Cutaneous squamous cell carcinoma (cSCC) arising from a chronic skin fistula: A case report
Hassane Ait Ali , Brahim Zeriouh, Usman Ebo Egyir, Mohamed Chablou, Tariq Bouhout, Badr Serji, Tijani Elharroudi
, Brahim Zeriouh, Usman Ebo Egyir, Mohamed Chablou, Tariq Bouhout, Badr Serji, Tijani Elharroudi
Department of Oncological Surgery of the University Hospital Center Mohamed VI, Oujda, Morocco
Corresponding author: Hassane Ait Ali, MD
Submission: 18.10.2020; Acceptance: 25.12.2020
DOI: 10.7241/ourd.20213.11
Cite this article: Ait Ali H, Zeriouh B, Ebo Egyir U, Chablou M, Bouhout T, Serji B, Elharroudi T. Cutaneous squamous cell carcinoma (cSCC) arising from a chronic skin fi stula: A case report. Our Dermatol Online. 2021;12(3):280-284.
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Squamous cell carcinoma (SCC) of the skin is the second most common form of skin cancer, characterized by abnormal, accelerated growth of squamous cells. We describe an unusual case of cSCC developing in a 38-year-old patient with a chronic skin fistula of the knee after a trauma in childhood. Multiple surgical biopsies were taken from the tumor site, which revealed the development of cutaneous squamous cell carcinoma. MRI revealed a tumor located on the skin. The patient was treated with a large surgical resection of the tumor with safety margins. A histological examination revealed a well-differentiated cSCC. After three years of follow-up, no recurrence was observed. The development of cSCC in a chronic skin fistula of the knee is rare. The diagnosis is often made by histological examination of biopsies. Malignant transformation should be suspected in a chronic skin fistula with recurrent episodes of inflammation, repeated purulent discharge, poor healing, and a chronic fistula.
Key words: Cutaneous squamous cell carcinoma; Chronic knee fistula; Chronic inflammation of the skin
INTRODUCTION
Basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC) are the first and second most common types of skin cancer, respectively. Other significant skin lesions are actinic keratosis and melanoma.
Actinic keratosis and basal cell carcinoma are easily excised and have a very good prognosis, whereas cSCC has a poor prognosis, especially if it invades the lymph nodes and adjacent structures.
It may also appear in any area of ??the skin, especially in areas exposed to the sun. It may develop on healthy skin as well, but is, still, more likely to develop on damaged skin.
The literature has proposed ultraviolet-light exposure, genetics, carcinogens, immunosuppression, and trauma as etiologies [1].
Squamous cell carcinoma (SCC) occurs when DNA damage from exposure to ultraviolet radiation or other damaging agents trigger abnormal changes in squamous cells.
The clinical suspicion of cSCC in a chronic skin fistula of the knee is low, leading to a delayed diagnosis and treatment.
We report an extremely rare case of cSCC developing in a 38-year-old male with a chronic knee fistula after a childhood knee trauma.
CASE REPORT
A 38-year-old male presented himself with a traumatic history of the right knee without fracture at 6 years of age. The right knee had developed a secondary infection with a chronic fistula showing discontinuous purulent discharge. The patient had received discontinuous antibiotic treatments for thirty years. The past medical history was unremarkable.
A physical examination revealed a budding crusty ulcerative lesion 3 × 3 cm in size and a skin fistula with purulent discharge on the right knee formed by chronic inflammation (Fig. 1).
 |
Figure 1: An image showing a cutaneous squamous cell carcinoma of the knee with excision limits. |
An examination of the lymph nodes showed no inguinal lymphadenopathy or other lymphadenopathy.
The patient underwent a surgical biopsy of the skin at 38 years of age.
The pathological diagnosis was cutaneous squamous cell carcinoma (cSCC) of the knee.
MRI revealed a skin lesion of the right knee located on the skin below the patella without locoregional invasion (Figs. 2 and 3).
 |
Figure 2: MRI of the knee showing a localized tumor in the skin. |
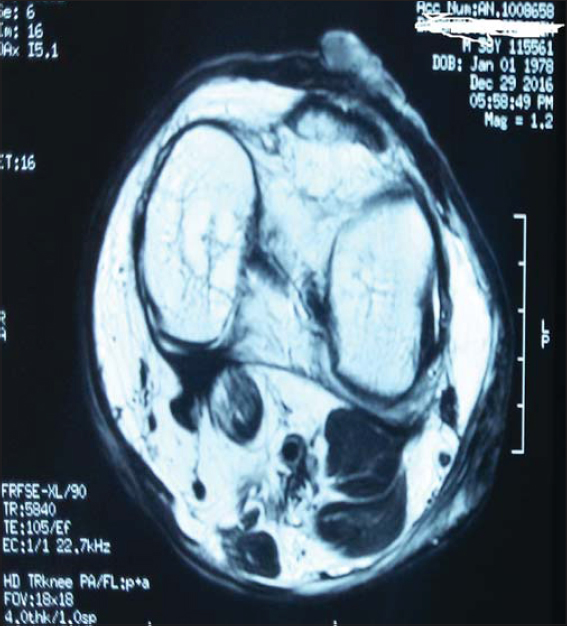 |
Figure 3: Cross-sectional MRI of the knee showing a localized tumor in the skin. |
The clinical diagnosis based on the imaging findings and the pathological diagnosis was SCC arising from a chronic skin fistula after childhood trauma of the knee. Staging for nodal disease was negative.
The patient underwent wide surgical excision of the tumor with safety margins.
On a four-year follow-up, the patient was doing well and revealed no local recurrence or distant metastasis.
DISCUSSION
The skin is a unique epithelial tissue covering the body and providing physical and biological surface protection. It is composed of three layers: the epidermis, the dermis, and the subcutaneous layer.
There are four major types of skin malignancies: basal cell carcinoma, squamous cell carcinoma, melanoma, and non-epithelial skin cancers [2].
Cutaneous squamous cell carcinoma (cSCC) arises from malignant proliferation of epidermal keratinocytes. cSCC is the second most common skin cancer in the U.S., representing around 20% of all skin cancers [3–5].
The risk factors of skin carcinogenesis include chronic cutaneous inflammation, viral infection, ultraviolet radiation (UVR), and other inflammation-inducing agents and traumas [6,7].
Squamous cell carcinoma most commonly appears after the age of 50 in areas of past sun exposure and typically occurs in males with light skin and light eyes and with a history of UV solar radiation exposure. However, anyone with a history of significant UV exposure, whether from past medical treatment or the sun, is at an increased risk. Squamous cell carcinoma is also considerably prevalent in patients who are immunosuppressed and, in these patients, may develop into aggressive subtypes [8–10].
UV radiation is accepted as the major risk factor for squamous cell carcinoma of the skin.
Tanning lamps, therapeutic UV exposure, and ionizing radiation are all well-known risk factors for the development of squamous cell carcinoma.
Extrinsic factors, such as ultraviolet light from sun exposure, are linked to cSCC, while intrinsic factors, such as the use of antioxidants, aspirin, and nonsteroidal anti-inflammatory drugs (NSAIDs) [11], are reported to reduce the risk of developing the disease [12].
It is now clear that pro-inflammatory immune cells play an important role in skin cancer development.
Chronic inflammation is linked to the development and progression of multiple cancers, including those of the lung, stomach, liver, colon, breast, and skin. Inflammation not only drives the oncogenic transformation of epithelial cells under the stress of chronic infection and autoimmune diseases, but also promotes the growth, progression, and metastatic spread of cancers.
Inflammation is characterized by the infiltration of plasma and leukocytes to tissues, which undergo disrupted homeostasis. The causes of inflammation range from pathogenic infection and tissue injury to tissue stress and malfunction, but the process of inflammation may bring detriment to the host, depending on the nature, duration, and magnitude of the inflammatory response elicited during infection or disease.
The pathophysiology of malignant degeneration of chronic wounds and irritation has been elucidated [13]. Chronic irritation and injury of the skin cause constant epithelial regeneration and ulceration, leading to dysplasia and eventual carcinoma.
The sites of chronic inflammation at risk of cSCC development are diverse and include scars, burns, chronic ulcers, sinus tracts, and inflammatory dermatoses, such as lichen sclerosus and atrophicus [14], but cSCC after a knee trauma and a chronic skin fistula in the knee are rare.
SCCs may appear as scaly red patches, open sores, rough, thickened or wart-like skin, or raised growths with a central depression. At times, SCCs may crust over, itch, or bleed. The lesions most commonly arise in sun-exposed areas of the body, but may also occur in other areas of the body, including the genitals.
A biopsy should be performed on any lesion suspected of being a cutaneous neoplasm.
All patients suspected of or diagnosed with a cSCC should undergo a regional LN examination. Any enlarged nodes should be examined histologically either by fine-needle aspiration or an excisional biopsy.
Common therapies for invasive cSCC include surgical excision, electrodesiccation and curettage (ED&C), Mohs surgery, cryotherapy, and radiation therapy [15].
Surgical excision is the primary treatment option [16,17]. The current mainstay treatment is complete surgical clearance of the lesion with histologically clear margins. Knowing that the majority of SCCs may easily and successfully be treated, if allowed to grow, these lesions may become disfiguring, dangerous, and even deadly, or may become invasive and grow into the deeper layers of the skin and spread to other parts of the body. On the other hand, because of the rate of metastasis from locally recurrent tumors arising from sun-damaged skin, the selection of the right treatment for each primary tumor is crucial to avoid unnecessary critical outcomes.
The optimal treatment may be determined by a multidisciplinary team involving input from a dermatologist, Mohs surgeon, surgical oncologist, vascular surgeon, and radiation oncologist, especially for complicated cases. A multidisciplinary evaluation may guide treatment decisions in order to minimize risk without compromising efficacy.
Tumor-positive nodes should be managed by aggressive surgical resection of all local and regional disease.
The addition of adjuvant radiation to lymphadenectomy may result in higher healing rates, which Veness reported to be 73% five-year disease-free survival (DFS) [18]. Thus, early detection of nodal metastasis may improve the outcome of a high-risk cSCC.
The use of chemotherapy in the management of a high-risk cutaneous cSCC remains relatively unexplored.
Regular follow-up after treatment is necessary, including physical examination and palpation of lymph node areas. The appearance of a cSCC should be documented histologically and treatment determined by a multidisciplinary team.
CONCLUSION
The cSCC is less common than basal cell carcinoma (BCC), but the number of reported SCC cases has been steadily increasing.
Cutaneous squamous cell carcinoma (cSCC) may develop on sites of chronic inflammation, including chronic skin fistulas.
The development of a cSCC in a chronic skin fistula of the knee is rare. Symptoms are usually attributed to chronic inflammation and diagnosis is often reached late by a histological examination of biopsies. Therefore, malignant transformation should be suspected in a chronic skin fistula of the knee, with recurrent episodes of inflammation, repeated purulent discharge, and poor healing. A histopathological study of multiple biopsies allows making an accurate diagnosis of cSCC and initiate surgical excision, with or without adjuvant radiotherapy as the appropriate treatment.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from the patient.
REFERENCES
1. Mullenders LHF. Solar UV damage to cellular DNA:from mechanisms to biological effects. Photochem Photobiol Sci. 2018;17:1842-52.
2. Chen AC, Halliday GM, Damian DL. Non-melanoma skin cancer:Carcinogenesis and chemoprevention. Pathology. 2013;45:331-41.
3. Karia PS, Han J, Schmults CD. Cutaneous squamous cell carcinoma:Estimated incidence of disease, nodal metastasis, and deaths from disease in the United States, 2012. J Am Acad Dermatol. 2013;68:957-66.
4. American Academy of Dermatology. Squamous cell carcinoma:tips for managing. https://www.aad.org/public/diseases/skin-cancer/squamous-cell-carcinoma#tips. Accessed December 5, 2018.
5. Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the U.S. population, 2012. JAMA Dermatol. 2015;151:1081-6.
6. Maru GB, Gandhi K, Ramchandani A, Kumar G. The role of inflammation in skin cancer. Adv Exp Med Biol. 2014;816:437-69.
7. Lund AW, Medler TR, Leachman SA, Coussens LM. Lymphatic vessels, inflammation, and immunity in skin cancer. Cancer Discov. 2016;6:22-35.
8. Okhovat JP, Beaulieu D, Tsao H, Halpern AC, Michaud DS, Shaykevich S, et al. The first 30 years of the American Academy of Dermatology skin cancer screening program:1985-2014. J Am Acad Dermatol. 2018;79:884-91.
9. Laprise C, Cahoon EK, Lynch CF, Kahn AR, Copeland G, Gonsalves L, et al. Risk of lip cancer after solid organ transplantation in the United States. Am J Transplant. 2019;19:227-37.
10. Larese Filon F, Buric M, Fluehler C. UV exposure, preventive habits, risk perception, and occupation in NMSC patients:A case-control study in Trieste (NE Italy). Photodermatol Photoimmunol Photomed. 2019;35:24-30.
11. Muranushi C, Olsen CM, Pandeya N, Green AC. Aspirin and nonsteroidal anti-inflammatory drugs can prevent cutaneous squamous cell carcinoma:A systematic review and meta-analysis. J Invest Dermatol. 2015;135:975-83.
12. Howell JY, Ramsey ML. squamous cell Skin cancer. In:StatPearls [Internet]. Treasure Island (FL):StatPearls Publishing;2020 Jan. 2020 Aug 8.
13. Coghill AE, Johnson LG, Berg D, Resler AJ, Leca N, Madeleine MM. Immunosuppressive medications and squamous cell skin carcinoma:Nested case-control study within the skin cancer after organ transplant (SCOT) cohort. Am J Transplant. 2016;16:565-73.
14. Carlson JA, Ambros R, Malfetano J, Ross J, Grabowski R, Lamb P, et al. Vulvar lichen sclerosus and squamous cell carcinoma:A cohort, case control, and investigational study with historical perspective;implications for chronic inflammation and sclerosis in the development of neoplasia. Hum Pathol. 1998;29:932-48.
15. Karia PS, Han J, Schmults CD. Cutaneous squamous cell carcinoma:Estimated incidence of disease, nodal metastasis, and deaths from disease in the United States, 2012. J Am Acad Dermatol. 2013;68:957-66.
16. Maubec E. Update of the management of cutaneous squamous-cell carcinoma. Acta Derm Venereol. 2020;100:adv00143.
17. Corchado-Caobos R, García-Sancha N, González-Sarmiento R, Pérez-Losada J, Cañueto J. Cutaneous squamous cell carcinoma:From biology to therapy. Int J Mol Sci. 2020;21:2956.
18. Veness MJ, Morgan GJ, Palme CE, Gebski V. Surgery and adjuvant radiotherapy in patients with cutaneous head and neck squamous cell carcinoma metastatic to lymph nodes:Combined treatment should be considered best practice. Laryngoscope. 2005;115:870-5.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.