Untoward effects on the skin by the use of personal protection equipment
Amrita Anandakumar Hongal1, Sijimol Mattekudilil Vijayan1, Radhika Setharampura Ramamurthy 1, Revathi Thimmanahalli Narasimhan1, Asha Gowrappala Shanmukhappa1, Shilpa Kanathur1, Eshwari Loganathan1, Somashekar Gejje2
1, Revathi Thimmanahalli Narasimhan1, Asha Gowrappala Shanmukhappa1, Shilpa Kanathur1, Eshwari Loganathan1, Somashekar Gejje2
1Department of Dermatology, Venerology, Leprosy, Bangalore Medical College and Research Institute, Bengaluru, India, 2Department of Plastic surgery, Bangalore Medical College and Research Institute, Bengaluru, India
Corresponding author: Radhika Setharampura Ramamurthy, MBBS, MD, DNB
How to cite this article: Hongal AA, Sijimol MV, Radhika SR, Revathi TN, Shilpa K, Eshwari L, Somashekar G. Untoward effects on the skin by the use of personal protection equipment. Our Dermatol Online. 2021;12(3):238-243.
Submission: 26.11.2020; Acceptance: 14.03.2021
DOI: 10.7241/ourd.20213.2
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: COVID-19 (coronavirus disease 2019) is the global pandemic that emerged in Wuhan, China, and has rapidly spread throughout the world. Healthcare workers (HCWs) who care for patients suffering from COVID-19 are at greater risk of contracting the infection and, for this reason, PPE (personal protective equipment) is worn. As PPE covers the entire surface area of the body and is worn for long hours, HCWs are likely to suffer from untoward effects on the skin.
Methods: To determine the occurrence of untoward effects on the skin from the use of PPE among HCWs, a questionnaire was prepared and circulated online among HCWs caring for COVID-19 patients. The questionnaire included questions regarding the grade and the duration of use of PPE and untoward effects on the skin. Univariate and multivariate analysis was employed to identify the potential factors for untoward effects on the skin from the use of PPE.
Results: A total of 415 HCWs responded to the questionnaire. The survey found three types of untoward effects on the skin. Among all, 389 (93.7%) had mask-related effects on the skin, 318 (76.6%) had glove-related effects on the skin, and 89 (21.4%) had gown-related effects on the skin. There was a significant association between the gender, the occupation, the level of PPE, the duration of use of PPE, and the moisture received during the use of PPE and the untoward effects on the skin.
Conclusion: Untoward effects on the skin from the use of PPE among HCWs are quite common Educating HCWs on these effects may help them to report early and receive proper care.
Key words: PPE (personal protective equipment); COVID-19 (coronavirus disease 2019); untoward skin effects
INTRODUCTION
COVID-19 (coronavirus disease 2019), which emerged in Wuhan, China, in December 2019, is caused by SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2). With no remedy to date, the virus has become a boundless pandemic, with 17 million cases and 600,000 mortalities across the world, with no differentiation between the poor and the rich [1]. SARS-CoV-2 is primarily transmitted through respiratory droplets (> 5–10 µm) and direct contact. Airborne transmission is possible during procedures and treatments that generate aerosols [2]. The fact that respiratory droplets and direct contact are the established routes of transmission of SARS-CoV-2 emphasizes the need for the use of appropriate PPE (personal protective equipment) by HCWs (healthcare workers) treating COVID-19 patients.
PPE is designed to provide protection against serious injuries or illnesses resulting from chemical, physical, mechanical, electrical, radiological, and other hazards [3]. PPE comprises equipment that protects the mouth, nose, eyes, ears, bare skin, and other vulnerable parts depending on one’s working environment [4]. PPE includes items such as gloves, safety glasses and shoes, earplugs, hoods, respirators, coveralls, vests, and full-body suits [5]. Based on the degree of protection provided, PPE is classified into four categories. Level A comprises an encapsulated suit and a self-contained breathing apparatus that provides the highest level of protection available for both contact and inhaled threats. Level B comprises an encapsulating suit or junction seams sealed with a supplied air respirator or a self-contained breathing apparatus that provides a high level of protection adequate for unknown environmental entry and a supplied air ensemble with increased mobility and dexterity. Level C comprises a splash suit and an air-purifying respirator that provides significantly increased mobility and decreased physical stress with extended periods of time with no fit testing required for the hood. Level D comprises work clothes and standard precautions such as surgical masks, gloves, and splash protection, providing the lowest level of respiratory and skin protection [6].
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) recommend N95 masks for HCWs caring for patients suspected or confirmed to have highly transmissible respiratory infections. The N stands for NIOSH (National Institute for Occupational Safety and Health), and the 95 indicates filter efficiency. Thus, an N95 mask is 95% efficient at filtering particles 300 nm in size and larger [7]. An N95 mask is made from a fine mesh of synthetic polymer fibers, often a non-woven polypropylene fabric, produced by melt-blowing to form filtration layers against hazardous particles. Gloves for medical examination, which act as a barrier against possible transmission of infection, are made from latex or synthetic materials, such as nitrile or vinyl. Gowns used for isolation and protection are made from non-woven materials such as polypropylene, polyester, or polyethylene alone or in combination [8]. Because no single protective equipment is capable of protecting against all hazards, PPE should be used in conjunction with other protective methods, including exposure control procedures and equipment. The use of PPE causes significant discomfort and, thus, impairs the wearer’s ability to perform work. Choosing well-fitting PPE based on the expected exposure provides the wearer with a comfortable environment to perform their work. However, the use of PPE may cause certain skin problems due to long-term sealing, friction, and pressure [4]. As reported by Foo et al. [9], the most common adverse reaction to an N95 mask is acne, followed by itch (caused by gloves) and rash (caused by gowns).
India reported its first COVID-19 case on January 30, 2020. Despite aggressive lockdown measures, confirmed cases continued to rise on a daily basis, reaching one million cases on July 17, 2020 [10]. In March 2020, some of our colleagues teleconsulted us for skin reactions after the use of PPE during the treatment of COVID-19 patients. For this reason, we began to suspect that the untoward effects on the skin from PPE were more common than expected and, thus, we decided to explore this issue in a study.
MATERIALS & METHODS
Study Design
A cross-sectional study was conducted from April to June 2020 at a tertiary care center in Bengaluru, a dedicated hospital for the treatment of COVID-19 cases.
Data Collection
A questionnaire was prepared to determine the untoward effects on the skin from the use of PPE among HCWs treating COVID-19 patients. The questionnaire was revised after reviewing articles and feedback from the medical and nursing staff. The questionnaire included demographic data (age, sex, occupation, place of work), information on the use of PPE (grade of PPE, duration of use of PPE, sweating during the use of PPE) and the untoward effects on the skin due to wearing masks, gloves, and gowns, as well as and the aftercare received. The questionnaire was distributed among HCWs as an online document by e-mail and social media such as WhatsApp. Participants who voluntarily filled the questionnaire and submitted it within a week were included in the study.
Statistical Analysis
Univariate analysis was performed first to identify the potential factors for the untoward effects on the skin from the use of PPE with a chi-squared test. A p value below 0.05 was considered significant and these variables were entered for multivariate analysis. All analysis was done with the SPSS software, version 20.0.
RESULTS
A total of 415 HCWs responded to our questionnaire. The mean age was 29.43 ± 3.8 years. 371 (89.4%) were less than 35 years of age and 44 (10.6%) were 35 years of age or older.
191 (46%) were male and 224 (54%) were female. 314 (75.7%) were doctors and 101 (24.3%) were nursing staff. 77 (18.6%) were working in a screening OPD, 286 (68.9%) in a COVID ward, and 52 (12.5%) in both a screening OPD and a COVID ward. 399 (96.1%) and 16 (3.9%) wore level B and level C PPE, respectively. 33 (8%) wore PPE for 3 hours, 48 (11.5%) for 3–6 hours, and 334 (80.5%) for more than 6 hours a day. Two layers of gloves were worn by 132 (31.8%) and three layers of gloves were worn by 283 (68.2%). The frequency of handwashing during the day was more than ten times in 220 (53%) and less than or equal to ten times in 195 (47%).
The survey found three types of untoward effects on the skin. 389 (93.7%) had mask-related effects on the skin, 318 (76.6%) had glove-related effects on the skin, and 89 (21.4%) had gown-related effects on the skin (Table 1). 72.5% reported a pressure effect on the skin due to the use of a mask, 47.5% had vague itching on the face, 35.9% had dry skin, 26.7% had pigmentation on the nasal bridge, 26.5% had a flare of acne, and 10.6% had folliculitis. 1.2% reported herpes simplex on the nose and the perinasal area. Additionally, 5.8% reported having a runny nose, and 0.5% had a worsening of their asthma due to the regular and prolonged use of a mask. Glove-related effects on the hands were noted, such as itching in 58.8% of cases, dry skin in 47.7%, redness in 14%, and a pressure effect in 12.5%. Gown-related effects were noted on the trunk, axilla, and groin, such as itching in 15.2% of cases, dry skin in 3.4%, redness in 2.4%, and a pressure effect in 5.5%.
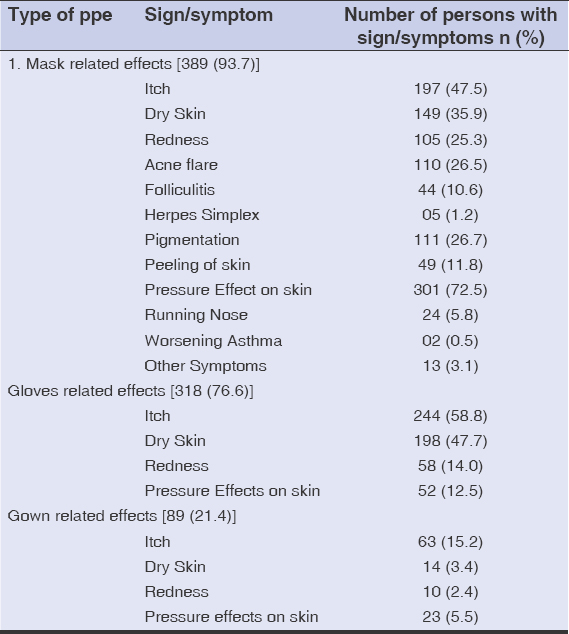 |
Table 1: Prevalence of untoward effects on the skin after the use of PPE. |
Table 2 shows the anatomical distribution of the untoward effects on the skin from the use of PPE, with the brunt on the hands 318 (76.6%), followed by the nose 291 (70%).
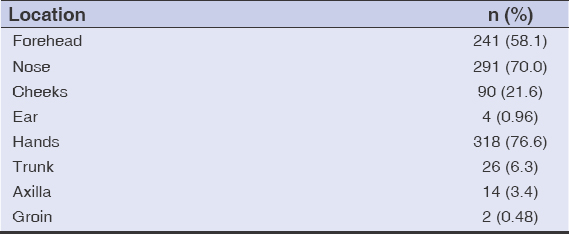 |
Table 2: Anatomical distribution of untoward effects on the skin. |
The data collected was subjected to univariate analysis, and a chi-squared test was employed to compare the categorical values (Table 3). There was a significant association between the gender, the occupation, the level of PPE, the duration of use of PPE, the moisture received during the use of PPE, and the untoward effects on the skin.
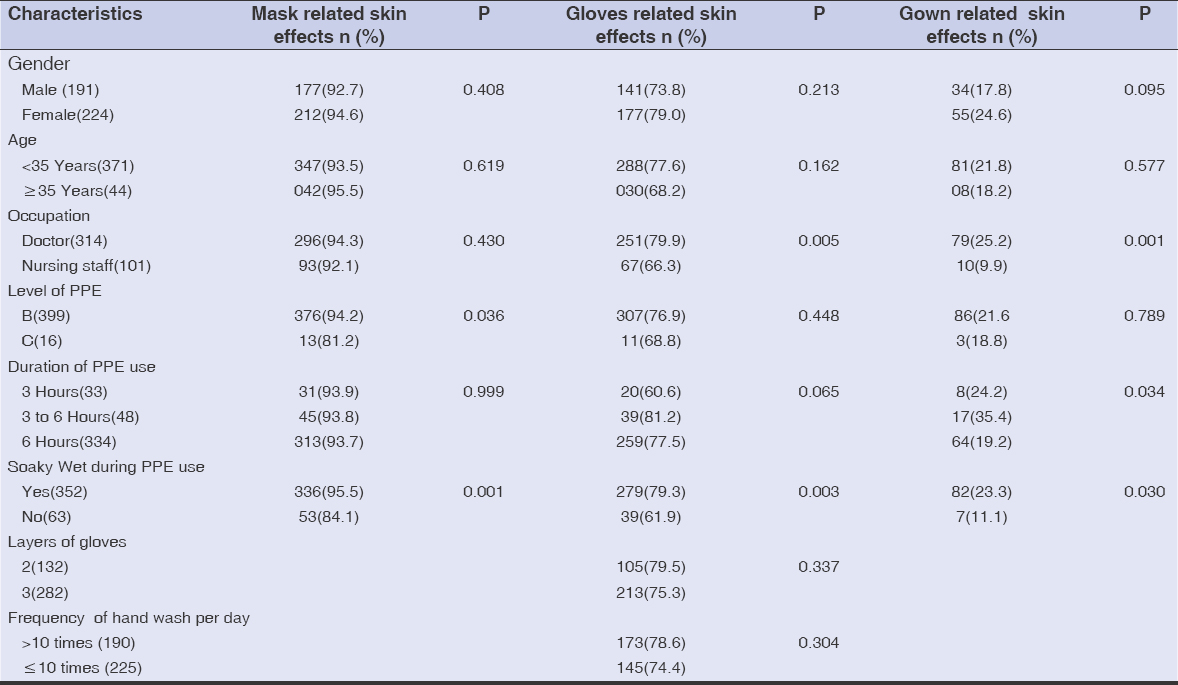 |
Table 3: Univariate analysis of untoward effects on the skin |
Characteristics with a p value less than 0.05 on univariate analysis were subjected to multivariate analysis with logistic regression (Table 4). Skin injuries were set as the dependent variable (0: absent; 1: present), and the single factors of a p value less than 0.05 (Table 3) were set as the independent variable.
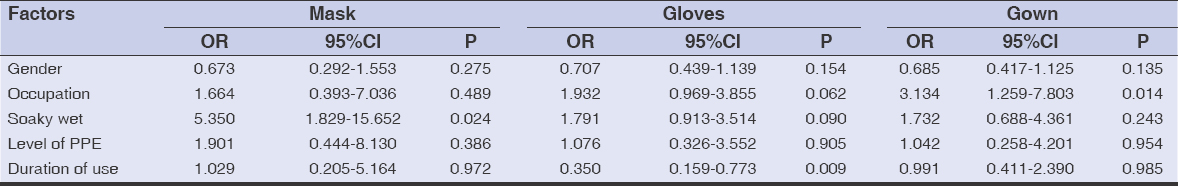 |
Table 4: Multivariate analysis of factors associated with untoward effects on the skin |
An odds ratio (OR) above 1 suggested a positive association between the mask-related effects and the occupation, the moisture received during the use of PPE, the level of PPE, and the duration of use of PPE. Also, a positive association was seen between glove- and gown-related effects and the occupation, the moisture received during the use of PPE, and the level of PPE. In our study, 75.7% of participants were doctors and 24.3% were nursing staff, so the association between the occupation and the untoward effects needs to be further evaluated. The Hyperhidrosis Disease Severity Scale (HDSS) was employed to assess the severity of sweating. The mean score during the use of PPE was 1.95 while, otherwise, it was 1.19, with a significant p value of 0.001, which suggests that most HCWs tend to sweat profusely, contributing to the untoward effects on the skin.
As a method of aftercare for untoward effects on the skin, 346 (83.4%) used moisturizers, 93 (22.4%) used soothing lotions, 26 (6.3%) needed an antibiotic, either orally or topically, and 1 (0.2%) needed to dress the wound for a week.
Figures 1a – 1f show clinical pictures of untoward effects on the skin from the use of PPE observed in our study.
DISCUSSION
HCWs (healthcare workers) are at the frontline of treating COVID-19 patients, wearing PPE for long hours and, therefore, being susceptible to PPE-related untoward effects. In our study, the most prevalent untoward effect on the skin from the use of PPE were mask-related effects, followed by glove-related and gown-related. This predominance in mask-related effects might be due to the greater number of sebaceous glands and a moderate number of eccrine sweat glands on the face, which may trigger acne and increase sweating, respectively.
The pressure effect of the mask on the bridge of the nose—the most frequent untoward effect of a mask—is due to the anatomical structure of the face, in which the nose is the most protruding element. The forehead was the second most common site for untoward effects, such as acne and folliculitis, which were due to the distribution and occlusion of the pilosebaceous ducts and the pressure effect by goggles, face shields, or surgical caps pressing on the forehead. These were the contributing factors for the untoward effects on multiple parts of the face.
This was similar to the observation made by Jiang et al. [11] in a study among medical staff in China, noting that device-related pressure injuries were more common than moisture-associated effects. A similar observation was made by Foo et al. [9] and Lin et al. [12]. We found little pressure effect on the ear, as the type of N95 mask that was used had overhead straps, not ear straps. The herpes simplex cases may be attributed to the reactivation of the virus due to the stress and anxiety in treating COVID-19 patients. A homeostatic interaction model suggests that the hypothalamic–pituitary–adrenal axis, especially corticosteroids, is the primary driving force of stress-induced secondary immune deficiencies that impairs viral clearance and, hence, may predispose to the reactivation of the herpes virus [13].
Dry skin, itch, and redness were also reported frequently on the face, hand, and trunk, probably from the frequent handwashing and bathing and the use of soaps and sanitizers, as well as contact dermatitis from the components of the mask, such as the rubber straps or metal clips, the gloves, and the fabric of the gown. Additional factors responsible for untoward effects are heavy and airtight PPE that makes it difficult to volatilize perspiration, thus changing the microclimate of the skin and decreasing skin tolerance. Soaked skin due to sweat combined with pressure increases the friction coefficient between the PPE and skin, thus causing abrasions and peeling of the skin [14].
Hence, promoting education on the proper use of PPE and restricting the duration of wearing PPE to not more than six hours a day may, at the administrative level, help in reducing the untoward effects on the skin. At the personal level, HCWs should be encouraged to follow the standards of the use of gloves, hand hygiene, and skincare. In the case of severe dermatoses or sustained aggravation of existing dermatoses, a dermatological referral is recommended [12].
Limitations
The limitations of this study were subjective evaluation of skin changes (self-perceived skin changes) and a small sample size.
CONCLUSION
The study suggests that all HCWs should be educated on the possible skin effects from the use of PPE and on the protective measures available for reducing these effects, such as prophylactic dressings and creams suitable for different parts of the body that would effectively keep the moisture balance and prevent fogging of the goggles.
According to the author’s knowledge, this is one of the pioneer questionnaire-based studies conducted in India relating to untoward effects on the skin from the use of PPE among HCWs.
Ethical Approval
Ethical approval was obtained from the Institutional Ethics Committee.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Garg S, Garg M, Prabhakar N, Agarwal R. Unravelling the mystery of Covid-19 cytokine storm:From skin to organ systems. Dermatol Therapy. 2020;e13859:1-8.
2. World Health Organization. (2020, March 29). Modes of transmission of virus causing COVID-19:implications for IPC precaution recommendations:scientific brief. Geneva:World Health Organization;Available from https://apps.who.int/iris handle/10665/331616. ( last accessed August 28, 2020).
3. Chemical Hazard Emergency Medical Management (CHEMM). Personal Protective Equipments. Retrieved from:https://chemm.nlm.nih.gov/ppe.htm. (last accessed August 28, 2020).
4. Zhou N, Yang L, Dong L, Li Y, An X, Yang L, Huang C, et al. Prevention and treatment of skin damage caused by personal protective equipments:experience of the first- line clinicians treating 2019-nCov infection. Int J Dermatol Venerol. 2020;10.1097/JD9.0000000000000085.
5. Safety and Health topics:Personal Protective Equipments [OSHA]. (2004). Retrieved from:http://www.osha.gov/personal-protective-equipment6. (last accessed August 8, 2020).
6. Hick JL, Hanfling D, Burstein JL, Markham J, Macintyre AG, Barbera JA, et al. Protective equipment for health care facility decontamination personnel:regulations, risks, and recommendations. Ann Emerg Med. 2003;42:370-80.
7. Chee Y C. SARS and PPE. SMA News. 2003;35:17–22.
8. N95 MASK. (2020,July 20).In Wikipedia. Retrieved from https://en.m.wikipedia.org/wiki/N95_mask. ( last accessed August 26, 2020).
9. Foo CC, Goon AT, Leow YH, Goh L C. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome-a descriptive study in Singapore. Contact Dermatitis. 2006;55:291-94.
10. COVID-19 Pandemic in India. (2020, January 30).In Wikipedia. Retrieved from:https//en.m.wikipedia.org/wiki COVID-19_pandemic_in_India. (last accessed August 28,2020)
11. Jiang Q, Song S, Zhou J, Liu Y, Chen A, Bai Y, et al. The prevalence, characteristics, and prevention status of skin injury caused by personal protective equipment among medical staff in fighting COVID-19:A multicenter, cross-sectional study. Adv Wound Care (New Rochelle). 2020;9:357-64.
12. Lin P, Zhu S, Huang Y, Li L, Tao J, Lei T, et al. Adverse skin reactions among healthcare workers during the coronavirus disease 2019 outbreak:a survey in Wuhan and its surrounding regions. Br J Dermatol. 2020;183:190-2.
13. Uchakin PN, Parish DC, Dane FC, Uchakina NO, Sscheetz PA, Agarwal KN, et al. Fatigue in medical residents leads to reactivation of herpes virus latency. Interdiscip Perspect Infect Dis. 2011;2011:571340.
14. Zulkowski K. Understanding moisture-associated skin damage, medical adhesive-related skin injuries, and skin tears. Adv Skin Wound Care. 2017;30:372–81.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-6820-7492 http://orcid.org/0000-0002-6820-7492 |




Comments are closed.