Penile porokeratosis mimicking annular lichen planus
Ngo Binh Trinh 1, Giang Huong Tran2, Hoang Trung Hieu3
1, Giang Huong Tran2, Hoang Trung Hieu3
1Department of Venereology, Ho Chi Minh City Hospital of Dermato-Venereology, Vietnam, 2Department of Pathology, University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam, 3Department of Dermatology, Ho Chi Minh City University of Medicine and Pharmacy, Vietnam
Corresponding author: Ngo Binh Trinh, MD
How to cite this article: Trinh NB, Tran GH, Hieu HT. Penile porokeratosis mimicking annular lichen planus. Our Dermatol Online. 2022;13(1):109-110.
Submission: 02.06.2021; Acceptance: 09.10.2021
DOI: 10.7241/ourd.20221.30
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Porokeratosis is a group of cutaneous diseases presented by epidermal keratinization [1]. Herein, we report the case of a patient with porokeratosis who responded well to carbon dioxide (CO2) laser therapy.
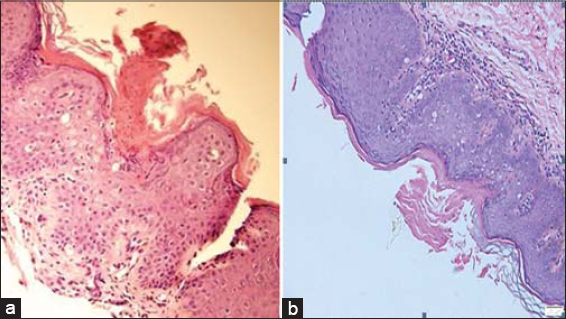
A 22-year-old Vietnamese male visited our department with an asymptomatic plaque on the penis present for three months. He denied a family history of similar lesions. A cutaneous examination of the penis revealed an annular, well-circumscribed plaque with slightly raised borders with scales (Fig. 1a). Other mucocutaneous lesions were absent. Fungal microscopy, a rapid plasma reagin (RPR) test, and a Treponema pallidum hemagglutination (TPHA) test were negative. Histological findings revealed a hyperkeratotic lesion with a discrete parakeratotic column. There was the presence of a cornoid lamella, which was a parakeratotic column overlying a small vertical zone of dyskeratotic and vacuolated cells within the epidermis (Fig. 2a). There was also a focal loss of the granular layer. A mild lymphocytic infiltrate could be seen around an increased number of capillaries in the underlying dermis (Fig. 2b).
CO2 laser removal was performed. There was no recurrence after a twelve-month follow-up (Fig. 1b). However, a hypopigmented scar was seen.
Porokeratosis is an uncommon disorder of keratinization with clinical variants, such as classical porokeratosis of Mibelli, disseminated superficial actinic porokeratosis, linear porokeratosis, and porokeratosis palmaris et plantaris disseminata [2].
Porokeratosis involving the genital areas and other adjacent sites is rare [2]. Genital porokeratosis was first described by Helfman in 1985 [3]. More than 69 cases have been reported in the literature [1].
The pathophysiology of genital porokeratosis remains unknown. It has been supposed that porokeratosis is linked to repeated minor frictional trauma. A benign lesion may transform into squamous cell carcinoma or basal cell carcinoma [4]. However, no malignant transformation of genital porokeratosis has been noted in the literature. Genital porokeratosis manifests itself clinically as classic or plaque-type porokeratosis of Mibelli [2].
Histological findings revealed a cornoid lamella with the absence of a granular layer and dyskeratotic cells in the upper spinous zone [2]. Our case may mimic some annular lesions, such as secondary syphilis, fungal infection, and annular lichen planus. Because a fungal examination and syphilis serology were negative, we could exclude fungal infection and annular secondary syphilis. The distinctive histology of porokeratosis such as a cornoid lamella with a decreased granular layer may help to differentiate between porokeratosis and annular lichen planus [4].
Numerous therapeutic methods of treatment exist, including surgical excision, CO2 laser, cryotherapy, topical retinoids, 5% 5-fluorouracil, vitamin D3 analogs, imiquimod cream, and 3% diclofenac gel [2,5].
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Bari O, Calame A, Marietti-Shepherd S, Barrio VR. Pediatric penile porokeratosis:A case report. Pediatr Dermatol. 2018;35:e103-e4.
2. Dongre A, Adhe V, Sanghavi S. Genital porokeratosis:a rare entity. Indian J Dermatol. 2013;58:81.
3. Helfman RJ, Poulos EG. Reticulated porokeratosis:A unique variant of porokeratosis. Arch Dermatol. 1985;121:1542-3.
4. Ahmed A, Hivnor C. A case of genital porokeratosis and review of literature. Indian J Dermatol. 2015;60:217.
5. Roge RP, Hajare SA, Mukhi JI, Singh RS. Genital porokeratosis:A report of two cases and review of literature. Indian J Dermatopathol Diagn Dermatol. 2020;7:19.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-3829-3115 http://orcid.org/0000-0002-3829-3115 |




Comments are closed.