Intracerebral hemorrhage as a rare manifestation in a patient with neurofibromatosis-1 and quasi-Moyamoya disease
Jeanne Maria Dsouza1, Ipshita Bhattacharya 2, Sudhish Gupta3, Rajesh Chetiwal3, Mukesh Yadav4
2, Sudhish Gupta3, Rajesh Chetiwal3, Mukesh Yadav4
1Kasturba Medical College, Manipal, India, 2Department of Dermatology, ESIPGIMSR, New Delhi, India, 3Department of Medicine, ESIPGIMSR, New Delhi, India, 4Department of Dermatology, ESI Hospital, Jaipur, India
Corresponding author: Ipshita Bhattacharya, MD
How to cite this article: Dsouza JM, Bhattacharya I, Gupta S, Chetiwal R, Yadav M. Intracerebral hemorrhage as a rare manifestation in a patient with neurofibromatosis-1 and quasi-Moyamoya disease. Our Dermatol Online. 2022;13(2):183-186.
Submission: 26.11.2022; Acceptance: 02.02.2022
DOI: 10.7241/ourd.20222.16
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Neurofibromatosis-1 (NF-1) is an autosomal dominant neurocutaneous syndrome with incomplete penetrance and variable phenotypic expressivity. Although it may affect any system of the body, the disease remains generally innocuous. NF-1 has been commonly linked to neurological symptoms, including headaches, seizures, cognitive deficits, and learning disabilities, and others. While optic glioma is the most common CNS complication, vasculopathy and cerebrovascular anomalies have also been rarely reported. Specifically, intracerebral hemorrhage with vascular stenosis in NF-1 is an extremely rare manifestation. Herein, we report a patient with NF-1 presenting with stroke secondary to intracranial hemorrhage and underlying quasi-Moyamoya disease. Since the cutaneous features of NF-1 appear early in life and are striking, dermatologists might be the first contact for such patients with the medical system, and consequently play an important role in the diagnosis, evaluation, and prevention of complications.
Key words: Neurofibromatosis-1; Genodermatoses; Stroke; Cerebrovascular anomalies; Moyamoya disease
INTRODUCTION
Neurofibromatosis-1 (NF-1) is a neurocutaneous syndrome affecting multiple systems, especially the skin, the eye, and the musculoskeletal, cardiovascular, and nervous systems. It is inherited in an autosomal dominant manner and the responsible gene is located on chromosome 17. As the skin lesions appear early and are conspicuous, patients usually present to the dermatologist. Diagnosis is based on the National Institute of Health (NIH) Consensus Development Conference diagnostic criteria [1]. A thorough workup for possible systemic involvement is imperative. Among the systemic features of involvement, cerebrovascular anomalies, including vascular stenoses and aneurysms, are rare yet recognized entities [2]. However, intracerebral hemorrhage with vascular stenosis in NF-1 is extremely unusual and of uncertain etiopathogenesis with only several cases published in the literature [3,4]. An interesting case of initially undiagnosed NF-1 presenting as an acute neurological emergency is being reported and its possible causes discussed.
CASE REPORT
A 44-year-old male presented to casualty with sudden weakness in the right upper and lower limbs persistent for one day, slurring of speech for four to six hours, and transient lateral deviation of the right side of the mouth. There was no history of trauma, loss of consciousness, an altered sensorium, headaches, seizures, blurring of vision, shortness of breath, palpitations, loss of bladder and bowel control, or any sensory deficit except a mild tingling sensation in the right foot. There was no history of a similar episode of sudden-onset weakness in the past. There was no history of hypertension, diabetes, or a chronic illness, including tuberculosis.
On admission, a general physical examination was normal. A neurological examination revealed a power grade of 4/5 in the flexor and extensor muscles of the right upper and lower limbs tested at the elbow, wrist, hip, knee, and ankle. Owing to a number of the cutaneous manifestations, a dermatology referral was sought, which revealed multiple (70–80 in number) soft papules and nodules present over the neck, trunk, and upper and lower limbs. They were well-defined, non-tender, and mobile and some showed buttonholing (Figs. 1a and 1b). Multiple (8–10) café-au-lait macules (CALMs), ranging from 1 × 0.5 cm to 3 × 2.5 cm in size, were scattered over the trunk and upper limbs. Several brownish-black freckles, 1–2 mm in size, were present over the trunk and the axillary (Fig. 2a) and inguinal regions. On ophthalmic evaluation, the patient had several Lisch nodules in the iris of both eyes (Fig. 2b).
 |
Figure 1: (a-b) Multiple soft, skin-colored papules and nodules on the trunk. |
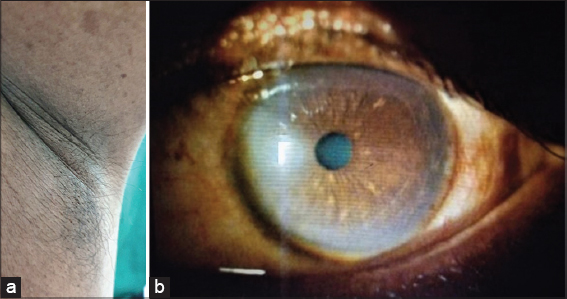 |
Figure 2: (a) Axillary freckling and b) classical Lisch nodules in the iris of the right eye. |
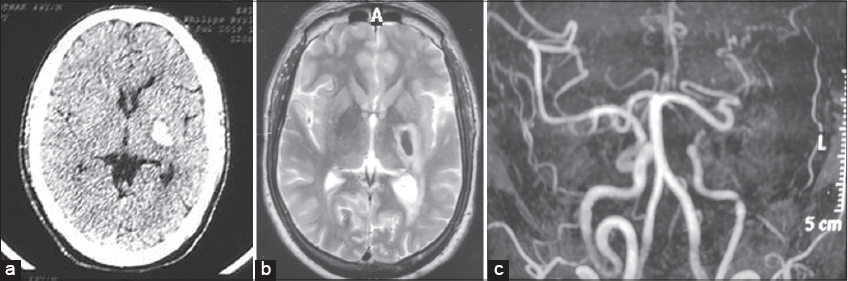
A routine hemogram and biochemical investigations, including blood sugar, a lipid profile, and liver, renal, and thyroid function tests, were normal. A skin biopsy from the nodule on the trunk was compatible with neurofibromatosis. Chest radiograph and ultrasound of the abdomen were unremarkable. NCCY (non-contrast CT) of the head revealed a hyperdense parenchymal lesion in the left basal ganglia, thalamus, and internal capsule, suggestive of hemorrhage with perilesional edema (Fig. 3a). MRI of the brain confirmed the above finding (Fig. 3b). 3D TOF (time of flight) MR angiography revealed stenosis of the cavernous segment of the left internal carotid artery (ICA) with non-visualization of the left middle and anterior cerebral artery with the presence of multiple collateral channels (Fig. 3c).
Based on history taking, the clinical examination, and investigations, a diagnosis of NF-1 with right hemiparesis secondary to intracerebral hemorrhage and underlying quasi-Moyamoya disease was reached. The patient was given injections of dexamethasone and mannitol for five days and was subsequently started on citicoline (a neuroprotective agent). His speech showed signs of improvement by the fourth day and muscle power slowly returned to normal after three months.
DISCUSSION
NF-1 is an autosomal dominant disease with an incidence of 1 in 2500–3300 [5]. Its cutaneous features include CALMs, intertriginous freckling, and discrete cutaneous and subcutaneous neurofibromas, all of which were present in our patient and which are usually sufficient to make the diagnosis based on the NIH criteria [1]. Neurological and cardiovascular involvement may be disabling and sometimes fatal. The most frequent NF-1 complication of the central nervous system is optic glioma, occurring in 5–15% of individuals and is often the first the physician considers in a patient with neurological symptoms [5]. However, a constellation of cerebrovascular lesions has also been reported, including narrowed or ectatic vessels, vascular stenoses, aneurysm, pseudoaneurysm, fistula, and Moyamoya disease [2]. In a study on 353 children with NF-1, cerebrovascular abnormalities were found in 2.5% of the cases [6].
It has been proposed that NF-1-related vasculopathy is secondary to abnormal neurofibromin function and may affect anterior cerebral, and less commonly the posterior cerebral, circulation [2]. The common clinical manifestations include headaches, seizures, and acute neurological deficits secondary to ischemia, due to thrombus or embolization, or intracranial hemorrhage [7]. Moyamoya disease, or more appropriately quasi-Moyamoya disease, with the occlusion of ICA or its branches and numerous resultant collateral channels has also been described [3].
A large case-control study analyzing data from patients with NF-1 between 1998 to 2009 revealed that odds of stroke are significantly increased in patients with NF-1 and may present at a younger age. Adult patients with NF-1 and stroke had a lower prevalence of stroke risk factors, including diabetes, atherosclerosis, and atrial fibrillation [8].
Occlusive cerebrovascular disease presenting with intracranial hemorrhage is a highly rare entity in NF-1, with only several cases reported. A case of a 49-year-old female with NF-1 presenting with intracerebral hemorrhage along with severe ICA stenosis with a fine telangiectatic network of collaterals was reported [4]. Another reported case was of a 39-year-old female with NF-1 presenting with intracerebral hemorrhage secondary to ICA occlusion and numerous collateral channels seen as flow voids on MRI, suggestive of quasi-Moyamoya disease [3]. In the present case, the patient presented de novo with sudden-onset neurological symptoms suggestive of a stroke before he was diagnosed with NF-1. The diagnosis of NF-1 was established only after a cutaneous examination done by the dermatologist. Imaging studies revealing the presence of a ganglio-thalamic bleed with left ICA stenosis and multiple collateral channels pointing toward the rare quasi-Moyamoya disease as the underlying etiology. Had a timely diagnosis of NF-1 and the associated quasi-Moyamoya been made before our patient landed with this complication, interventions, including revascularization surgery, which has been proven to be effective in hemorrhagic MMD, could have been instituted [9].
CONCLUSION
Although rare, physicians should be aware of the increased risk of stroke in NF-1 and evaluate it for the potential causes mentioned above. Screening patients with NF-1 who usually present first to the dermatologist with MRI and MRA to exclude uncommon yet potentially fatal cerebrovascular lesions could facilitate the institution of timely interventions and improve the overall outcome.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Neurofibromatosis. Conference statement. National Institutes of Health (NIH) Consensus Development Conference. Arch Neurol. 1988;45:575-8.
2. Baldauf J, Kiwit J, Synowitz M. Cerebral aneurysms associated with von Recklinghausen’s neurofibromatosis:Report of a case and review of the literature. Neurol India. 2005;53:213-5.
3. Hori YS, Ebisudani Y, Aoi M, Fukuhara T. Adult-onset hemorrhagic quasi-Moyamoya disease with unilateral steno-occlusive lesion in a patient with neurofibromatosis type 1. J Stroke Cerebrovasc Dis. 2018;27:1423-4.
4. Fujimoto K, Shimomura T, Okumura Y. [Severe stenosis of the internal carotid artery and intracerebral hematoma associated with neurofibromatosis type 1:A case report]. No Shinkei Geka. 1999;27:61-5.
5. Singhal S, Birch JM, Kerr B, Lashford L, Evans DG. Neurofibromatosis type 1 and sporadic optic gliomas. Arch Dis Child. 2002;87:65-70.
6. Rosser TL, Vezina G, Packer RJ. Cerebrovascular abnormalities in a population of children with neurofibromatosis type 1. Neurology. 2005;64:553-5.
7. Friedman JM, Arbiser J, Epstein JA, Gutmann DH, Huot SJ, Lin AE, et al. Cardiovascular disease in neurofibromatosis 1:Report of the NF1 Cardiovascular Task Force. Genet Med. 2002;4:105-11.
8. Terry AR, Jordan JT, Schwamm L, Plotkin SR. Increased risk of cerebrovascular disease among patients with neurofibromatosis type 1:Population-based approach. Stroke. 2016;47:60-5.
9. Acker G, Fekonja L, Vajkoczy P. Surgical management of Moyamoya disease. Stroke. 2018;49:476-82.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-1163-0780 http://orcid.org/0000-0003-1163-0780 |



Comments are closed.