Isolated pilomatricoma of the arm: A case and a review of the literature
Sara Bouabdella 1, Afaf Khouna1, Siham Dikhaye1,2, Nada Zizi1,2
1, Afaf Khouna1, Siham Dikhaye1,2, Nada Zizi1,2
1Department of Dermatology, Mohammed VI University Hospital of Oujda, Medical School of Oujda, Mohammed First University of Oujda, Morocco, 2Department of Epidemiology, Clinical Research and Public Health Laboratory, Medical School of Oujda, Mohammed First University of Oujda, Morocco
Corresponding author: Sara Bouabdella, MD
How to cite this article: Bouabdella S, Khouna A, Dikhaye S, Zizi N. Isolated pilomatricoma of the arm: A case and a review of the literature. Our Dermatol Online. 2022;13(1):86-88.
Submission: 15.01.2021; Acceptance: 17.05.2021
DOI: 10.7241/ourd.20221.21
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Pilomatricoma is a relatively rare tumor of the skin derived from primitive basal cells of the epidermis that differentiate into hair matrix cells. These tumors appear as solitary, firm nodules, showing a normal to pearl white epidermis. Its most frequent locations are the head and neck, while involvement of the upper extremities is relatively uncommon. Herein, we present the case of a seventeen-year-old female with pilomatricoma of the arm and review the literature regarding pilomatricomas of the upper extremities. The diagnosis of pilomatricoma is confirmed histologically and its treatment is based on surgical excision. Because of the low incidence and variable clinical presentation, pilomatricoma is a tumor not commonly suspected preoperatively. This presentation may help clinicians to diagnose this entity more effectively and decrease the rate of misdiagnosis.
Key words: Pilomatricoma; Adnexal tumor; Benign tumor
INTRODUCTION
Pilomatricoma is a relatively rare tumor of the skin derived from primitive basal cells of the epidermis that differentiate into hair matrix cells. Pilomatricoma comprises approx. 1% of all benign skin tumors [1]. Its most frequent locations are the head and the neck. Involvement of the limbs remains exceptional. Herein, we present the case of a seventeen-year-old female with unusual pilomatricoma, interesting for its location and size.
CASE REPORT
A seventeen-year-old female with a history of trauma presented with swelling of the anteroexternal aspect of the right arm evolving for the last three years. A clinical examination revealed a bluish lump of swelling, 3 cm in diameter, hard, painless, adherent to the skin, and movable relative to the deep plane (Fig. 1). The patient underwent a total excision of the tumor under local anesthesia. An anatomopathological study revealed intensely basophilic epithelial cells with hyperchromatic ovoid monomorphic nuclei showing mitoses and often mummified epithelial cells with a pale acidophilic phantom appearance with zones of acidophilic cells nucleated at the transition zones and the presence of calcifications (Figs. 2 and 3). The diagnosis of pilomatricoma was accepted.
 |
Figure 1: Pilomatricoma. |
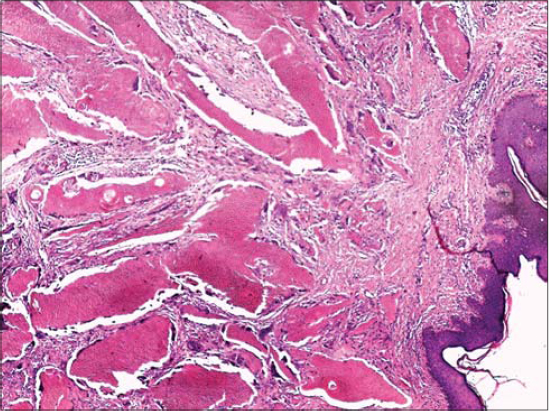 |
Figure 2: Proliferation of mummified beds in the dermis (H&E; 50×). |
 |
Figure 3: Proliferation of basaloid cell beds and mummified massifs (H&E; 50×). |
DISCUSSION
Pilomatricoma or calcifying epithelioma of Malherbe is a benign skin tumor [1], reported to be the most common cutaneous adnexal tumor in patients younger than twenty years old [2]. Most studies report a slight preponderance in females and this tumor seems to occur usually in Caucasians when compared with Asians and African-Americans [2]. Clinically, it manifests itself as a solitary, asymptomatic, benign, soft and friable to hard nodule, 0.5–5.0 cm in size. It is a slow-growing subcutaneous tumor that may or may not be attached to the skin and mobile over underlying structures. It may also present itself as multiple and in a nodular pattern in 2–10% of cases [3]. The stretching of the skin over the tumor shows the multifaceted “tent sign.” In addition, by pressing one edge of the lesion, the opposite edge protrudes like a “swing.” These two signs are pathognomonic of pilomatricoma. Its usual locations are the neck and head, and only several exceptional isolated locations on the limbs have been reported in the literature [4].
Calcification of the tumor is observed in 80% of cases, sometimes producing a true subcutaneous osteoma [4]. Its diagnosis is clinical and confirmed by histology, allowing to eliminate certain differential diagnoses, mainly epidermoid and pilar cysts, but especially malignant pilomatricoma.
Preceding trauma, as is the case of our patient, surgery, infection, an insect bite, and an intramuscular injection on the site of the tumor have been reported [4]. In general, pilomatricoma is not hereditary. Its etiology has been linked to mutations such as β-catenin and BCL2. Trisomy 18 has been shown to be a consistent feature in pilomatricoma [4]. Standard radiography is useful only if a significantly calcified pilomatricoma is suspected. An immunohistochemical study confirms the diagnosis [5].
Histologically, pilomatricoma is characterized by a mass composed of basaloid cells in the periphery, ghost cells in the center, calcification, and sometimes ossification. The ghost cells represent necrotic areas of previously vital basaloid cells. The calcification and ossification areas appear progressively in necrotic areas. Ghost cells are pathognomic of pilomatricoma [3].
Malignant transformation of pilomatricoma is, however, rare, and tends to occur in middle or old age [4]. The prognosis for pilomatricoma is generally good. Healing without recurrence is a rule after total surgical excision [5].
CONCLUSION
Pilomatricoma is a rare, benign, asymptomatic, and slow-growing skin tumor. The cervicofacial location and the female sex are the usual characteristics. Histological diagnosis will rule out a malignant pilomatricoma. The treatment to avoid recurrence is surgical excision.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. El Jouari O, Gallouj S, Douhi Z, Benkirane S, Baybay H, Mernissi FZ. A pregnancy pilomatricoma:An uncommon dermatologic benign neoplasm. Our Dermatol Online. 2018;9:425-7.
2. Harbaoui S, Youssef S, Ben Lagha I, Daadaa N, Jaber K, Dhaoui MR, et al. Multiple and giant perforating pilomatrixoma:A case report. Our Dermatol Online. 2018;9:299-301.
3. Arif T, Amin SS, Raj D. Pilomatricoma of the eyelid. Our Dermatol Online. 2017;9:73-4.
4. Corredor-Osorio R, Suarez-Tata M, Orellana ME. Pilomatricoma of the orbit. Our Dermatol Online. 2016;7:188-90.
5. Chan JJ, Tey HL. Multiple pilomatricomas:Case presentation and review of the literature. Dermatol Online J. 2010;16:2.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.