Folliculotropic mycosis fungoides treated with topical corticosteroids: A case report and a review of its trichoscopic features
Linda Manaa 1, Yosra Soua1, Ines Lahouel1, Marwa Thabouti1, Laila Njim2, Monia Youssef1, Hichem Belahdjali1, Jameleddine Zili1
1, Yosra Soua1, Ines Lahouel1, Marwa Thabouti1, Laila Njim2, Monia Youssef1, Hichem Belahdjali1, Jameleddine Zili1
1Dermatology Department, Fattouma Bourguiba Hospital, University of Medicine, Monastir, Tunisia, 2Anatomopathology Department, Fattouma Bourguiba Hospital, University of Medicine, Monastir, Tunisia
Corresponding author: Linda Manaa, MD
How to cite this article: Manaa L, Soua Y, Lahouel I, Thabouti M, Njim L, Youssef M, Belahdjali H, Zili J. Folliculotropic mycosis fungoides treated with topical corticosteroids: A case report and review of its trichoscopic features. Our Dermatol Online. 2022;13(1):111-113.
Submission: 08.06.2021; Acceptance: 14.10.2021
DOI: 10.7241/ourd.20221.31
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Folliculotropic mycosis fungoides (FMF) represents 5% of cutaneous lymphomas. It is a rare variant of mycosis fungoides that differs not only by its clinical and histological presentation but also by its prognosis.
It is characterized by an infiltrate of atypical lymphocytes in the perifollicular dermis and hair follicles, with or without mucinosis, while epidermotropism may be completely absent.
Dermoscopic and trichoscopic features in FMF are variable and not well defined.
Herein, we present a unique case of FMF in a female patient with scalp alopecia, which evolved well under topical treatment. We review its trichoscopic findings.
A 64-year-old female presented to our dermatology department with a seven-month history of an alopecic plaque on the scalp. No complaints of itching or burning were made. There was a history of arterial hypertension and dyslipidemia, which has been treated by oral medication. A physical examination revealed an erythematous, non-infiltrated, circumscribed alopecia in the frontal region of the scalp 8 cm in size associated with alopecia of the eyebrows (Fig. 1a and 1b).
 |
Figure 1: (a) Erythematous, circumscribed alopecia on the scalp; (b) alopecia of the eyebrows; (c) clinical improvement after two months. |
Trichoscopy showed a decreased number of pilosebaceous units, white scales, an erythematous background, and linear fine vessels (Fig. 2a and 2b).
 |
Figure 2: (a) Fine linear vessels and an erythematous background; (b) white scales and a decreased number of follicles. |
No other cutaneous lesions were evident. There were no other alopecic or infiltrated plaques, no hyperkeratosis or follicular papules, no acneiform lesions. A histopathological examination of a biopsy specimen revealed an epidermis covered with focally parakeratotic hyperkeratosis. The dermis contained a lymphocytic infiltrate in the follicles and the perifollicular areas. The hair follicles were dissociated by Alcian blue-positive edema. Folliculotropic infiltrate showed positive staining for CD3 and CD4. Some lymphocytes were CD20+ (Fig. 3a – 3c). The clinical, histological, and immunohistochemical appearance was consistent with the diagnosis of folliculotropic MF. Further examination showed no extracutaneous involvement. A full blood count and liver and kidney parameters were found to be in the normal range. A thoraco-abdomino-pelvic CT scan was without abnormality. Referring to the WHO/EORTC classification, the patient’s disease was stage IA. We initiated treatment with a high-potency topical corticosteroid with close monitoring. After two months of treatment, improvement was observed (Fig. 1c).
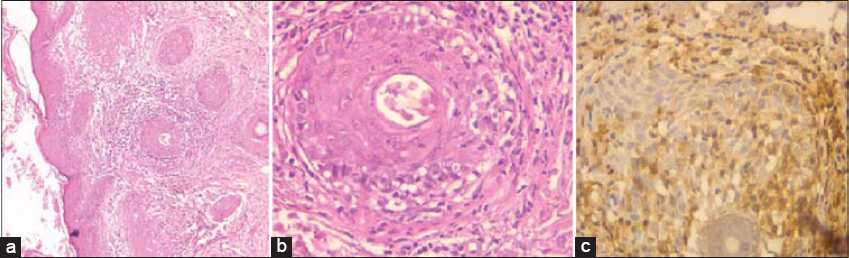 |
Figure 3: Lymphocytic infiltrate into the follicles and the perifollicular areas (a: H&E, 100×; b: H&E, 400×); (c) lymphocytes showing positive staining for CD4 (H&E, 400×). |
FMF presents a wide clinical spectrum. Alopecia is a typical manifestation of FMF occurring in up to 81% of patients [1]. The involvement of the scalp is not uncommon and may manifest itself by infiltrated inflammatory areas with hair loss, plaques mimicking alopecia areata, less frequently non-inflammatory scarring alopecia with comedo-like lesions [2,3].
Alopecic involvement of the eyebrows, as in our case, is highly characteristic in FMF and may present an early sign of the disease [1].
Several small studies have described dermoscopic patterns of MF and its variants. Dermoscopic features in FMF are heterogeneous, which goes together with the wide clinical spectrum of the disease. Numerous aspects have been described in the literature (Table 1).
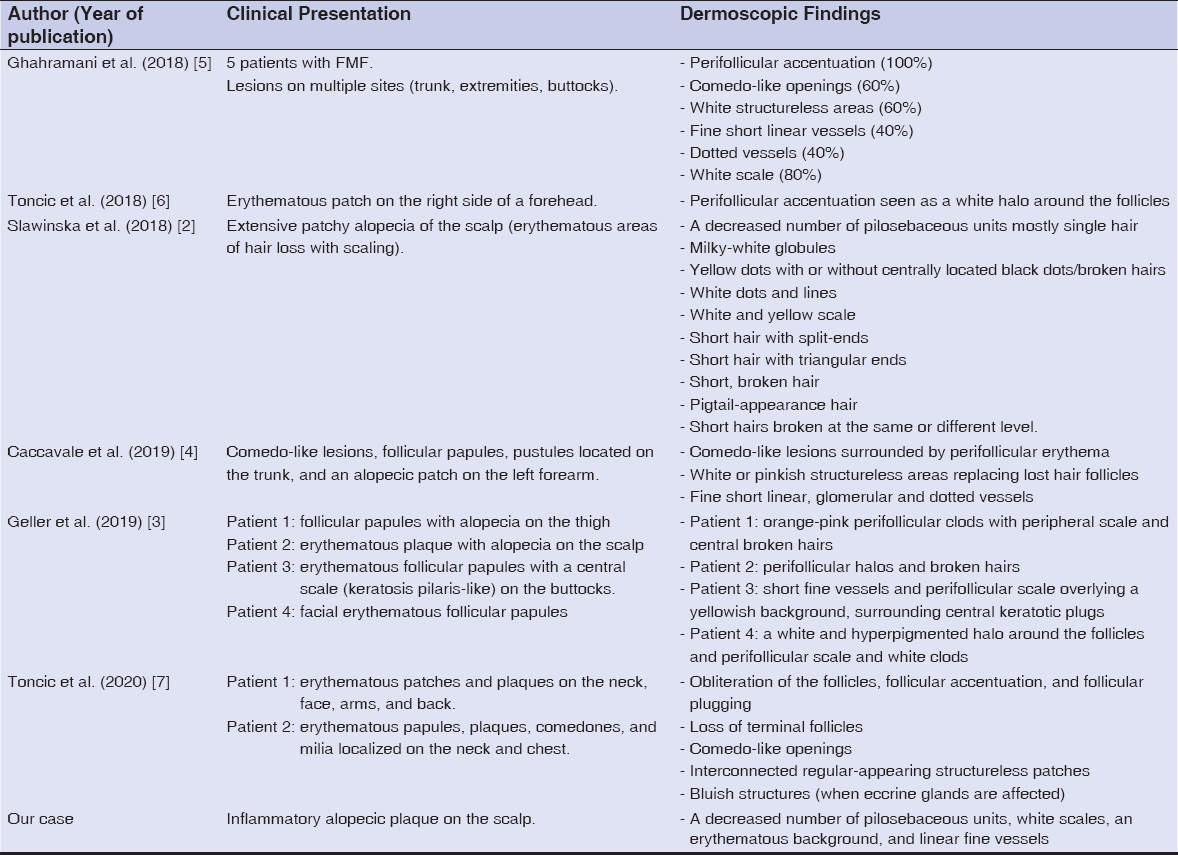 |
Table 1: Literatuare review of the dermoscopic features of FMF. |
Additional observations are needed to identify the trichoscopic spectrum of FMF allowing the differentiation with other diseases causing alopecia.
Recent studies have distinguished indolent (early-stage FMF) and more aggressive (advanced-stage FMF) subgroups [1,4]. This classification enabled the adaptation of treatment to each group and the use of less aggressive therapies in the first one.
According to this classification, our patient belonged to the first group, which shows a better response to less aggressive treatment regimens.
The management of FMF is not well defined and depends on its stage. Referring to the literature, local treatments rarely lead to complete remission. This may be attributed to the depth and location of the infiltrate.
In our patient, given the early stage of the disease, treatment with topical corticosteroids was sufficient to control the lesions.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Van Santen S, Roach REJ, van Doorn R, Horváth B, Bruijn MS, Sanders CJG, et al. Clinical Staging and Prognostic Factors in Folliculotropic Mycosis Fungoides. JAMA Dermatol. 2016;152:992-1000.
2. Sławińska M, Sobjanek M, Olszewska B, Nowicki R, Sokołowska-Wojdyło M. Trichoscopic spectrum of folliculotropic mycosis fungoides. J Eur Acad Dermatol Venereol. 2018;32:e107-8.
3. Geller S, Rishpon A, Myskowski PL. Dermoscopy in folliculotropic mycosis fungoides—A possible mimicker of follicle-based inflammatory and infectious disorders. J Am Acad Dermatol. 2019;81:e75-6.
4. Caccavale S, Vitiello P, Franco R, Panarese I, Ronchi A, Sica A, et al. Dermoscopic characterization of folliculotropic mycosis fungoides selectively localized on trunk and limbs. Int J Dermatol. 2019;58:e187-9.
5. Ghahramani GK, Goetz KE, Liu V. Dermoscopic characterization of cutaneous lymphomas:A pilot survey. Int J Dermatol. 2018;57:339-43.
6. Jurakic Toncic R, Ledic Drvar D, Bradamante M, Rados J, Jerkovic-Gulin S, Caccavale S, et al. Early dermoscopic sign of folliculotropism in patients with mycosis fungoides. Dermatol Pract Concept. 2018;8:328-9.
7. JurakićTončićR, RadošJ, ĆurkovićD, IlićI, Caccavale S, Bradamante M. Dermoscopy of syringotropic and folliculotropic mycosis fungoides. Dermatol Pract Concept. 2020;10:e2020069.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.