Chronic dermatophytosis: A clinical, epidemiological, mycological study
Al-Ramadi Teaching Hospital, Al-Anbar Health Directorate, Ministry of Health/Iraq
Corresponding author: Abdullah Mancy, MD
How to cite this article: Mancy A. Chronic dermatophytosis: A clinical, epidemiological, mycological study. Our Dermatol Online. 2022;13(1):36-40.
Submission: 30.07.2021; Acceptance: 26.11.2021
DOI: 10.7241/ourd.20221.7
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Dermatophytes are a common cause of superficial fungal infection of the skin. The emergence of epidemic-like attacks of those chronic and recurring represents a public health problem.
Materials and Methods: Two hundred patients with suspected fungal infection of the skin attending the Dermatology and Venereology Department of Al-Ramadi Teaching Hospital were examined. Fifty-nine patients with chronic dermatophytosis were selected for the study and fifty of those were subjected for culture. History taking and a physical examination were conducted for all patients. A wet mount of 10% potassium hydroxide and culture on Sabouraud dextrose agar was done for selected cases.
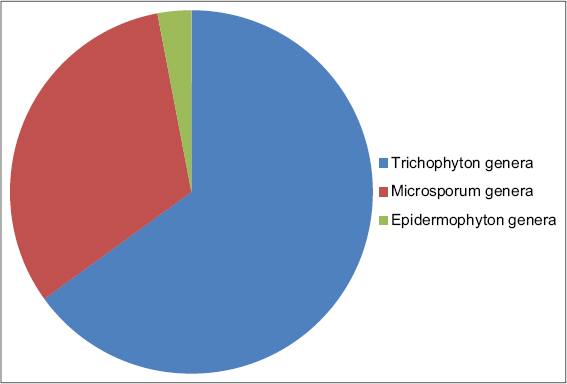
Results: Among 59 patients with chronic infections, the main age group affected was 29 years old, with a nearly equal sex ratio. The mean duration of the illness was 1.2 years. Tinea corporis was the most common type. The Trichophyton genera were the most common (65%), and Trichophyton mentagrophyte was the most common species isolated (46%).
Conclusion: Multiple factors have been associated with the appearance of epidemic-like attacks of chronic dermatophyte infections in Iraq in the last several years. Herein, we would like to shed light on these factors and the pathogens responsible.
Key words: Ringworms; Dermatophytes; Chronic Infections; Potent steroids
INTRODUCTION
Fungal infections attacking humans are classified into three forms: superficial, subcutaneous, and systemic [1]. Dermatophytes are one of the fungi that digest the keratin in the skin, hair, and nails [2]. They are classified into three genera: Trichophyton, Microsporum, and Epidermophyton; and into anthropophilic, geophilic, and zoophilic, according to the mode of transmission [3]. They may affect any site on the body and are clinically known according to that site [4]. In the last years, several terms have been used to describe persistent fungal infections, such as chronic, recurrent, and recalcitrant dermatophytosis [5–7]. In this study, chronicity will be applied to an infection lasting more than six months, with the presence or absence of recurrence despite treatment. Multiple factors in the environment and host and the infecting agents affect the chronicity of an infection. Environmental factors such as weather changes and hot and humid climates are a favorable environment for fungal growth [5,7]. Host factors involve frequent use of antifungal and steroid combinations, noncompliance of the patient with antifungal drugs, obesity, and sedentary lifestyle [7]. Frequent migration of people enhances the spread of the infection with a special strain such as Trichophyton mentagrophyte [8]. A defective immunological status, poverty, and overcrowding are mostly associated with chronic infection [5,7,9]. Infecting agents involve the emergence of novel antifungal, drug-resistant strains of dermatophytes [10,6]. Biofilm produced by some species of dermatophytes enhances virulence and hence chronicity [11]. The immune response is ameliorated to escape the detection by the host immune system [12].
MATERIALS AND METHODS
This study was conducted in the Dermatology and Venereology Department of Al-Ramadi Teaching Hospital and College of Science, Al-Anbar University. After obtaining ethical approval from the institution, two hundred patients suspected to be infected with different types of tinea were examined in the period of six months, from March 2020 to August 2020. We selected cases lasting more than six months despite treatment. After excluding patients affected with tinea capitis and tinea unguium, 59 patients with chronic infection were subjected for this study and 50 of them were subjected for culture. Informed consent was taken from all patients. A detailed history was taken from the patients regarding the duration of the illness, contact with animals, other affected family members, the presence of medical diseases, immunosuppression, a drug history, topical steroid use, migration to other countries, and compliance with drug regimens. A physical examination of the skin, hair, and nails, in addition to laboratory investigations, was performed. The affected skin was cleansed with 70% alcohol and scales were taken from the active border of the lesion with a sterile surgical blade. The scales were divided into two parts: one for direct microscopical examination with a 10% potassium hydroxide (KOH) mount, the other enclosed in a dark, dry paper and sent for culture in Sabouraud dextrose agar (SDA), being incubated at 28°C for at least four weeks. The exact dermatophyte species were identified by the appearance of the growth of a fungal colony in the culture and their microscopic features after using lactophenol cotton blue.
RESULTS
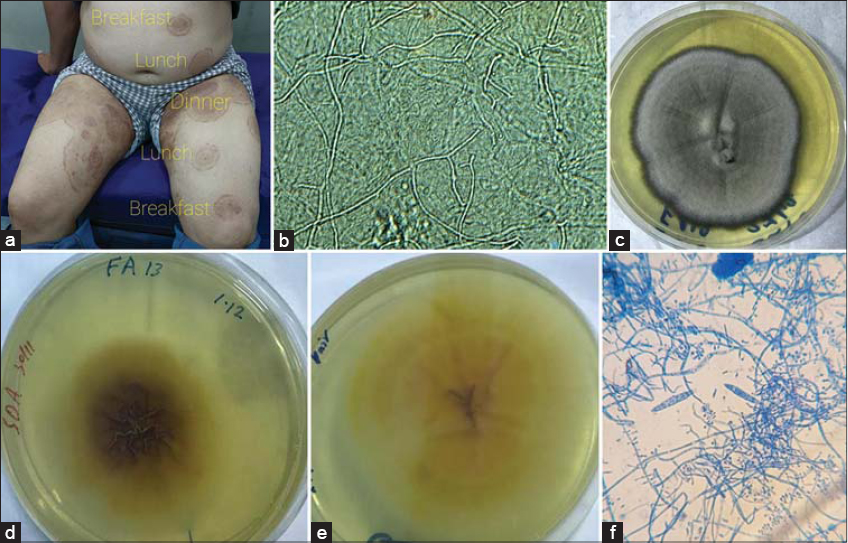
Fifty-nine patients with chronic dermatophytes infection were evaluated. The patients’ age ranged from 2 to 64 years, with a mean age of 29 years and a nearly equal sex ratio. The duration of the infection ranged from 6 months to 6 years, with a mean of 1.2 years. A family history of involvement was present in 66% of the cases, and their residence was rural in 74%. There were different types and sites of involvement in the same patient. The most common clinical type was tinea corporis and tinea cruris (Figs. 1–3). Wet mount of the specimens with 10% KOH was positive in 80%. The culture results were positive in 74% of the cases. Macroscopical and microscopical studies of the growth demonstrated that the Trichophyton genera were the most common infecting agents (Fig. 4). Within the Trichophyton genera, the Trichophyton mentagrophyte species was the most common (Table 1).
 |
Table 1: Distribution of dermatophyte species in the present study. |
DISCUSSION
Superficial fungal infections are common issues that affect around 20–25% of people worldwide, with 30–70% of the adult population being asymptomatic carriers of dermatophytes [13,14]. Previously, infection with dermatophytes was thought to be an easy to treat disease in dermatological clinics yet, in the last several years, this notion has changed due to the appearance of numerous cases of infections in different parts of the world that are difficult to treat. The incidence of chronic dermatophyte infections in the present study was 29.5%. In other parts of the world, there is a steady increase in the incidence of this infection, as described by Pathania et al. [15] and Sharma et al. [16]. Apart from tinea capitis that mainly affects children [17], dermatophyte infection mainly attacks post-pubertal ages, around the age of 20–30 years. Males are more frequently involved than females due to the more frequent outdoor occupational activities in males, which exposes them to a hot and sweaty environment that encourages dermatophyte growth [18,19]. In the present study, all age groups were affected and both sexes were involved equally, which was also observed by Verma et al. [20]. Overcrowding and the involvement of more than one family member in addition to farm work exposing to hot, sweat, and contact with animals all predispose to the contraction of infection [15]. There exist different types and forms of dermatophyte infections. Usually, more than one site is affected. Severe itching, erythema, and the double-edge sign are present. The most common type is tinea corporis followed by tinea cruris. All these features are present in the epidemic-like infection reported by Verma et al. [20]. In the present study, Trichophyton mentagrophyte was the most common infecting agent, which was also found in recent studies by Sheikh et al. [21], Pathania et al. [15], and others [22,23]. Previously, Trichophyton rubrum was the most infective agent, but recently there has been a shift toward Trichophyton mentagrophyte [17]. Numerous factors are involved in changing the virulence of the pathogen, some related to the environment and host and the infective agent or immunological factors [24,25]. In our locality, we believe that the frequent travel of people to regions in which new strains and drug-resistant species appear as with religious tourism and medical treatment will help to disseminate the new infecting agents [26]. Also, this small area of the world was exposed to different terrorist waves, which has led to displacing people from their homes and, as a result, overcrowding and poverty in refugee camps. This may indicate the presence of 4.1% of Trichophyton infections related to Trichophyton soudanense, which is endemic to the sub-Saharan Africa region and only some sporadic cases are reported [27]. Lastly, the pandemic of COVID-19 that has recently affected the entire world will intensify the problem [28]. In addition to that, 74% of these chronic cases are in contact with farm work and animal domestication, which will facilitate the transmission of the pathogens.
CONCLUSION
In the last several years, difficult-to-treat dermatophyte infections have appeared in different parts of the world, including Iraq. There has been a similarity to factors encouraging the appearance of this epidemic-like infection. For this reason, extensive efforts are required to overcome this with further studies. Also, advanced molecular investigations are essential to discover new species and subspecies of dermatophytes.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Craddock LN, Schieke SM. Superficial fungal infection. In:Lowell A. Goldsmith, Stephen I. Katz, Barbara A. Gilchrest, Amy S. Paller, David J. Leffell, Klaus Wolff, editors. Fitzpatrick’s Dermatology in General Medicine. 8th ed. McGraw-Hill;2019. p 2925 – 2989.
2. Ajagopalan M, Inamadar A, Mittal A, Autar K, Miskeen, CR, Kabir S, et al. BMC Dermatology volume 1 Expert Consensus on The Management of Dermatophytosis in India (ECTODERM India). BMC Dermatol, 2018;18:6.
3. Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis:A comprehensive review. Indian Dermatol Online J. 2016;7:77-86.
4. AL-Khikani FH. Dermatophytosis a worldwide contiguous fungal infection:Growing challenge and few solutions. Biomed Biotechnol Res J. 2020;4:117-22.
5. Dogra S, Uprety S. The menace of chronic and recurrent dermatophytosis in India:Is the problem deeper than we perceive?Indian Dermatol Online J. 2016;7:73-6.
6. Erma SB, Panda S, Nenoff P, Singal A, Rudramurthy SM, Uhrlass S, et al. The unprecedented epidemic-like scenario of dermatophytosis in India:II. Diagnostic methods and taxonomical aspects. Indian J Dermatol Venereol Leprol. 2021;87:326-32.
7. Rengasamy M, Chellam J, Ganapati S. Systemic therapy of dermatophytosis:Practical and systematic approach. Clin Dermatol Rev. 2017;1:19-23.
8. Nenoff P, Verma SB, Ebert A, SüßA, Fischer E, Auerswald E, et al. Spread of terbinafine-resistant Trichophyton mentagrophytes type VIII (India) in Germany:“The tip of the iceberg?“J Fungi. 2020;6:207.
9. Shenoy MM, Kilaru G, Rasak A, Pinto A. Atypical dermatophytosis in a case of systemic lupus erythematosus. Our Dermatol Online. 2020;11:e165.1-e165.3
10. Osborne CS, Leitner I, Favre B, Ryder NS. Amino acid substitution in Trichophyton rubrum squalene epoxidase associated with resistance to terbinafine. Antimicrob Agents Chemother. 2005;49:2840-4.
11. Bishnoi A, Vinay K, Dogra S. Emergence of recalcitrant dermatophytosis in India. Lancet Infect Dis. 2018;18:250-1.
12. Collette JR, Lorenz MC. Mechanisms of immune evasion in fungal pathogens. Curr Opin Microbiol. 2011;14:668-75.
13. AL-Khikani FH, Ayit AS. Major challenges in dermatophytosis treatment:Current options and future visions. Egypt J Dermatol Venerol. 2021;41:1-9.
14. Monise FP, Abreu MH, Cantelli BAM, Segura GG, Nishimura FG, Bitencourt TA, et al. Epidemiology and diagnostic perspectives of dermatophytoses. J Fungi. 2020;6:310.
15. Pathania S, Rudramurthy SM, Narang T, Saikia UN, Dogra S. A prospective study of the epidemiological and clinical patterns of recurrent dermatophytosis at a tertiary care hospital in India. Indian J Dermatol Venereol Leprol. 2018;84:678-84.
16. Sharma R, Adhikari L, Sharma RL. Recurrent dermatophytosis:A rising problem in Sikkim, a Himalayan state of India. Indian J Pathol Microbiol. 2017;60:541-5.
17. James WD, Berger TG, Elastone DM. Diseases resulting from fungi and yeasts In:Andrews Diseases of the Skin:Clinical Dermatology.13th ed. Philadelphia. WB Saunders Company, 2020;291-324.
18. Bhatia VK, Sharma PC. Epidemiological studies on dermatophytosis in human patients in Himachal Pradesh, India. Springerplus. 2014;3:134.
19. Singh SK, Subba N, Tilak R. Efficacy of terbinafine and itraconazole in different doses and in combination in the treatment of tinea infection:A randomized controlled parallel group open labeled trial with clinic-mycological correlation. Indian J Dermatol. 2020;65:284-9.
20. Verma SB, Panda S, Nenoff P, Singal A, Rudramurthy SM, Uhrlass S, et al. The unprecedented epidemic-like scenario of dermatophytosis in India:I. Epidemiology, risk factors and clinical features. Indian J Dermatol Venereol Leprol. 2021;87:154-75.
21. Sheikh JS, Aaqib AS, Ilham I, Faizan Y, Iffat HS. Dermatophytosis:An epidemiological and clinical comparative study in a tertiary care centre. Int J Contemp Med. 2020;7:21-7.
22. Hanumanthappa H, Sarojini K, Shilpashree P, Muddapur SB. Clinicomycological study of 150 cases of dermatophytosis in a tertiary care hospital in South India. Indian J Dermatol. 2012;57:322-3.
23. De Freitas RS, Neves PS, Charbel CE, Criado PR, Nunes RS, Santos-Filho AM, et al. Investigation of superficial mycosis in cutaneous allergy patients using topical or systemic corticosteroids. Int J Dermatol. 2017;56:e194-8.
24. Nenoff P, Verma SB, Vasani R, Burmester A, Hipler UC, Wittig F, et al. The current Indian epidemic of superficial dermatophytosis due to Trichophyton mentagrophytes:A molecular study. Mycoses. 2019;62:336-56.
25. Shenoy MM, Jayaraman J. Epidemic of difficult-to-treat tinea in India:Current scenario, culpritscurbing strategies. Arch Med Health Sci. 2019;7:112-7.
26. Taghipour S, Shamsizadeh F, Pchelin IM, Rezaei-Matehhkolaei A, Mahmoudabadi AZ, Valadan R, et al. Emergence of terbinafine resistant Trichophyton mentagrophytes in Iran, harboring mutations in the squalene epoxidase (SQLE) gene. Infect Drug Resist. 2020:13:845-50.
27. Sahai S, Mishra D, Tripathi P. Rare isolation of Trichophyton soudanense from three cases of superficial mycoses in Lucknow, India. Indian J Pathol Microbiol. 2010;53:896-7.
28. Yaneva M, Demerdjieva Z, Darlenski R, Tsankov N. COVID-19 and skin:Analysis of the available data. Our Dermatol Online. 2020;11(Supp. 2):6-9.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-3688-6953 http://orcid.org/0000-0002-3688-6953 |






Comments are closed.