Lipedematous scalp: A possible association with Ehlers–Danlos syndrome
Najla Daadaa 1, Azima Ben Tanfous1, Imen Hlel2, Anissa Zaouak1, Raja Jouini2, Ashraf Debbiche2, Houda Hammami1, Samy Fenniche1
1, Azima Ben Tanfous1, Imen Hlel2, Anissa Zaouak1, Raja Jouini2, Ashraf Debbiche2, Houda Hammami1, Samy Fenniche1
1Department of Dermatology, Hbib Thameur Hospital, Tunis, Tunisia, 2Department of Pathology, Hbib Thameur Hospital, Tunis, Tunisi
Corresponding author: Najla Daadaa, MD
How to cite this article: Daadaa N, Ben Tanfous A, Hlel I, Zaouak A, Jouini R, Debbiche A, Hammami H, Fenniche S. Lipedematous scalp: A possible association with Ehlers Danlos syndrome. Our Dermatol Online. 2021;12(3):337-338.
Submission: 02.01.2021; Acceptance: 27.03.2021
DOI: 10.7241/ourd.20213.28
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
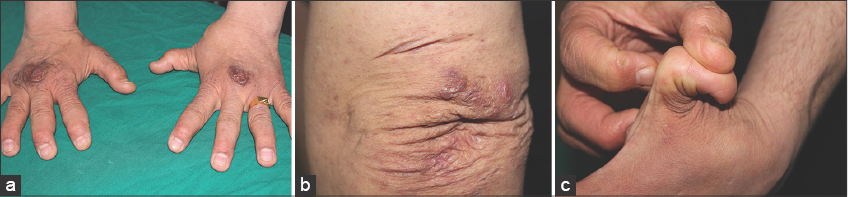
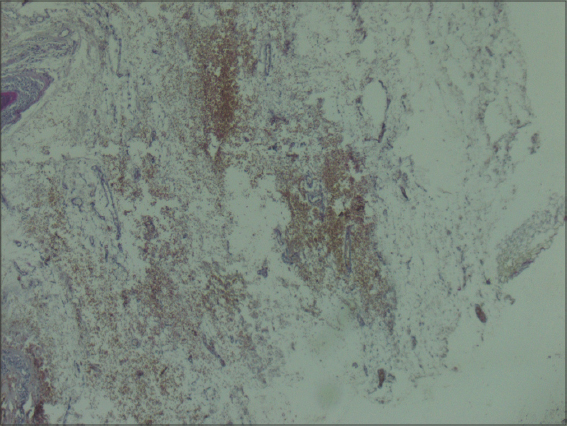
A 40-year-old male presented to the dermatology department with a history of a gradual diffuse swelling of the scalp felt as if underlaid with cotton. No previous trauma or surgery to the head or scalp were reported. He was not hyperlipidemic. The family history revealed no similar complaints in parents and siblings. The medical history included an unclassifiable form of Ehlers–Danlos syndrome (EDS) diagnosed at the age of 28 by the presence of a velvety, fragile skin, cutaneous hyperelasticity, peculiar cigarette-paper scars (Figs. 1a and 1b), subcutaneous molluscus pseudotumor formation, hypermobility of the joints (Fig. 1c), keratoconus, and mitral insufficiency. On examination, the surface of the scalp had an irregular appearance and was smooth, boggy, spongy, and fluctuant on palpation (Fig. 2). No clinical signs of inflammation were apparent. Hair density and length were normal. A histopathologic examination of a scalp skin biopsy revealed increased thickness of subcutaneous fat tissue close to the epidermis (Fig. 3) Thus, the diagnosis of a lipedematous scalp (LS) associated with EDS was reached. Therapeutic abstention happened to be the best management strategy since the patient was asymptomatic.
An LS is a rare disease characterized by a thick and boggy scalp due to increased thickness of subcutaneous fatty tissue. In 1935, Cornbleet described the first case in an African female. Up to date, about fifty cases of an LS have been reported, mostly in females [1,2]. To the best of our knowledge, only two male cases, excluding our patient, have been recorded [2,3]. Most patients with an LS are asymptomatic, as our case. The pathogenesis of an LS remains unknown. It is believed, however, that leptin, a hormone regulating fat masses and their distribution, may be inducing hyperplasia of subcutaneous fat [2]. Another theory explaining its pathogenesis involves metaplasia and displacement of adipose tissue [1,4]. EDS has not been reported in association with an LS but several women with lipedema of the lower body were reported to have a positive Beighton score (≥ 5) associated with joint pains, suggesting EDS hypermobility type (EDS-HT), formerly type III [5]. Furthermore, a single case of lipedematous alopecia, another entity that is part of the same disease spectrum associated with sparsity and shortness of the hair [3], was also described in association with significant hyperelasticity of the skin and hyperlaxity of the joints without other criteria to confirm true EDS [6]. No treatment was attempted in our case, although surgical intervention with debulking and scalp reduction have been proposed to treat an LS, but with variable results [1].
In conclusion, an LS is a rare disorder that dermatologists should be aware of, as it is not difficult to diagnose. Whether the coexistence of an LS and EDS is merely coincidental or a true association remains unclear. Further investigative studies are needed to assess a possible pathophysiological link.
ACKNOWLEDGMENTS
We would like to thank the patient for granting permission to publish this manuscript in the form of written consent.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Sahu P, Sangal B, Dayal S, Kumar S. Lipedematous scalp with varied presentations:A case series of four patients. Indian Dermatol Online J. 2019;10:571-3.
2. Al Gaadi S, Al Godayan S, Bukhari I. Lipedematous scalp:Case report and review of the literature. Our Dermatol Online. 2016;7:198-200.
3. Carrasco-Zuber JE, Alvarez-Veliz S, Cataldo-Cerda K, Gonzalez-Bombardiere S. Lipedematous scalp:A case report and review of the current literature. J Dtsch Dermatol Ges. 2016;14:418-21.
4. Fernández-Canga P, Rodríguez-Díaz E, Carvajal-Álvarez M, Gonzalvo-Rodríguez P, Vázquez-Osorio I. Lipoedematous scalp. Clin Exp Dermatol. 2019;44:684-6.
5. Herbst KL, Mirkovskaya L, Bharhagava A, Chava Y, Te CHT. Lipedema fat and signs and symptoms of illness, increase with advancing stage. Arch Med. 2015;7:1-8.
6. Kilinc E, Dogan S, Akinci H, Karaduman A. Lipedematous scalp and alopecia:Report of two cases with a brief review of literature. Indian J Dermatol. 2018;63:349-53.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-2062-2256 http://orcid.org/0000-0003-2062-2256 |




Comments are closed.