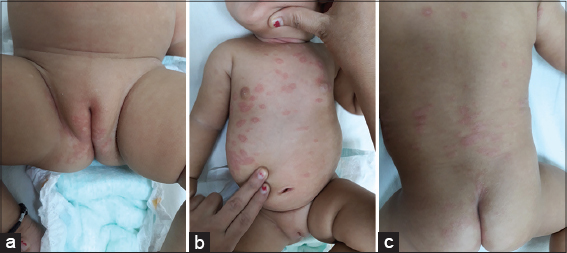
A six-month-old infant presented with a one-week history of multiple reddish, scaly skin lesions in the trunk area. An inspection of the diaper area revealed multiple reddish, moist, elevated skin lesions. No history of atopy or psoriasis was present in the family members. An examination revealed a well-defined area of intense erythema and papules with some satellite papules around the larger lesion in the diaper area also involving the groin folds (Fig. 1a). Similar lesions were also present in the neck fold area. Multiple well-defined erythematous plaques with loosely adherent white scales were seen in the trunk area (Figs. 1b and 1c). A potassium hydroxide (KOH) examination of the diaper and neck fold area revealed budding yeast cells suggestive of Candida albicans, whereas the trunk lesions showed no fungal elements (Fig. 2).
Routine blood investigations were done and returned normal. The patient was treated with oral fluconazole at a dose of 6 mg/kg of body weight for ten days. The lesions in the diaper area, neck folds, and trunk resolved completely with post-inflammatory hypopigmentation in ten days with no subsequent reoccurrence (Figs. 3a and 3b).
 |
Figure 3: (a and b) Post-treatment pictures of the complete resolution of the psoriasiform lesions leaving post-inflammatory hypopigmentation. |
DISCUSSION
Diaper dermatitis is a common condition, especially among newborns and infants. It is an irritating and inflammatory acute dermatitis of the perineal and perianal areas resulting from occlusion and irritation caused by diapers. Diapers create particular conditions of moisture and friction, and with urine and feces come increased pH and irritating enzymes (lipases and proteases) [3]. Fungi may take advantage of all these factors to cause infection. Candida yeasts, especially Candida albicans, are responsible for the most frequent secondary infections.
Early irritant dermatitis is characterized by erythema, mild maceration, and edema, while Candida diaper dermatitis (CDD) is characterized by erythematous and scaly plaques with maceration and edema, sometimes with satellite pustules or papules, the latter being the most characteristic feature of Candida infection [4]. Erosion and ulceration may occur in severe cases.
Id reaction is also known as an auto eczematous response, as there must be an identifiable initial inflammatory or infectious skin problem that leads to generalized eczema. Josef Jadassohn, a German dermatologist who coined the term Id, observed a dermatophytosis infection causing secondary allergic skin dermatitis [5]. Alex et al. observed infants who developed erythema multiforme and psoriasiform-type Id reactions due to a Candida spp. infection in the diaper area [6]. Fergusson et al. studied 52 cases of diaper dermatitis and napkin dermatitis that later evolved into disseminated psoriasiform Id eruptions [1]. One of the definite causes was attributed to Candida albicans in these cases. Other causes included infantile seborrheic eczema, psoriasis, atopic dermatitis, and ammoniacal diaper dermatitis.
Rattet et al. studied two cases of diaper dermatitis with the subsequent presence of generalized, papulosquamous, scaly lesions. Biopsies from these lesions showed psoriasis-like histological features [2]. Another such case was studied by Balasubramanian et al., in which a post-ureterostomy infant on prolonged antibiotic therapy developed candidal diaper dermatitis followed by generalized psoriasiform Id eruptions [7].
Due to paucity of literature on the topic, we report a case of an infant who presented with generalized skin lesions resembling psoriasis clinically, with the simultaneous presentation of candidal diaper dermatitis. Most authors report the resolution of diaper area lesions with topical antifungals with or without steroids and Id eruptions with topical steroids alone [8]. Our patient showed complete resolution of all lesions with oral fluconazole alone.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Fergusson AG, Fraser ND, Grant PW. Napkin dermatitis with psoriasiform “ide“:A review of fifty-two cases. Br J Dermatol. 1966;78:289-96.
2. Rattet JP, Headley JL, Barr RJ. Diaper dermatitis with psoriasiform Id eruption. Int J Dermatol. 1981;20:122-5.
3. Fölster-Holst R. Differential diagnoses of diaper dermatitis. Pediatr Dermatol. 2018;35 Suppl 1:s10-s18.
4. Dutta A, Dutta M, Nag SS. Candidal diaper dermatitis. Indian Pediatr. 2015;52:1100.
5. Ilkit M, Durdu M, KarakaşM. Cutaneous Id reactions:A comprehensive review of clinical manifestations, epidemiology, etiology, and management. Crit Rev Microbiol. 2012;38:191-202.
6. Alex MP, Mohan L, Singh KK, Mukhiya RD. Erythema annulare centrifugum due to candida infection. Indian J Dermatol Venereol Leprol. 1999;65:283-4.
7. Balasubramanian P, Jagadeesan S, Thomas J, Panicker VV, Anjanayen G. Diaper dermatitis with psoriasiform Id eruptions. Indian J Dermatol Venereol Leprol. 2015;81:435.
8. Colcannon P, Gisoldi E, Phillips S, Grossman R. Diaper dermatitis:A therapeutic dilemma. Results of a double-blind, placebo-controlled trial of miconazole nitrate 0.25%. Pediatr Dermatol. 2001;18:149-55.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-8253-7706 http://orcid.org/0000-0001-8253-7706 |




Comments are closed.