Impact of prurigo nodularis on quality of life and psychiatric comorbidities among children and their parents in Yaoundé, Cameroon
Emmanuel Armand Kouotou, Ulrich Nguena Feungue, Dahlia Noëlle Tounouga , Ange Engolo Fandio, Elie Claude Ndjitoyap Ndam
, Ange Engolo Fandio, Elie Claude Ndjitoyap Ndam
1Department of Internal Medicine and Specialties, Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Yaoundé, Cameroon, 2Yaoundé University Teaching Hospital, Yaoundé, Cameroon, 3University Hospital of Treichville, Abidjan, Ivory Coast, 4Lafe-Baleng Divisional Health Centre, Bafoussam, Cameroon
Corresponding author: Dahlia Noelle Tounouga, MD
How to cite this article: Kouotou EA, Nguena Feungue U, Tounouga DN, Engolo Fandio A, Ndjitoyap Ndam EC. Impact of prurigo nodularis on quality of life and psychiatric comorbidities among children and their parents in Yaoundé, Cameroon. Our Dermatol Online. 2021;(3):244-250.
Submission: 16.03.2021; Acceptance: 31.05.2021
DOI: 10.7241/ourd.20213.3
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Prurigo nodularis (PN) is a recurrent, itchy dermatosis in children secondary to arthropods bites. The objective of this study was to determine the impact of PN on the quality of life (QoL) of affected children and their parents and to investigate the presence of depression and anxiety.
Method: We performed a cross-sectional study during the period from February through May 2017 at the dermatology departments of six hospitals in Yaoundé, Cameroon. Children suffering from PN and their parents were included. We collected sociodemographic data, assessed the QoL of the children and their parents (CDLQI, DLQI, FDLQI), and evaluated anxiety and depression among them (GAD-7 and PHQ-9).
Results: A total of 112 children (median: 2 years; range: 5 months – 16 years), including 62 males and 50 females and their 112 parents (median age: 31 years; range: 20 – 65 years), were included in the study. As far as QoL was concerned, 29 children and 112 parents were selected. Most children (93.1%) and a large majority of the parents (99.1%) experienced negative impact on their QoL. We found no depression or anxiety among these two groups.
Conclusion: Prurigo nodularis has a negative impact on QoL among affected children and their parents. However, we found no psychiatric comorbidities associated with this pathology in our study.
Key words: Prurigo nodularis; Quality of life; Parents; Children; Cameroon
INTRODUCTION
Prurigo nodularis (PN) is a recurrent, itchy dermatosis in children secondary to arthropods bites [1]. It is due to cellular hypersensitivity to environmental arthropods and is characterized by pruritus and papular or papulovesicular erythematous skin lesions on the exposed areas: the upper and lower limbs, the neck area, and the trunk [1,2]. Because PN is often chronic and recurrent despite adequate management [2], it may alter the psychological and social well-being of patients and have an impact on their quality of life (QoL) [3]. PN is a childhood condition and its management requires parents to accompany their children during consultation and to care for them; this may be a source of psychological stress for these parents [4]. To the best of our knowledge, the literature offers no data on PN, particularly the impact of PN on QoL among children in Cameroon. This is the reason why we decided to conduct this study, which aimed to assess the QoL of patients with PN and their parents and to investigate the existence or absence of psychiatric comorbidities.
MATERIALS AND METHODS
Method
This was a descriptive, cross-sectional study that took place for a period of four months, from February through May 2017, in six hospitals of Yaoundé, namely, Yaoundé Central Hospital (YCH), Biyem-Assi District Hospital (BADH), Gyneco-Obstetric and Pediatric Hospital of Yaoundé (GOPHY), University Teaching Hospital of Yaoundé (UTHY), Essos Hospital Center (EHC), and Subdivisional health Center of Elig-Essono. These hospitals were chosen by convenience, based on the availability of a dermatologist. Our sampling was non-probabilistic and consecutive. Our target population was children attending dermatological consultation for dermatosis during this period.
In the study, we included: 1) children aged 0 to 16 years attending dermatological consultation because of PN after clinical examination, whose parents gave their consent, and 2) parents or guardians of children suffering from PN, who gave their consent to participate in the study.
Furthermore, all children and parents who refused to participate or who decided to withdraw were excluded from the study without any constraint.
Ethical Approval
We requested and obtained the research authorizations from the administrative authorities of the hospitals included in this study.
Data Collection
Data collection took place during dermatological consultations. Thus, after informing patients about the study and obtaining their informed consent, patients fulfilling the inclusion criteria were retained after the consultation. A questionnaire containing sociodemographic data, the effect of PN on the QoL of patients and research on psychiatric comorbidities, was completed by all patients according to the periods adapted to each scale: one week for the CDLQI, two weeks for the PHQ9 and GAD7, and one month for the FDLQI.
MATERIAL
Data Collection Tools
The data was collected using:
• A technical sheet providing information on sociodemographic data (age, sex, place of residence, type of residence, profession of parents/guardians);
• Assessment scales of QoL in children and parents/guardians: 1) The Children’s Dermatology Life Quality Index (CDLQI) assessed QoL in children aged 4 to 16 years [5]. Patients responded to questions about their illness over the last week prior to inclusion; this included 10 questions divided into six items: symptoms (question 1 and 2), sleep (question 9), social life and leisure (questions 4, 5, and 6), study (question 7), relationships (questions 3 and 8), and treatment (question 10). Each question was scored from 0 to 3, giving a possible score range from 0 (no impact of the skin disease on QoL) to 30 (maximum impact on QoL); 2) The Family Dermatology Life Quality Index (FDLQI) [6] assessed the QoL of parents/guardians of these children. Parents or guardians responded to questions about the impact that their child’s illness had had on them over the last four weeks prior to inclusion; this consisted of ten items: emotional distress, physical well-being, personal relationships, reactions with others, social life, hobbies/leisure, time, extra housework, job/study, and household expenditure. Each of these items was scored from 0 to 3. The total score varied from 0 to 30 points and was calculated by adding the score obtained from each of the different questions;
• Anxiety and depression screening scales: 1) The 9-Item Patient Health Questionnaire (PHQ-9) is a nine-point, self-assessment scale employed to diagnose mental depression according to nine criteria for major depression in the Diagnostic and Statistical Manual of Mental Disorders, Version 4 (DSM-IV) [7]; each item was scored from 0 to 3; 2) Generalized Anxiety Disorder 7-Item (GAD-7) is a 7-item anxiety rating scale, a useful screening tool for diagnosing generalized anxiety disorder [8]; each item was scored from 0 to 3. The total score varied from 0 to 21. This was used to screen the presence of mental depression and anxiety in children aged ≥ eight years as well as in their parents.
Interpretation of QoL Scores
The CDLQI made it possible to assess the children’s QoL and the parents’ FDLQI. Responses to these two scales were interpreted as follows: 1) extremely (3 points); 2) a lot (2 points); 3) a little (1 point); and 4) not at all (0 points). The total score was calculated by adding the scores obtained from each question. The interpretation of the scores was as follows: 1) 0–1: no effect at all on the patient’s life; 2) 2–6: small effect on the patient’s life; 3) 7–12: moderate effect on the patient’s life; 4) 13–18: large effect on the patient’s life; and 5) 19–30: extremely large effect on the patient’s life.
Interpretation of Depression and Anxiety Scores
The PHQ-9 and GAD-7 questionnaires were used to screen the presence of mental depression and anxiety, respectively, in children aged ≥ eight years. The same questionnaire was taken by their parents. Responses to each item in these two scales were rated as follows: 1) nearly every day (3 points); 2) – more than half the days (2 points); 3) several days (1 point); and 4) not at all (0 points).
The total score was calculated by adding the score obtained from each question, thus varying from 0 to 27 in the PHQ-9 and from 0 to 21 in the GAD-7. A PHQ-9 score of ≥10 had a sensitivity and specificity of 88% for depression [7], while a GAD-7 score of ≥10 had a sensitivity of 89% and a specificity of 82% for anxiety [8]. Therefore, the results were interpreted as follows: 1) a score of ≤10: no depression or anxiety; and 2) a score of ≥10: depression or anxiety.
Correlation Study
We looked for the existence of a correlation between the age and the QoL score, between the age and the anxiety and mental depression scores, and between the duration of PN and the QoL score, respectively in children and adults. We also looked for a correlation between the child’s age and the parents’ QoL and anxiety and depression scores.
Statistical Analysis
The data collected was encoded by the CSPRO 6.3 software, then exported to SPSS 23.0 for statistical analysis. Qualitative variables were described by their numbers and percentages and quantitative variables by their means associated with their standard deviation. The Mann–Whitney test was employed to compare medians. Pearson and Spearman linear correlation tests were used to determine the correlation between the patient’s age and the QoL scores and the depression and anxiety scores on one hand and between the child’s age and the child’s scores, the parents’ QoL and the depression and anxiety scores on the other hand. The threshold of significance was set at 5%.
Ethics Statement
Before beginning the study, ethical clearance was obtained from the institutional ethics committee of the Faculty of Medicine and Biomedical Sciences of Yaoundé and authorizations from the directors of hospitals included in the study were obtained. The patients were informed about the different aspects of the study and their agreement was only obtained after the parents gave their consent to participate in the study and obtaining an agreement for children aged >7 years. We ensured the anonymity of the patients and the confidentiality of the information collected.
RESULTS
Sociodemographic Characteristics of Children
We included a total of 112 predominantly male children (62/112; 55.4%), with a sex ratio of 1.2. The most represented age group was 0 to 5 years (78.6%). The median age was 2 (18 months – 4 years), varying from 5 months to 16 years. In these children, the median duration of PN was 8 (2–18) months, varying from 1 to 108 months.
Sociodemographic Characteristics of Parents
Our study included 112 predominantly female parents (109/112; 97.3%). The mean age among the parents was 33 ± 8.2 years, varying from 20 to 65 years. Among these parents, 56.2% were married and most of them had high school education (50.9%).
QoL Assessment and Screening for Mental Depression and Anxiety in Children
Children’s QoL Assessment (CDLQI)
In our sample, 29/112 children were aged from 4 to 16 years old and we assessed their QoL over the last week prior to inclusion with the CDLQI. Table 1 shows the distribution of these children according to responses to the CDLQI’s questions.
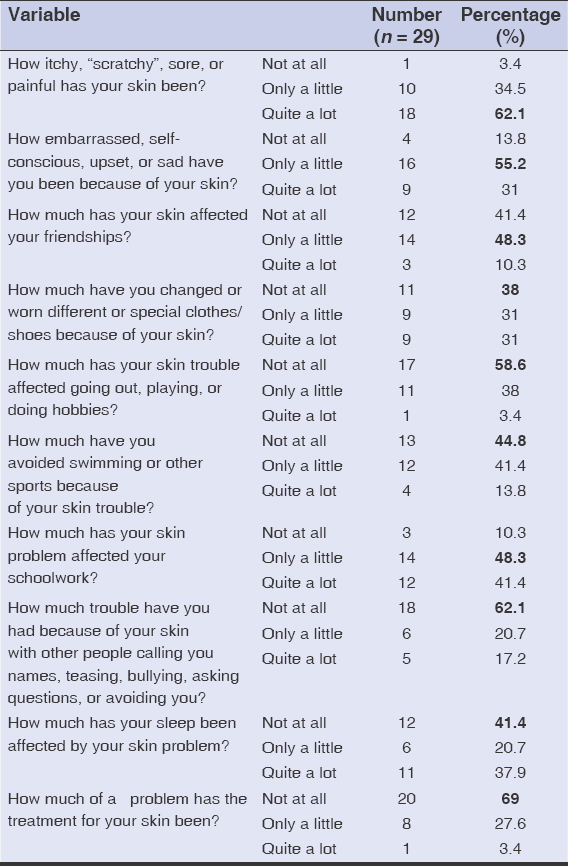 |
Table 1: Distribution of the children according to the CDLQI. |
The most affected QoL items were symptoms and study (Table 1). As far as the symptoms items are concerned, the questions relating to the sensation of itching and/or soreness (28/29; 96.6%) and discomfort related to the skin problem (25/29; 86.2%) were mostly involved (Table 1). As for the study item, only 3 children (10.3%) felt no impact of their condition on their schoolwork (Table 1).
The mean QoL score in the 29 affected children was 8.6 ± 2.8, ranging from 0 to 15. QoL was impaired in almost all children (27/29; 93.1%). It was slightly, moderately, and severely altered in 5/29 (17.2%), 17/29 (58.6%), and 5/29 (17.2%), respectively (Table 2).
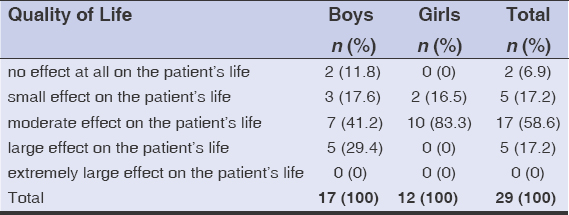 |
Table 2: Distribution of the children according to the level of deterioration in quality of life (CDLQI) |
We found moderate QoL impairment in 7 boys (41.2%) and 10 girls (83.3%). The median QoL score in boys was 9, with extremes of 0 and 15, while in girls it was 10, with extremes of 4 and 12. Furthermore, this difference was not statistically significant (p = 0.91).
Comparison of QoL between Boys and Girls by CDLQI
There was no statistically significant difference between the median score of different QoL items (symptoms, activities, leisure, personal relationships, study, and treatment) between boys and girls (p > 0.05) (Table 3).
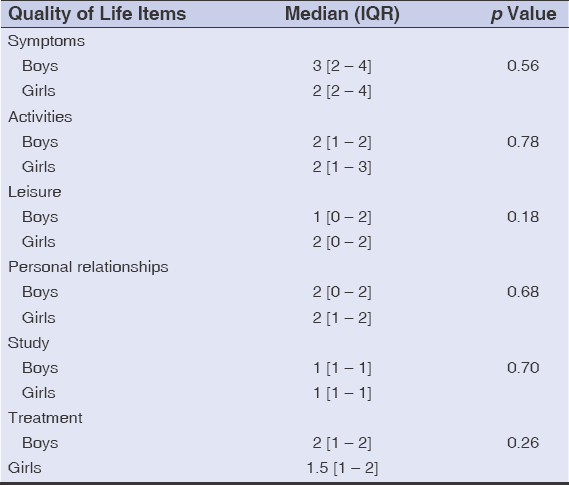 |
Table 3: Comparison of the QoL score by the CDLQI according to the sex of child |
Assessment of Anxiety and Depression in Children
Among our 112 children, 19 were ≥8 years old; we administered the PHQ-9 and GAD-7 questionnaires to them. After rating each question from the PHQ-9 and GAD-7, we obtained scores that ranged from 0 to 4 and from 0 to 6, respectively. We found no cases of mental depression or anxiety in our sample.
Assessment of QoL and Searching for Anxiety and Depression in Parents
We assessed the QoL of the 112 parents accompanying our children. Table 4 shows the distribution of the parents according to responses to the FDLQI over the last four weeks preceding their inclusion in the study. Emotional distress and expenditure were the most intruding factor for the parents (Table 4).
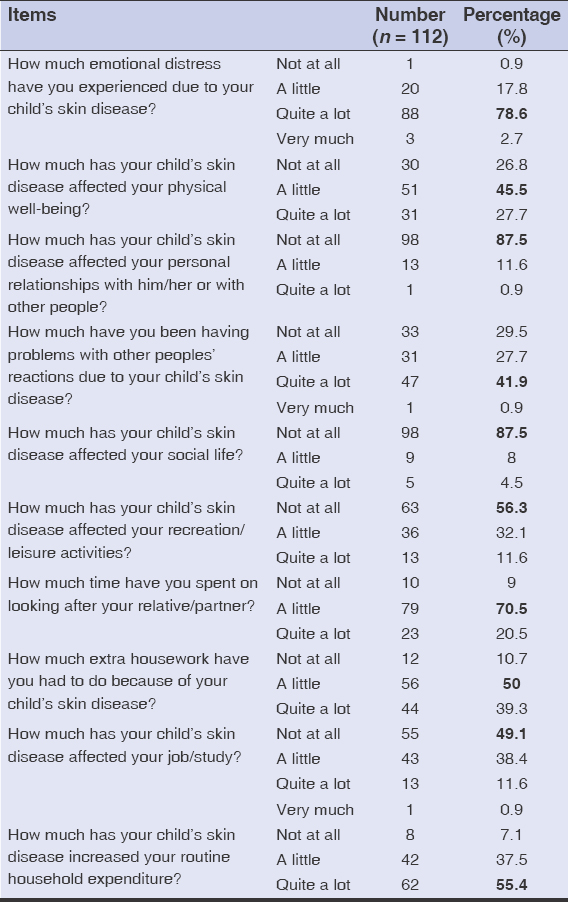 |
Table 4: Distribution of the parents according to responses to the FDLQI. |
We found a moderate change in QoL in more than half of the parents (76/112; 67.9%). Furthermore, this alteration in QoL was mild in 20/112 (17.9%) and severe in 15/112 (13.4%). Only one parent seemed to be unaffected by his child’s illness. The mean QoL score for parents was 9.4 ± 2.1, ranging from 0 to 17.
Researching Anxiety and Depression in Parents
We looked for the presence of anxiety or mental depression in the 112 parents in our sample. After rating each question from the PHQ-9 and GAD-7, we obtained scores that ranged from 0 to 8 and from 0 to 9, respectively. No cases of anxiety or mental depression were found among the parents. We found no statistically significant difference between the median score for depression and anxiety of the parents accompanying girls compared to the score of the parents accompanying boys (p > 0.05) (Table 5).
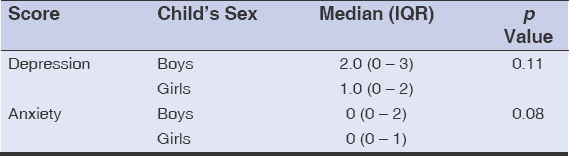 |
Table 5: Comparison of mental depression and anxiety scores of parents accompanying boys compared to those accompanying girls |
Correlation Study
Association between Age and QoL Score
We found no linear correlation between the age of a child and the child’s QoL score (r = 0.05; p = 0.79) on one hand and between the age of a parent and the parent’s QoL score (r = 0.15; p = 0.12) on the other hand.
Association between Duration of Evolution of PN and QoL Score
We found no linear correlation between the duration of evolution of PN and the QoL score in children (r = 0.15; p = 0.44) on one hand and between the duration of development of PN and the QoL score in parents (r = 0.04; p = 0.65) on the other hand.
Association between age and mental depression and anxiety score
We found no linear correlation between the age of a child and the score for mental depression (r = 0.25; p = 0.29) or anxiety (r = 0.22; p = 0.35). In contrast, among parents, there was a weak positive linear correlation between the age and mental depression (r = 0.22; p = 0.02). In fact, this score increased with the age of the parent (Figure 1).
 |
Figure 1: Linear correlation of the depression score among parents and their ages. |
Association between Child’s Age and QoL Score and Parental Anxiety and Depression Score
There was a weak negative linear correlation between the child’s age and the parent’s QoL (r = -0.31; p = 0.001). Indeed, the younger the child, the more the parent’s QoL was altered. There was also a weak positive linear correlation between the child’s age and parental anxiety (r = 0.25; p = 0.007). In fact, the parent’s anxiety score increased with the child’s age. There was a weak positive linear correlation between the child’s age and parental mental depression (r = 0.21; p = 0.03); the parent’s mental depression score increased with the child’s age (Table 6).
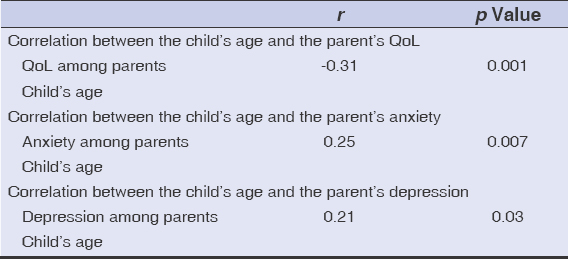 |
Table 6: Correlation studies. |
DISCUSSION
To our knowledge, this work is one of the few African studies assessing QoL and psychiatric comorbidities in children with PN as well as in their parents.
Overall, QoL was impaired in 93.1% of children and 99.1% of parents. In our series, there was a weak negative linear correlation between the child’s age and the parent’s QoL (r = -0.31; p = 0.001). In children and parents, we found no psychiatric comorbidities.
Quality of Life in Children and Parents
The mean QoL score in children was 8.6 ± 2.8; overall, the child’s QoL was moderately impaired. This mean score was close to that of Monti et al. from Italy (7.0 ± 5.2), who also found a moderate alteration in QoL in a cohort of children suffering from atopic dermatitis [4]. In contrast, Maridet et al. from France found an average CDLQI score of 6.1, which means an overall slight deterioration in QoL in children suffering from chronic prurigo [9]. The higher level of QoL alteration during PN compared to chronic prurigo might be explained by the periodic occurrence of more inflammatory acute flare-ups during PN compared to chronic prurigo. Chronic prurigo is also said to be somewhat accepted in children. Items of QoL that posed the biggest problem in children were symptoms, with a negative impact of pruritus and/or discomfort in almost all children (28/29; 86.2%), and study (26/29; 89.7%). In 2009, Kouassi et al. from Ivory Coast also noted a highly significant effect of pruritus on QoL among children with atopic dermatitis in their series (65%) [10]. The itchy, displaying, and recurrent nature of these dermatoses would explain these children’s feelings. Over half of our children had trouble with sleeping (58.6%) and felt sadness (96.2%) because of their skin problem. Several series in the literature corroborate our results [10]. Prurigo and itchy dermatoses generally affect QoL in both adults and children. Brenaut et al., reported in their multicenter cohort in Europe, an alteration in QoL ranging from very significant to extreme in 63.0% of adult patients with PN [11]. The Ivorian study on the QoL of children with atopic dermatitis also found a similar profile; indeed, the impact of the condition on QoL ranged from no effect to very strong effect [10]. Among our participants, only 2 (6.9%) children had no altered QoL. Overall, itchy dermatoses affect patients’ QoL, are a source of expense for families, and may even lead to psychiatric comorbidities, such as depression, anxiety, and suicidal ideation [11,12].
Among the parents, the mean QoL score was 9.4 ± 2.1, with a moderate impact of their child’s affection on their QoL. This QoL score was higher than that of the children (8.6 ± 2.8), which reflects a greater alteration in QoL in the parents than in the sick child. This finding might be explained by the importance of the cost of long-term care; most parents admit that their child’s illness leads to increased expenses (21/29; 72%). Overall, the QoL of the parents is at least as impaired as that of the sick child.
In addition, parental QoL is negatively correlated with the child’s age (r = -0.31; p = 0.001). Although this correlation is weak, the QoL of parents is mostly altered when the child is much younger. Our work is corroborated by one of Monti et al., who found a weak inverse correlation between the age of the child with atopic dermatitis and the parent’s QoL (r = -0.26; p = 0.046) [4]. Parents seem more worried about their children’s illness when they are young.
Anxiety and Mental Depression
We found no cases of anxiety (GAD-7) or mental depression (PHQ-9) in either children or parents in our sample. All scores were below 10. This result suggests that, in our context, although unaesthetic, PN does not affect the child’s QoL to the point of causing mental depression and anxiety in both the child and the parent. However, the tendency seems different when prurigo affects adults. Indeed, Brenault et al., in their cohort of 27 patients with prurigo, found a proportion of 30.4% of cases of mental depression, 39.1% of anxiety, and 21.8% of suicidal ideation [11].
Correlation Study
We found a weak positive correlation between the parental age and the parental mental depression score (r = 0.22; p = 0.02). The older the parents are, the higher this score. Indeed, parents become less and less inclined to endure stress from their child’s illness with age. We also found a weak positive linear correlation between the child’s age and the parent’s anxiety score (r = 0.25; p = 0.007) on one hand and a weak positive linear correlation between the child’s age and the parent’s mental depression score on the other hand (r = 0.21; p = 0.03). Conversely, there was a weak negative linear correlation between the age of the child and the QoL of the parents (r = -0.31; p = 0.001) in our series; the parent’s QoL was mostly altered if the child was younger. In 2011, Monti et al. found similar results in their cohort. Their work revealed that QoL among the parents of children with atopic dermatitis was also negatively correlated with the age of the children (r = -0.26; p = 0.046) [4]. Concerning itchy skin diseases in children, parents are more affected by the condition of their child if the child is younger.
Limitations of our Study
Our study might have had some limitations due to the fact that: 1) Our study population was a hospital-based study and, therefore, was not representative of the general population. 2) We made a choice of convenience for the different hospitals in which patient recruitment took place. 3) All the QoL scales that we employed had been tested on Caucasian populations. Research should be done to find better ways to measure mental depression and anxiety in young children—less than four years old—and in Africans in general.
CONCLUSION
The QoL of children with PN and of their parents is mostly moderately impaired. Parental QoL impairment is inversely correlated with the child’s age. However, PN, although with an impact on the QoL of children and their parents in our environment, is not associated with psychiatric comorbidities, including mental depression and anxiety. The clinician should consider the QoL aspect of the sick child and parent in order to improve their overall management.
ACKNOWLEDGMENTS
The authors are very grateful to the directors of the six hospitals in Yaoundé where our study took place and to all of their staff for their kind assistance during data collection. This recognition also goes to the patients and the parents/guardians of the children who agreed to participate fully and voluntarily in this study.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Philibert F, Baubion E, Amazan E, Ferrati-Fidelin G. Recrudescence de prurigo strophulus en Martinique liée aux piqûres de culicoïdes. Ann Dermatol Vénéréol. 2019;146:A244-5.
2. Halpert E, Borrero E, Ibañez-Pinilla M, Chaparro P, Molina J, Torres M, et al. Prevalence of papular urticaria caused by flea bites and associated factors in children 1-6 years of age in Bogotá, D.C. World Allergy Organ J. 2017;10:36.
3. Henshaw EB, Olasode OA, Ogedegbe EE, Etuk I. Dermatologic conditions in teenage adolescents in Nigeria. Adolesc Health Med Ther. 2014;5:79-87.
4. Monti F, Agostini F, Gobbi F, Neri E, Schianchi S, Arcangeli F. Quality of life measures in Italian children with atopic dermatitis and their families. Ital J Pediatr. 2011;37:59.
5. Olsen JR, Gallacher J, Finlay AY, Piguet V, Francis NA. Quality of life impact of childhood skin conditions measured using the Children’s Dermatology Life Quality Index (CDLQI):A meta-analysis. Br J Dermatol. 2016;174:853-61.
6. Handjani F, Kalafi A. Impact of dermatological diseases on family members of the patients using Family Dermatology Life Quality Index:A preliminary study in Iran. Iran J Dermatol 2013;16:128-31.
7. Manea L, Gilbody S, McMillan D. A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ9) algorithm scoring method as a screen for depression. Gen Hosp Psychiatry. 2015;37:67-75.
8. Wild B, Eckl A, Herzog W, Niehoff D, Lechner S, Maatouk I, et al. Assessing generalized anxiety disorder in elderly people using the GAD-7 and GAD-2 scales:Results of a validation study. Am J Geriatr Psychiatry. 2014;22:1029-38.
9. Maridet C, Perromat M, Miquel J, Chiaverini C, Bessis D, Lasek A, et al. Prurigo chronique de l’enfant:formes cliniques et profils de sensibilisation aux allergènes de l’environnement. Étude prospective. Ann Dermatol Vénéréol. 2016;143:S140.
10. Kouassi YI, Ahogo KC, Bih OF, Kouassi KA, Kourouma HS, Allou AS, et al. Évaluation de la qualitéde vie des enfants atteints de dermatite atopique par le score CDLQI en milieu tropical africain. Ann Dermatol Vénéréol. 2019;146:A187.
11. Brenaut E, Misery L, Kupfer J, Dalgard F, Halvorsen JA. Impact sur la qualitéde vie et comorbidités psychiatriques chez les patients avec un prurigo nodulaire en Europe. Ann Dermatol Vénéréol. 2016;143:S266.
12. O’Donnell BF. Urticaria:Impact on Quality of Life and Economic Cost. Immunol Allergy Clin North Am. 2014;34:89-104.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-3879-2659 http://orcid.org/0000-0003-3879-2659 |



Comments are closed.