Does early acne intervention provide more than just a reduction in the incidence of scars? A review of the literature
Eastern Health, 8 Arnold Street, Box Hill, VIC, 3128, Australia
Corresponding author: Ayesha Vos, MD
How to cite this article: Vos A. Does early acne intervention provide more than just a reduction in the incidence of scars? A review of the literature. Our Dermatol Online. 2021;12(4):402-405.
Submission: 14.06.2021; Acceptance: 04.09.2021
DOI: 10.7241/ourd.20214.11
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: It is well established that early intervention in acne treatment reduces the incidence of scars. The purpose of this paper was to identify if early intervention in acne management also provides a cost benefit to the patient, reduces relapse rates or lessens the requirement for the treatment of acne scars.
Method: A systematic search of The Cochrane Library, MEDLINE and Cumulative Index to Nursing and Allied Health Literature (CINAHL) was performed independently by one reviewer using predefined criteria.
Results: Seven articles were identified from the literature – one systematic review, one review article and five expert opinion articles. Although data supports early intervention in acne management, no articles identified whether a cost benefit was also provided, if there was a reduction in the relapse rates or if there was a decreased requirement for the treatment of acne scars.
Conclusions: This review identifies an overall lack of published data regarding multiple outcomes for early intervention in acne and allows for the possible identification of areas where primary research would be beneficial.
Key words: Acne; early intervention; scarring; cost-benefit; relapse
INTRODUCTION
Acne is a disease of the pilosebaceous unit resulting in non-inflammatory lesions including microcomedones and comedones as well as inflammatory lesions comprising papules, pustules, nodules and cysts [1]. It is one of the three most common dermatoses in the world with up to 80-90% of people between the ages of 16 and 20 affected [2]. In severe cases, acne can lead to cutaneous scarring which in most cases, is permanent. The psychological scarring that can result from acne may also be profound [3]. There is thorough evidence to suggest that early initiation of treatment in acne, in particular with isotretinoin, may reduce the incidence and extent of acne scarring [4]. Pursuing early treatment of acne may prevent or reduce psychosocial problems such as issues with self-esteem, social withdrawal, depression and unemployment [5]. Extrapolation of US data shows that acne could be costing up to $100 million per year to the Australian community [6] with justification provided given the social, psychological and physical impacts of the condition. There is however, little research on whether early intervention reduces the overall costs of acne treatment and the need for the treatment of scarring. In addition, there also appears to be a lack of concrete knowledge of whether relapse rates of acne are reduced with early intervention. Given the prevalence and significant patient morbidity resulting from acne, it is vital that robust, good-quality research is completed in this area. This review aims to investigate whether early intervention in acne provides a cost-benefit to the patient, reduces the need for treatment of acne scarring and reduces relapse rates.
METHODS
A systematic search of The Cochrane Library, MEDLINE and Cumulative Index to Nursing and Allied Health Literature (CINAHL) was performed independently by one reviewer using predefined criteria. Key words used in each search engine included acne, early intervention, cost benefit, scarring and relapse. Inclusion criteria included primary research related to early intervention in acne, electronically published literature, articles written in the English language and articles from 1995 onwards. Exclusion criteria included primary research not relating to early intervention in acne, articles not written in the English language, articles published before 1995 and unpublished literature. A total of seven studies were included, which included one systematic review, one review article and five expert opinion articles. The full articles of all studies identified were analysed in depth and can be found in Table I.
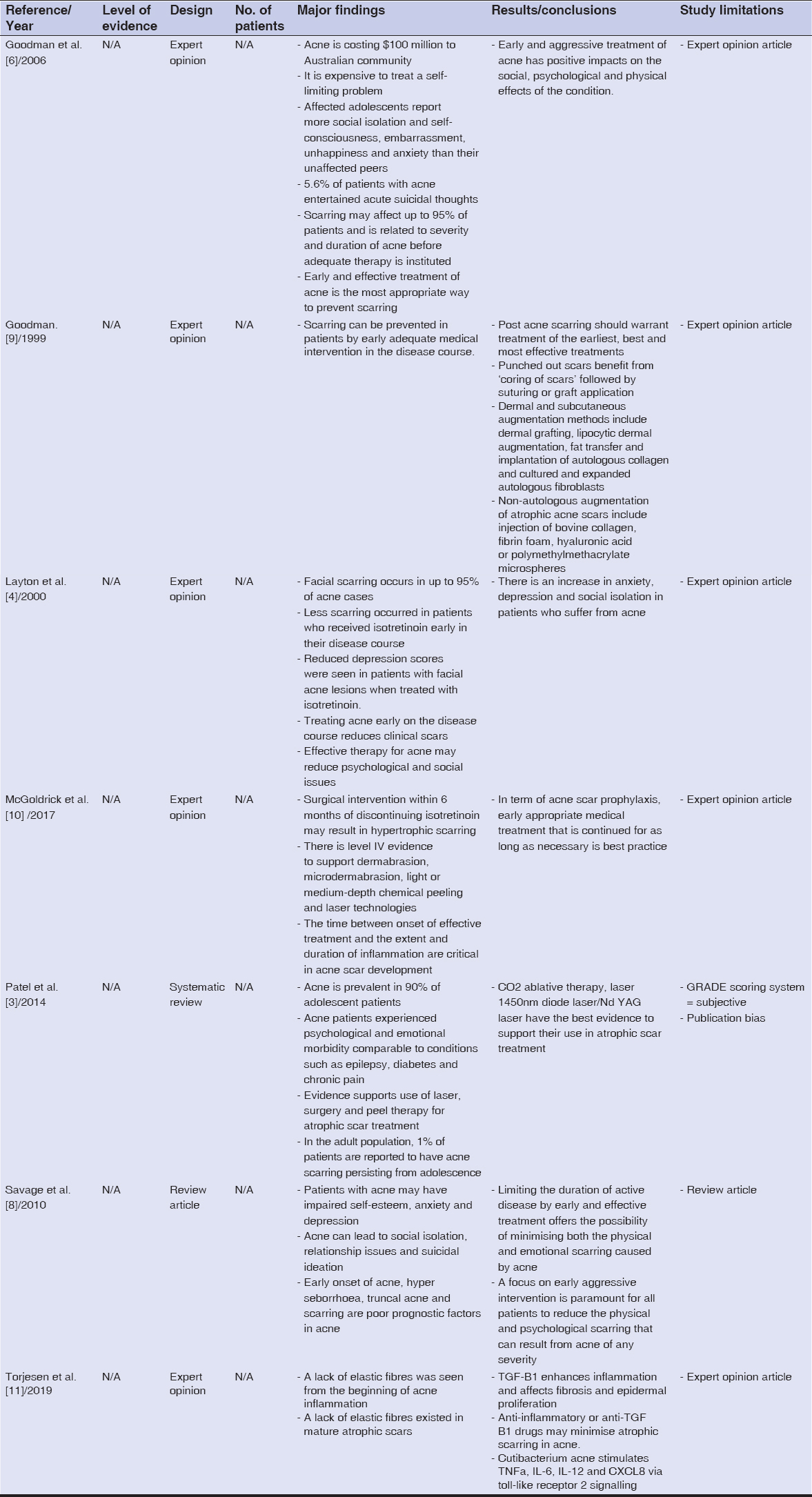 |
Table I: Analysis of articles |
RESULTS
One systematic review, one review article and five expert opinion articles were identified. Whilst ample data was identified to support early intervention in acne to reduce the incidence of scarring, there was no identifiable research found on whether early intervention reduces the need for the treatment of scarring. There was also no identifiable literature on whether early intervention in acne reduces relapse rates or whether it provides a cost benefit to the patient. Studies identified focussed on optimising acne management and patient education in order to reduce the incidence of acne scarring with Bonney et al. (2016) suggesting that acne outcomes can be improved when general practitioners are able to recognise acne scarring early [7]. Layton (2000) argues that isotretinoin instituted early on in the disease course can reduce both the physical and psychological scars that can result from acne [4]. There is evidence to suggest that optimisation of acne management should involve the use of both topical, systemic and localised therapies in order to minimise the development of acne scars [8]. There has also been extensive research performed on the treatment of atrophic scars, the most common form of scars found in patients with acne. Despite this, further research with randomised controlled trials is necessary to be able to provide sound evidence for the management of atrophic scars [3].
DISCUSSION
Despite comprehensively and systematically reviewing the literature in an attempt to address our research question, knowledge on various outcomes for early intervention in acne management are limited. Our research questions were not answerable using the literature. While there has been much research on the reduction in the incidence of scarring with early intervention, few researchers have delved into whether early intervention reduces the need for treatment of scars. Given the significant patient morbidity of acne, this points to the need for a study involving primary data collection in order to find an answer to whether or not early intervention in acne provides a cost benefit to the patient, reduces the need for treatment of acne scarring and reduces relapse rates. Limitations of our study include the small number of articles retrieved from which we are able to draw a firm conclusion as well as the fact that there is no best approach to comparing qualitative, quantitative and discussion papers. A publication bias was also noted as unpublished literature and literature not written in the English language were excluded. Other sources of limitations include unavailable and inaccessible data.
CONCLUSION
In summary, this review identifies an overall lack of published data regarding multiple outcomes for early intervention in acne and allows for the possible identification of areas where further primary research would be beneficial. Whilst it is known that isotretinoin, early optimisation of acne management and patient education can reduce the incidence of both the physical and psychological scars of acne, more research needs to be conducted to identify whether early intervention in acne provides a direct cost-benefit to the patient, reduces the need for the treatment of acne scarring and reduces relapse rates.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Ramasamy S, Barnard E, Dawson TL, Li H. The role of the skin microbiota in acne pathophysiology. Br J Dermatol. 2019;181:691-9.
2. Bagatin E, Costa CS. The use of isotretinoin for acne – an update on optimal dosing, surveillance, and adverse effects. Expert Rev Clin Pharmacol. 2020;13:885-97.
3. Patel L, McGrouther D, Chakrabarty K. Evaluating evidence for atrophic scarring treatment modalities. JRSM Open. 2014;5:1-13.
4. Layton A. Acne scarring –reviewing the need for early treatment of acne. J Dermatol Treat. 2000;11:3-6.
5. Paravina M, StepanovićM, Štilet P, SpasićDJ. Acne vulgaris – Adequate and timely therapy as an early prevention of psychological disturbances. Med Biol. 2019;21:76-80.
6. Goodman G. Acne and acne scarring:the case for active and early intervention. Aust Fam Physician. 2006;35:503-4.
7. Bonney AD, Mullan J, See J, Rayner JE, Hammond A. Investigating GP experiences:Barriers and facilitators to the management and referral of acne patients in a primary care setting. Research Online. 2016;1:1.
8. Savage LJ, Layton AM. Treating acne vulgaris:systemic, local and combination therapy. Expert Rev Clin Pharmacol. 2010;3:563-80.
9. Goodman GJ. Acne and acne scarring:why should we treat?. Med J Aust. 1999;171:62-3.
10. McGoldrick RB, Theodorakopoulou E, Azzopardi EA, Murison M. Lasers and ancillary treatments for scar management Part 2:Keloid, hypertrophic, pigmented and acne scars. Scars Burn Heal. 2017;3:1-16.
11. Torjesen I. Early acne intervention may prevent later scarring. Dermatol Times. 2019;40:27.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.