Hospital prevalence and causes of non-adherence to acne treatment: A report from Nepal
Suchana Marahatta 1, Urvi Shrestha2
1, Urvi Shrestha2
1Department of Dermatology & Venereology, Co-ordinator (MBBS-Phase II), B.P. Koirala Institute of Health Sciences, Dharan, Nepal, 2Department of Intern, B.P. Koirala Institute of Health Sciences, Dharan, Nepal
Corresponding author: Suchana Marahatta, MD
How to cite this article: Marahatta S, Shrestha U. Hospital prevalence and causes of non-adherence to acne treatment: A report from Nepal. Our Dermatol Online. 2021;12(3):251-256.
Submission: 18.11.2020; Acceptance: 21.02.2021
DOI: 10.7241/ourd.20213.4
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: With acne being a chronic and relapsing condition, patients may not be compliant with its treatment, especially because of the various reasons leading to treatment failure. This study aimed to determine the hospital prevalence and causes of non-adherence to acne treatment among patients attending the dermatology outpatient department of a tertiary care hospital in eastern Nepal.
Materials and Methods: This was a cross-sectional study conducted from April 22 through May 20, 2017, and was based on a preset proforma distributed among the attendees at the dermatology OPD of BPKIHS, Dharan, Nepal. A validated questionnaire was used to ascertain the patient’s non-adherence to acne treatment. If non-adherence was confirmed, sociodemographic details, along with a detailed history of the illness, including the duration of the illness, the age of onset, and the examination findings, were noted in the proforma.
Results: The study found the hospital prevalence of non-adherence to acne treatment to be 61.76%. The majority of the non-adherent patients were females 10–20 years old. In 76.8% of the cases, both oral and topical treatment was prescribed, and both modes of treatment were abandoned by a majority of the participants (56.5%). Failing to remember to take the medications at the right time (45.7%), being unaware of the necessity of their continuation (34.8%), and the appearance of their side effects (28.3%) were the three most prevalent reasons for abandoning the prescribed treatment.
Conclusion: Greater non-compliance was observed in patients taking both oral and topical medications. Among the different reasons for non-compliance, failing to remember to take the medications and being unaware of the necessity of their continuation were the two most prevalent answers. Hence, educating patients on the importance of treatment adherence seems to be of great value in minimizing non-compliance.
Key words: Acne vulgaris; Adverse effect; Education; Medication adherence; Nepal; Treatment
INTRODUCTION
Acne is a very common non-infectious skin condition frequently encountered in dermatological practice [1]. The Global Burden of Disease (GBD) project estimates the prevalence of acne at 9.4%, ranking it as the eighth most prevalent disease in the world [2]. In a study conducted in rural Nepal, the point prevalence of acne was found to be 7.7% [3]. Likewise, in a report from western Nepal, the prevalence among the pediatric age group was found to be 10.1% [4].
Different treatment modalities may be employed for acne, such as topical retinoids, antibiotics, benzoyl peroxide, alpha hydroxy acid, azelaic acid, niacinamide, hydrogen peroxide, anti-seborrheic medications. Some commonly prescribed systemic treatments are antibiotics, retinoids, and hormonal treatments [5]. Additionally, estrogen levels tend to be found low in females with acne, thus further supporting the role of hormonal therapy in the treatment of acne [6].
Adherence is the extent to which a patient follows agreed-on treatment recommendations. Non-adherence may be classified into primary non-adherence – failure to obtain and initiate the treatment – and secondary non-adherence – failure to abide by the procedure of the treatment or discontinuing the treatment too early. Non-adherence is a pervasive problem in all fields of medicine, particularly in treating chronic conditions. Chronic conditions, including acne, show low secondary adherence rates because patients often miss doses and discontinue treatments [7]. Due to non-compliance, the treatment outcome will be less than optimum. Hence, the patient may experience frustration, resignation, and a lower quality of life. It is, therefore, becoming increasingly imperative that the factors associated with non-adherence to acne treatment must be assessed to devise alternatives and strategies to improve the patient’s compliance toward the advised medical treatment.
MATERIALS AND METHODS
This was a cross-sectional study that aimed to determine the hospital prevalence of non-adherence to acne treatment and the reasons behind the non-adherence in acne patients attending the dermatology outpatient department of B.P. Koirala Institute of Health Sciences. The study was carried out from April 22 through May 20, 2017. All subjects with the diagnosis of acne vulgaris with non-adherence to treatment were included in the study after informed consent. A validated ECOB questionnaire was employed to ascertain the patient’s non-adherence to acne treatment [8]. Excluded were patients seeking acne treatment for the first time, those compliant with the prescribed treatment, and those unwilling to participate in the study. The study was conducted according to the declaration of Helsinki. Sociodemographic details, along with a detailed history of the illness, including the duration of the illness, the age of onset, and the examination findings, were noted in the proforma. Acne was classified into four grades (grade I, II, III, and IV) according to the pleomorphic grading system [9]. The study employed purposive sampling. Data entry was performed with Microsoft Excel. Analysis was performed with SPSS, version 11.5. Descriptive statistics was employed to explore the characteristics of the collected data by calculating percentages, means, ranges, and standard deviations. Ethical clearance was obtained from the Departmental Research Unit.
LIMITATIONS
In the ECOB questionnaire, the color of the medication packaging is accepted as a correct answer to the question: “Do you remember the name of the last drugs you took?” However, since there may be more than one manufacturer of the same drug, this answer could not be accepted. Since the details of the adherent patients have not been taken, bivariate and multivariate analysis could not be performed. Since the study was cross-sectional, causal inferences could not be made. A study with a longer duration, a follow-up period, and bigger sample sizes may generate more details. Inclusion of other widely recognized adherence scales, such as the Morisky Medical Adherence Scale or the Medication Event Monitoring System may help to better determine the extent of adherence.
RESULTS
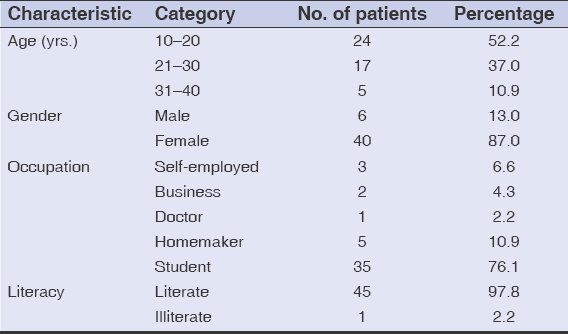
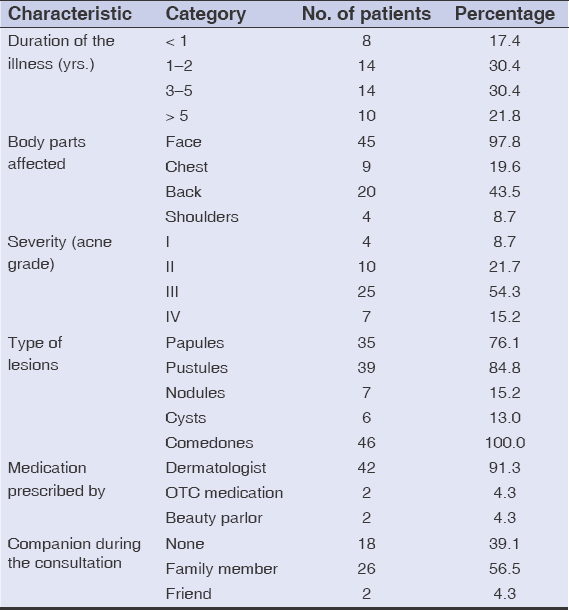
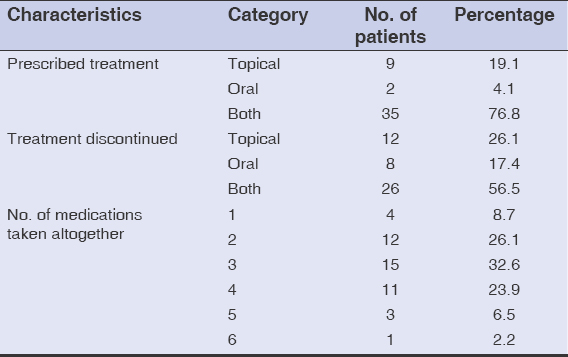
During the study, a total of 68 acne patients visited the dermatology OPD. Among them, 42 fulfilled the criteria for non-adherence to acne treatment, hence giving a hospital prevalence of 61.76%. More than half of them (52.2%) were 10–20 years old, with a mean age of 21.3 ± 5.8 years. The majority (87.0%) of the participants were females (Table 1). Non-adherence was the highest (82.6%) among participants suffering from acne for more than a year. The face was the most commonly (97.8%) affected site. More than half of the participants (54.3%) had grade III acne. Comedones were found unanimously in all 46 participants, while pustules were predominant among 84.8% of the participants. In 91.3% of cases, medications were prescribed by a dermatologist. More than half (56.5%) had a family member as their companion during the consultation (Table 2). For 76.8%, both oral and topical treatments were prescribed, and both modes of treatment were abandoned by a majority of the participants (56.5%) (Table 3). Among the numerous reasons enumerated in the proforma, failing to remember to take the medications at the right time (45.7%), being unaware of the necessity of their continuation (34.8%), and the appearance of their side effects (28.3%) were the three most prevalent reasons for abandoning the prescribed treatment (Table 4). Itching (17.3%) was the most frequently encountered side effect among the participants who claimed to have abandoned the prescribed treatment because of the side effects of the medications. Half (50.0%) claimed there was no difference in their condition when the treatment was withdrawn. A majority (71.7%) used no alternative treatments after abandoning the prescribed treatment for acne, while the rest (28.3%) resorted to beauty products such as moisturizers and cleansers (Table 5).
DISCUSSION
Acne affects prepubescents and teenagers as well as adults, and may have devastating impact on one’s mental and social well-being. Those who seek help for their acne not only do so because of the severity of the disease but also because of the sociocultural factors and the disease’s impact on other people’s attitude toward and perception of them. This is also determined by their coping capacity. Compliance with the prescribed treatment regimen is an essential element in the overall effectiveness of the therapy [10]. According to our study, the rate of non-adherence to acne treatment was found to be 62.16%, which is quite similar to a cross-sectional study done on 500 patients with acne vulgaris, in whom poor adherence was found in 64.4% of cases [11]. In a similar fashion, an international observational study on acne treatment found the overall risk of poor adherence to be 50%, with regional variations of 43% in the Americas, 48% in Asia, and 58% in Europe. Unlike this report, the higher rate of non-adherence in our study might be correlated with the ease of directly contacting a dermatologist in Nepal, so that, in case of a disease flare, they are able to immediately visit the specialist again. Likewise, the considerable availability of over-the-counter medications in Nepal might be another reason for the higher non-adherence. Hence, the patients might not have been taking the treatment seriously enough. Yentzer et al. highlighted that acne treatment compliance is only about 50% in a non-clinical trial setup, but may increase in clinical trials. They found maximum compliance among the frequently followed-up group. However, a daily electronic reminder and a parental reminder did not improve compliance [12]. This suggests that frequent visits to the doctor may influence and encourage the patient to adhere to the treatment.
Most of the studies assessed adherence with a validated ECOB questionnaire. Its advantages are as follows: may be employed easily in routine clinical practice; may readily be adapted to other languages; and may even be taken by children younger than 15 years [8,13]. In a study conducted in Japan, there was an overall rate of poor adherence in 76% of the participants [14].
In our study, 52.2% of the participants were 10–20 years old, with a mean age of 21.3 ± 5.8 years. The majority (87.0%) were females. Almost all were literate (97.8%), with more than half of all participants having attended higher secondary education (60.9%). This finding is comparable with a study by Dréno et al., who have also shown that poor adherence was independently correlated with a young age, most visibly in patients less than 15 years old as well as 15–25 years old [13].
What our study shows is that both modes of treatment (oral and topical) were abandoned by a majority of the participants (56.5%). This is in contrast with a study conducted in France, which showed an 81% adherence rate to one or both modes of acne treatment [8]. According to a past review, adherence was higher for oral treatments than topical. The authors concluded that frequent office visits and web-based educational tools may significantly improve adherence to acne treatment [15]. In a study conducted in the U.S., the adherence rates with topical antibiotics were determined at 4.04%, retinoids at 57.28%, contraceptives at 48.99%, glucocorticoids at 1.64%, while the adherence rates with oral antibiotics were determined at 3.89%, retinoids at 2.29%, and glucocorticoids at 1.98% [16]. In a more recent study on adherence to topical acne treatments, discontinuation occurred mostly with the use of retinoids (40%), benzoyl peroxide combinations (44.1%), and retinoid combinations (60%). Furthermore, the discontinuation of these treatments was reported to have been due to side effects, with rates of 50%, 33.3%, and 65.7%, respectively [17]. Likewise, a previous report showed that a complex treatment regimen, lack of a response, side effects, lack of time, forgetfulness, inconvenience, and others were common reasons for secondary non-adherence to acne therapy [10]
In our study, failing to remember to take the medications at the right time (45.7%), being unaware of the necessity of their continuation (34.5%), the appearance of their side effects (28.3%), and no improvement with the medications taken (26.1%) were the most prevalent reasons for abandoning the prescribed treatment. Likewise, 91.3% of the participants were prescribed the treatment by a dermatologist, more than half (56.5%) had a family member as a companion, and almost all (97.8%) were literate. Therefore, we feel that if the patient is counseled properly about the possible side effects of the medications and about the need for long-term treatment, which is due to the chronic and relapsing nature of the disease, the chance of non-adherence may be minimized to a great extent. A recent study on adherence rates in five chronic skin diseases, including acne, showed that unresponsiveness was the most common reason for treatment discontinuation, with the highest significance in patients with severe acne. Forgetfulness, fear of side effects, and a longer duration of treatment were other common factors [18]. This also supports our suggestion that these factors may be minimized to a great extent with adequate counseling by the doctor prescribing the treatment. However, among the five dermatological diseases (acne vulgaris, psoriasis, atopic dermatitis, hair growth disorders), patients with acne vulgaris were more adherent to treatment and more motivated, probably due to the appearance of lesions in exposed areas [18]. Other factors linked to non-adherence, according to another study, included treatment dissatisfaction, the use of an over-the-counter topical medication or previous systemic therapy, lack of improvement in symptoms, lack of knowledge on the treatment, being male, poor education, living alone or being single, unemployment, insufficient time resources, feelings of frustration, and other comorbidities [19]. A pilot randomized controlled trial found that, even after demonstrating the product and sampling the fixed combination of adapalene or benzoyl peroxide gel, adherence rates decreased from 86% after one week of treatment to 36% within six weeks of treatment [20].
Good adherence correlated with patients who had a better understanding of acne and its treatment. The best adherers used cosmetics, experienced good clinical improvement, had more severe acne, used either isotretinoin or topical therapy alone, and were both knowledgeable about and satisfied with their treatment. An increase in acne disability and a decrease in the duration of treatment or alcohol intake showed a direct correlation with high compliance. Adherence with topical therapy was positively associated with the negative impact of acne on quality of life [21].
It may be assumed that non-adherence rates are higher than recorded, jeopardizing the reported treatment efficacy rates. This implies that much larger sample sizes are required in trials to achieve statistical significance [22].
Simplification serves as one solution to non-adherence, allowing treatment to better fit into the patient’s lifestyle. Among patients who were prescribed one, two, or three acne treatments, primary adherence was significantly higher in those who were prescribed one medication [7]. Education, specifically dynamic education, which involves more informative patient–physician interaction, may also increase adherence. Patients with acne who had greater adherence expressed a positive effect of their education and interaction with the dermatologist on their behavior, while those dissatisfied with their interaction with the dermatologist reported feeling unsure as to why they needed continuous treatment, what the expected results were, or how to prevent acne in general [14]. Scheduling follow-up visits is an effective method of intervention to increase adherence [23].
CONCLUSION
In this study, the hospital prevalence of non-adherence to acne treatment was found to be 62.16%. Greater non-compliance was observed in patients taking both oral and topical medications. Among the different reasons for non-compliance, failing to remember to take the medications at the right time was the most prevalent answer, followed by being unaware of the necessity of their continuation, the appearance of their side effects, no improvement with the medications taken, an inability to dedicate enough time for a follow-up, and others. It seems, thus, that we may be able to minimize non-adherence to acne treatment to a great extent with adequate counseling.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Canavan TN, Chen E, Elewski BE. Optimizing non-antibiotic treatments for patients with acne:A review. Dermatol Ther (Heidelb). 2016;6:555-78.
2. Hay RJ, Johns NE, Williams HC, Bolliger IW, Dellavalle RP, Margolis DJ, et al. The global burden of skin disease in 2010:An analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134:1527-34.
3. Walker SL, Shah M, Hubbard VG, Pradhan HM, Ghimire M. Skin disease is common in rural Nepal:Results of a point prevalence study. Br J Dermatol. 2008;158:334-8.
4. Poudyal Y, Ranjit A, Pathak S, Chaudhary N. Pattern of pediatric dermatoses in a tertiary care hospital of western Nepal. Dermatol Res Pract. 2016;2016:6306404.
5. Fox L, Csongradi C, Aucamp M, Du Plessis J, Gerber M. Treatment modalities for acne. Molecules. 2016;21:1-20.
6. Akdogan N, Dogan S, Atakan N, Yalçin B. Association of serum hormone levels with acne vulgaris:Low estradiol level can be a pathogenetic factor in female acne. Our Dermatology Online. 2018;9:249-56.
7. Anderson KL, Dothard EH, Huang KE, Feldman SR. Frequency of primary nonadherence to acne treatment. JAMA Dermatology. 2015;151:623-6.
8. Pawin H, Beylot C, Chivot M, Faure M, Poli F, Revuz J, et al. Creation of a tool to assess adherence to treatments for acne. Dermatology. 2009;218:26-32.
9. Adityan B, Kumari R, Thappa D. Scoring systems in acne vulgaris. Indian J Dermatol Venereol Leprol. 2009;75:323-6.
10. Moradi Tuchayi S, Alexander TM, Nadkarni A, Feldman SR. Interventions to increase adherence to acne treatment. Patient Prefer Adherence. 2016;10:2091-6.
11. Hayran Y, ?ncel Uysal P, Öktem A, Aksoy GG, Akdo?an N, Yalç?n B. Factors affecting adherence and patient satisfaction with treatment:A cross-sectional study of 500 patients with acne vulgaris. J Dermatolog Treat. 2019;6634(May):1-6.
12. Yentzer BA, Gosnell AL, Clark AR, Pearce DJ, Balkrishnan R, Camacho FT, et al. A randomized controlled pilot study of strategies to increase adherence in teenagers with acne vulgaris. J Am Acad Dermatol. 2011;64:793-5.
13. Dréno B. Recent data on epidemiology of acne. Ann Dermatol Venereol. 2010;137 Suppl 2:S49-51.
14. Miyachi Y, Hayashi N, Furukawa F, Akamatsu H, Matsunaga K, Watanabe S, et al. Acne management in Japan:Study of patient adherence. Dermatology. 2011;223:174-81.
15. Park C, Kim G, Patel I, Chang J, Tan X. Improving adherence to acne treatment:The emerging role of application software. Clin Cosmet Investig Dermatol. 2014;7:65-72.
16. Tan X, Al-Dabagh A, Davis SA, Lin HC, Balkrishnan R, Chang J, et al. Medication adherence, healthcare costs and utilization associated with acne drugs in Medicaid enrollees with acne vulgaris. Am J Clin Dermatol. 2013;14:243-51.
17. Sevimli Dikicier B. Topical treatment of acne vulgaris:Efficiency, side effects, and adherence rate. J Int Med Res. 2019;47:2987-92.
18. Alsubeeh NA, Alsharafi AA, Ahamed SS, Alajlan A. Treatment adherence among patients with five dermatological diseases and four treatment types:A cross-sectional study. Patient Prefer Adherence. 2019;13:2029-38.
19. Kaymak Y, Taner E, Taner Y. Comparison of depression, anxiety and life quality in acne vulgaris patients who were treated with either isotretinoin or topical agents. Int J Dermatol. 2009;48:41-6.
20. Sandoval LF, Semble A, Gustafson CJ, Huang KE, Levender MM, Feldman SR. Pilot randomized-control trial to assess the effect product sampling has on adherence using adapalene/benzoyl peroxide gel in acne patients. J Drugs Dermatol. 2014;13:135-40.
21. Snyder S, Crandell I, Davis SA, Feldman SR. Medical adherence to acne therapy:A systematic review. Am J Clin Dermatol. 2014;15:87-94.
22. Eicher L, Knop M, Aszodi N, Senner S, French LE, Wollenberg A. A systematic review of factors influencing treatment adherence in chronic inflammatory skin disease – strategies for optimizing treatment outcome. J Eur Acad Dermatol Venereol. 2019;33:2253-63.
23. Yentzer BA, Ade RA, Fountain JM, Clark AR, Taylor SL, Fleischer AB Jr FS. Simplifying regimens promotes greater adherence and outcomes with topical acne medications:A randomized controlled trial. Cutis. 2010;86:103-8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-3542-0350 http://orcid.org/0000-0002-3542-0350 |





Comments are closed.