Heat dermabrasion of congenital nevi as a simple, innovative technique
Khalifa Sharquie 1, Raed I Jabbar2
1, Raed I Jabbar2
1Department of Dermatology, College of Medicine, University of Baghdad, Medical City Teaching Hospital, Baghdad, Iraq, 2Department of Dermatology, Fallujah Teaching Hospital, Al-Anbar Health Directorate, Anbar, Iraq
Corresponding author: Prof. Khalifa E Sharquie, MD PhD
How to cite this article: Sharquie K, Jabbar RI. Heat dermabrasion of congenital nevi as a simple, innovative technique. Our Dermatol Online. 2021;12(3):262-266.
Submission: 05.02.2021; Acceptance: 07.05.2021
DOI: 10.7241/ourd.20213.6
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Congenital nevi are a relatively common dermatological problem that carries a risk of malignant transformation.
Patients and Methods: The following is an interventional study in which five patients with congenital melanocytic nevi were enrolled, 3 (60%) females and 2 (40%) males. After local anesthesia, heat dermabrasion was performed with a diathermal needle until complete debulking was achieved and bleeding points appeared. Follow-up was done every two months for four months.
Results: The location of the nevi in all cases was the face, while the size was variable, ranging from 1 to 17 cm.Erythema was observed on the sites of the removed nevi after two weeks and then gradually went to normal during the follow-up period, leaving minimal scarring. Complications were absent and no relapses were observed during the follow-up period.
Conclusion: This is a simple, easy, and innovative technique that employs heat dermabrasion and, thus, avoids excision and suturing with or without grafting or flaps.
Key words: Congenital melanocytic nevus; Heat dermabrasion; Malignant melanoma
INTRODUCTION
Congenital melanocytic nevi (CMN) are either present at birth or appear in the first several weeks of life, with an incidence of 1% to 2% in newborns [1]. They consist of benign proliferations of neural-crest cell-derived melanocytes [2], and no significant gender predilection has been demonstrated. CMNs occur most commonly on the trunk and extremities, although scalp and facial involvement is seen as well. For practical purposes, small congenital nevi are at most 1.5 cm in diameter, medium-sized congenital nevi are 1.5 to 20 cm in diameter, large congenital nevi are 20 to 40 cm in diameter, and giant congenital nevi are more than 40 cm in diameter [2].
Small and medium-sized CMNs are usually round or oval. These lesions are usually slightly elevated at birth and may be brown. They may or may not be associated with hypertrichosis [3].
CMNs may be a great burden and reduce the patient’s quality of life due to their cosmetic appearance [4]. Moreover, there is an increased risk of developing malignant melanoma (MM) in patients with CMN, especially with larger CMNs [5]. Large and giant lesions have a high risk of developing MM, but small and medium-sized lesions have a lower risk. Previously, the lifetime risk of MM in patients with CMN was estimated to be up to 40% in giant CMNs [1], but more recent studies indicate an overall lower incidence with CMN, at about 0.7% to 2.9% [6,7].
The treatment of CMNs is primarily based on two factors: their cosmetically disfiguring appearance and the increased risk of progression to melanoma. The decision to remove a CMN is on an individual basis and depends on the age of the patient, the risk of melanoma, the anatomic location, the anticipated cosmetic outcome, the presence or absence of neurocutaneous melanosis, and the complexity of removal [3].
In the last century, complete nevus excision had been the first choice of management to reduce the risk of malignant transformation [8]. However, excision has not been proven to reduce the risk of melanoma [9]. In the past, dermabrasion was sometimes performed, resulting in a less elevated and more lightly pigmented CMN [3].
Lasers such as Q-switched ruby, Q-switched alexandrite, carbon dioxide (CO2) have also been used to treat CMNs, but the recurrence of pigmentation is an issue because of the persistence of the nevus cells [10].
Laser devices are utilized for epidermal and dermal pigmented skin diseases [11,12], and these devices may be categorized into ablative and pigment-specific [13]. The management of CMNs with lasers, however, remains controversial, mainly because of the absence of evidence on their efficacy and safety concerns. Some state that lasers may decrease the risk of malignancy by reducing the melanocytic mass, while others are concerned about the potential carcinogenic risk of sublethal laser damage [9,14].
A novel and safe technique known as heat dermabrasion with a diathermal needle was introduced by Sharquie for the treatment of different types of acne scarring and nose volumeplasty for a bulky nose under local anesthesia in one session with minimal or no adverse effects, and proved its safety [15–19].
The aim of the present study was to find a new and easy technique for the removal of congenital nevi, which thus avoids excision and possible grafting or flaps.
PATIENTS AND METHODS
The following was a prospective, interventional, surgical procedure in which five patients with a CMN were treated during the period from January 2013 through October 2018—3 (60%) females and 2 (40%) males. Their age ranged from 5 to 16 years with a mean of 12 years.
A proper history was taken, including the sex and age, the duration of disease and the age of onset, the associated symptoms, and the past medical and drug history.
A full clinical examination was performed to identify the site, size, color, and associated signs.
The study followed the principles of the Declaration of Helsinki and a formal written consent was obtained from each patient’s parents before the surgical procedure, after explaining in full the method of intervention, possible complications, follow-up, prognosis, and need for before-and-after treatment photographs at the same place, at a constant distance, and in the same lighting.
The patients were prepared by cleaning the site of the nevus and the adjacent area with 70% alcohol, waiting several minutes until it dried, then moving an impregnated gauze with normal saline repeatedly over the same area in different directions for further cleaning and sterilization. After local anesthesia, heat dermabrasion was performed with a diathermal needle until complete debulking was achieved and bleeding points appeared. Topical povidone was applied twice daily with oral antibiotics to be seen after two weeks. Then, follow-up visits were scheduled for every two months for four months.
The patient’s satisfaction with the response after the treatment was assessed as follows: 1) full satisfaction, 2) partial satisfaction, 3) no satisfaction.
Data was described statistically in terms of range, mean, frequency (no. of cases), percentage (%), and male-to-female ratio.
RESULTS
The location of the nevi in all cases was the face and the size was variable, ranging from 1 to 17 cm. (Table 1).
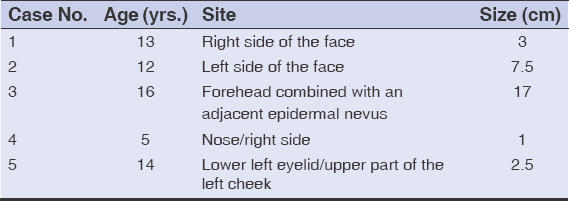 |
Table 1: The age of the patient and the site and size of the CMN |
In 4 (80%) cases, there was a complete clearance of hyperpigmentation after heat diathermy, while, in one patient, there was a marked reduction in hyperpigmentation, but not a complete clearance of the largest. Nonetheless, the hair density in the treated nevus was reduced.
No important side effects apart from mild pain, transient edema, and crust formation were observed at the end of two weeks of the treatment session.
Erythema was observed at the sites of nevi after two weeks and then gradually went to normal during four months of follow-up, leaving minimal scarring. No relapses were observed during the follow-up period and no further patient visits to the treating doctor to record any complications or relapses. Repigmentation was not noted during the follow-up period. In one patient, who was a relative to the treating doctor, the follow-up period was around five years with no relapses or complications. In all patients, there were marked cosmetic results and full satisfaction was achieved in all patients.
Figs. 1 –2 show photos of the patients prior to the session, at the end of the session, and during the follow-up period. While one patient showed CMN on the forehead superimposed and neighboring epidermal nevus (Fig.3).
DISCUSSION
Numerous methods and techniques to treat CMNs exist. One early is surgical excision. Complete nevus excision has been used to reduce the risk of malignancy [8]. However, surgical excision has not been proven to decrease the risk of MM [9]. Furthermore, CMNs may be too large to be completely removed with surgery, and excision may lead to unwanted cosmetic results, such as scarring and restrictions in joint mobility [9]. Besides, surgical excision is costly and requires experience in nevus excision, grafting may be needed, especially in large and giant CMNs, and general anesthesia may sometimes be required. As with any surgical intervention, the possible complications involved with surgical excision need to be considered, such as bleeding, infection, and the risks entailed by general anesthesia.
Mechanical dermabrasion has sometimes been performed in the treatment of CMNs [3]. This technique might be effective but often requires general anesthesia, especially with large nevi. Also, the procedure is bloody and messy, as using a brush causes blood contamination to the surroundings, possibly leading to the transmission of infection from the patient to medical staff. The post-dermabrasion area is usually tender, thinner, and more fragile, and repigmentation may occur [20,21].
Although Q-switched, CO2, and other lasers have also been used in the treatment of CMNs, they are also risky. A laser is costly and requires protection for the doctor’s and the patient’s eyes, considerable experience, numerous sessions to achieve the final, cosmetically acceptable outcome. The use of lasers for the management of CMNs remains controversial, mainly because of the absence of evidence on their efficacy and safety concerns [9,14]. Pigment lasers have been shown to bear a high rate of repigmentation, in up to 54% of patients. Also, ablative lasers are associated with a high incidence of complications, such as hypopigmentation and hypertrophic scarring [22]. Even then, the use of heat dermabrasion as an innovative technique in the present work produced only mild scarring during the follow-up period and gave a satisfactory cosmetic appearance, with full patient satisfaction during one session.
Heat dermabrasion is a safe technique, as it was used in the treatment of facial acne scarring in 250 patients with 35% TCA peeling, and no complications such as hypertrophic scars or keloids as the face skin is rich in skin appendages such as hair follicles and sebaceous glands. Nevertheless, one should be cautious of the chin and mandibular areas as these show a more marked tendency for scarring [23]. Still, to achieve minimal scarring after congenital nevi, heat dermabrasion would be more acceptable than excision and suturing or excision and grafting. This new technique is also safer and less costly than an ablative laser or mechanical dermabrasion [9,14,20–22].
No patient had a nevus recurring or complications such as hypertrophic scars or keloids after the follow-up period.
The limitations of this study were a small number of cases and a limited follow-up period. Therefore, more clinical data and lengthened follow-up periods are required to prove the safety of this novel treatment and record any possible relapses.
CONCLUSION
This is a simple, easy, non-costly, innovative technique that uses heat dermabrasion to treat small and medium-sized CMNs, avoiding excision and suturing with or without grafting or flaps. The heat of diathermy removes most or all residual melanocytes that could not be cleared by dermabrasion. Neither complications nor relapses were observed during our follow up-period.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Alikhan A, Ibrahimi OA, Eisen DB. Congenital melanocytic nevi:Where are we now?Part I. Clinical presentation, epidemiology, pathogenesis, histology, malignant transformation, and neurocutaneous melanosis. J Am Acad Dermatol. 2012;67:495e1-17;quiz 512-4.
2. Krengel S, Scope A, Dusza SW, Vonthein R, Marghoob AA. New recommendations for the categorization of cutaneous features of congenital melanocytic nevi. J Am Acad Dermatol. 2013;68:441-51.
3. Palin S J, Barhill R L . Benign Melanocytic Neoplasms . In:Bolognia J L, Sccaffer J V, Ceroni L. Text book of dermatology , 4th edition. China, Elsevir , 2018;18,112:1976-1980.
4. Masnari O, Neuhaus K, Aegerter T, Reynolds S, Schiestle C M, Landolt MA. Pediatric of health-related quality of life and psychological adjustment in children and adolescent with congenital melanocytic nevi:analysis of parent reports. J Pediatr Psychol.2019;44:714-725.
5. Viana ACL, Gontijo B, Goulart EMA, Bittencourt FV. A prospective study of patients with large congenital melanocytic nevi and the risk of melanoma. An Bras Dermatol. 2017;92:200-5.
6. Vourc’h-Jourdain M, Martin L, Barbarot S, Barbarot S, aRED. Large congenital melanocytic nevi:Therapeutic management and melanoma risk:A systematic review. J Am Acad Dermatol. 2013;68:493-8.e1-14.
7. Kinsler VA, Hare PO, Bulstrode N, Calonje JE, Chong WK, Hargrave D, et al. Melanoma in congenital melanocytic naevi. Br J Dermatol. 2017;176:1131-43.
8. Arad E, Zuker RM. The shifting paradigm in the management of giant congenital melanocytic nevi:Review and clinical applications. Plast Reconstr Surg. 2014;133:367-76.
9. Ibrahimi OA, Alikhan A, Eisen DB. Congenital melanocytic nevi:Where are we now?Part II. Treatment options and approach to treatment. J Am Acad Dermatol. 2012;67:515.e1-13;quiz 28-30.
10. Kishi K, Okabe K, Ninomiya R, Konno E, Hattori N, Katsube K, et al. Early serial Q-switched ruby laser therapy for medium-sized to giant congenital melanocytic naevi. Br J Dermatol. 2009;161:345-52.
11. Momen S, Mallipeddi R, Al-Niaimi F. The use of lasers in Becker’s naevus:An evidence- based review. J Cosmet Laser Ther. 2016;18:188-92.
12. Shah VV, Bray FN, Aldahan AS, Mlacker S, Nouri K. Lasers and nevus of Ota:A comprehensive review. Lasers Med Sci. 2016;31:179-85.
13. Arora H, Falto-Aizpurua L, Chacon A, Griffith R D, Nouri K. Lasers for nevi:A review. Lasers Med Sci. 2015;30:1991-2001.
14. Eggen A M, Lommerts JE, Van Zuuren EJ, Limpens J, Pasmans SGMA, Wolkerstorfer A. Laser treatment of congenital melanocytic nevi:A systemic review. Br J Dermatol. 2018;178:369-83.
15. Sharquie KE. Heat dermabrasion of different types of scars. IMCAS 2018. http://www.imcas.com.
16. Sharquie KE. Nose volumeplasty. IMCAS 2019;https://www.imcas.com/en/attend/imcas-world-congress-2019.
17. Sharquie KE. Iraqi society of dermatology activities. https://www.imcas.com/en/attend/imcas-world-congress-2019.
18. Sharquie KE. Pearls in skin surgery and cosmetology 2019 28th EADV Madrid.eadvprogram.manage.com en-GB.
19. Sharquie KE, Al-Jaralla FA. Volumeplasty of bulky nose using heat dermabrasion as a minor therapy. American Journal of Dermatological Research and Reviews. 2020;3:18.
20. Bohn J, Svensson H, Aberg M. Dermabrasion of large congenital melanocytic naevi in Neonates. Scand J Plast Reconstr Surg Hand Surg. 2000;34:321-6.
21. Kishi K, Matsuda N, Kubota Y, Katsube KI, Imanishia` N, Nakajima T. Rapid, severe repigmentation of congenital melanocytes naevi after curettage and dermabrasion:Histological features. Br J Dermatol. 2007;156:1251-7.
22. Bray FN, Shah V, Nouri K. Laser treatment of congenital melanocytic nevi:A review of the literature. Lasers Med Sci. 2016;31:197-204.
23. Sharquie KE, Jabbar RI. Heat dermabrasion using diathermy needle combined with TCA (35%) peeling as innovative therapy for acne scarring in patients with dark complexion. Our Dermatol Online. 2021:1-8(In publication list).
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-0265-2040 http://orcid.org/0000-0002-0265-2040 http://orcid.org/0000-0001-5197-4786 http://orcid.org/0000-0001-5197-4786 |






Comments are closed.