The first case of adalimumab-induced hypertrophic lichen planus
Sarra Saad 1, Mouna Korbi1, Ismail Bejia2, Hichem Belhadjali1, Jameleddine Zili1
1, Mouna Korbi1, Ismail Bejia2, Hichem Belhadjali1, Jameleddine Zili1
1Dermatology Department, University Hospital of Monastir, University of Medicine of Monastir, University of Monastir, Tunisia, 2Rheumatology Department, University Hospital of Monastir, University of Medicine of Monastir, University of Monastir, Tunisia
Corresponding author: Sarra Saad, MD
How to cite this article: Saad S, Korbi M, Bejia I, Belhadjali H, Zili J. The first case of adalimumab-induced hypertrophic lichen planus. Our Dermatol Online. 2021;12(3):341-342.
Submission: 05.09.2020; Acceptance: 06.11.2020
DOI: 10.7241/ourd.20213.30
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Tumor necrosis factor (TNF) alpha inhibitors are new therapeutics used to treat a range of rheumatological diseases refractory to conventional drugs. Several anti-TNF-a side effects have been described, especially cutaneous manifestations [1]. A number of so-called lichenoid eruptions have been reported in three different clinical patterns: lichen planus-like (LP-like), non-specific maculopapular eruption, and psoriasis-like. These cases are unified by a common lichenoid histology [2]. However, hypertrophic LP has never been reported in association with anti-TNF-a therapy.
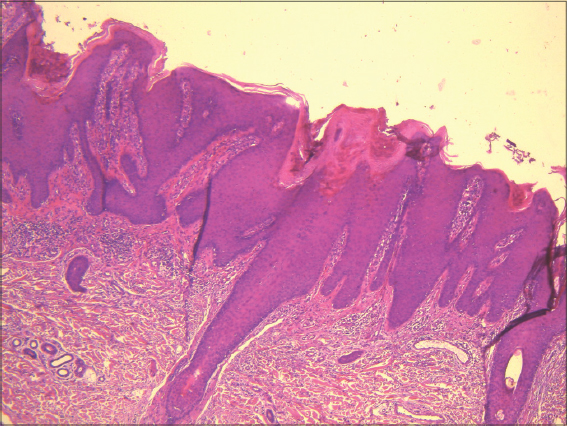
A healthy 68-year-old male had suffered from arthropathic psoriasis for twenty-six years. His medical history involved multiple cutaneous psoriatic lesions almost on the entire body (body surface affected (BSA) = 60%), which had been resistant to topical treatment. The patient was treated with methotrexate. Three years later, we noted a slight improvement in both cutaneous (BSA = 40%) and arthropathic symptoms. We opted for one injection of adalimumab weekly. We noted rapid clinical improvement (BSA = 2%) and relieving of arthropathic symptoms. However, several months later, the patient presented himself with purplish nodular lesions on both forearms (Fig. 1). We noted neither mucosal involvement nor hair or nail lesions. A histopathological examination confirmed the diagnosis of hypertrophic LP (Fig. 2). Based on the clinical history and the histopathological findings, the diagnosis of adalimumab-induced hypertrophic LP was established. Adalimumab could not be stopped. The hypertrophic LP was treated with a topical corticosteroid with a slight improvement.
TNF is a pro-inflammatory cytokine produced by a wide variety of cell types, including keratinocytes, that plays a complex role in innate immunity and host defense, particularly against mycobacterial infections, and that may both enhance and suppress adaptive immunity. The main anti-TNF-a drugs (adalimumab, etanercept, and infliximab) have all been shown to be very effective in treating psoriasis [3].
Our patient presented an unusual side effect of adalimumab. A temporal association and a histopathological examination of our patient strongly suggested a causative relationship between the TNF blockage and the onset of the cutaneous lesions. With the Naranjo algorithm, a causality score of 6 was obtained and the case was categorized as a probable reaction to adalimumab.
Lichenoid eruptions induced by TNF-a inhibitors have, for the first time, been described by Vergara et al. in 2002 [4]. Since then, multiple cases of lichenoid eruption, including cutaneous and oral LP, lichen planopilaris, maculopapular eruption, and psoriasis-like LP, have been reported [1,2,4,7]. Only twenty cases of LP induced by TNF-a inhibitors have been described [1,2,4]. The three main TNF-a inhibitors (infliximab, etanercept, and adalimumab) were incriminated [5]. Some mechanisms have been suggested to explain the occurrence of lichenoid eruption due to TNF-a inhibitors therapy. In fact, the suppression of TNF may lead to the development of opposing inflammatory cytokines, which may activate T cells and dendritic cells leading to lichenoid eruption [6].
Our patient presented hypertrophic LP, which is a particular clinical and histological form of LP. To the best of our knowledge, no case of hypertrophic LP induced by an anti-TNF-a drug has been reported [1,2,4]. Only one case of hypertrophic LP induced by anti-interleukin 17 (secukinumab) has been reported [7].
In conclusion, we witnessed the first case of hypertrophic LP induced by an anti-TNF-a drug. Physicians should be aware of this rare side effect. In fact, patients with cutaneous hypertrophic LP are prone to skin cancer. Therefore, we believe it to be worthwhile to monitor patients who use anti-TNF-a drugs for psoriasis against hypertrophic LP.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Andrade P, Lopes S, Albuquerque A, Osório F, Pardal J, Macedo G. Oral lichen planus in IBD patients:A paradoxical adverse effect of anti-TNF-a therapy. Dig Dis Sci. 2015;60:2746-9.
2. Jayasekera PSA, Walsh ML, Hurrell D, Parslew RAG. Case report of lichen planopilaris occurring in a pediatric patient receiving a tumor necrosis factor a inhibitor and a review of the literature. Pediatr Dermatol. 2016;33:e143-6.
3. Tateishi C, Imanishi H, Nimmannitya K, Tsuruta D. Ustekinumab successfully treated a patient with severe psoriasis vulgaris with primary failure to infliximab and secondary failure to adalimumab. Our Dermatol Online. 2015;6:296-8.
4. Vergara G, Silvestre JF, Betlloch I, Vela P, Albares MP, Pascual JC. Cutaneous drug eruption to infliximab:Report of 4 cases with an interface dermatitis pattern. Arch Dermatol. 2002;138:1258-9.
5. Abreu Velez AM, Jackson BL, Howard MS. Intraepidermal and subepidermal blistering with skin necrosis, possibly caused by etanercept in treatment of a patient with psoriasis. Our Dermatol Online. 2015;6:299-303.
6. Upasana M, Yin WY, Bo WJ, Quan SJ. Granulocyte-colony stimulating factor induced early psoriasis – a case report and literature review. Our Dermatol Online. 2020;11:56-8.
7. Doolan BJ, Anderton H, Christie M, Dolianitis C. Cutaneous lichen planus induced by secukinumab. J Clin Exp Dermatol Res. 2017;9:437.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.