Heat dermabrasion with needle diathermy combined with 35% TCA peeling as an innovative therapy for acne scarring in patients with a dark complexion
Khalifa E Sharquie 1, Raed I Jabbar2
1, Raed I Jabbar2
1Department of Dermatology, College of Medicine, University of Baghdad. Medical City Teaching Hospital, Baghdad, Iraq, 2Department of Dermatology, Fallujah Teaching Hospital, Al-Anbar Health Directorate, Anbar, Iraq
Corresponding author: Prof. Khalifa E Sharquie, MD PhD
How to cite this article: Sharquie KE, Jabbar RI. Heat dermabrasion with needle diathermy combined with 35% TCA peeling as an innovative therapy for acne scarring in patients with a dark complexion. 2021;12(3):230-237.
Submission: 06.11.2020; Acceptance: 11.01.2021
DOI: 10.7241/ourd.20213.1
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Numerous techniques have been introduced to correct acne scarring, such as acid and laser peeling and mechanical and CO2 dermabrasion.
Objective: The aim was to find a new, simple, and cheap technique for improving and correcting acne scarring.
Patients and methods: This interventional therapeutic study started in 2013 and lasted until 2020. A total of 250 patients with acne scarring were included, with the age ranging from 20 to 45 years. Most scar severity ranged from moderate to severe. The common types of scars were boxcar, icepick, and mixed. After local xylocaine anesthesia, direct heated needle diathermy was applied to the whole skin that included the scars and two passing were done superficial and deep, followed by a TCA peel. These patients were given topical antiseptic washing agents with oral antibiotics and 10 mg prednisolone once a day to be seen again after two weeks. Scoring was done to assess the reduction rate in the scars during follow-up periods.
Results: Reduction rate scores after four months were as follows: a moderate score in 10 (4%) patients, a marked score in 140 (56%) patients, and an excellent score in 100 (40%) patients. No important complications were observed apart from temporary hyperpigmentation. Patients with active acne lesions also had a full remission following the dermabrasion. Full satisfaction was expressed by 225 (90%) patients, while partial by 25 (10%).
Conclusion: This simple, easy, clean, and cheap innovative technique for dermabrasion was conducted on an outpatient basis with two-week downtime, showing marked (56%) to excellent (40%) reduction rates in acne scars within one session.
Key words: Heat dermabrasion; Diathermy; TCA peeling; Acne scarring
INTRODUCTION
Acne is a common chronic inflammatory skin disease experienced by most adolescents and young adults with a prevalence of over 90% among adolescents [1]. The pathogenesis of acne lesion formation and scarring involves the interplay of a variety of factors, including follicular hyperkeratinization, excess sebum production, inflammation mediated by Propionibacterium acnes, and other normal skin flora and immunological reactions [2].
Acne Scars
Acne lesions may result in permanent scarring with a marked impact on the quality of life. Scars affect a high percentage of patients with acne vulgaris. Genetic factors, disease severity, and delay in treatment are the important factors influencing scar formation [3,4].
Clinical Classification
Acne scars are classified into three basic types according to the depth, width, and three-dimensional structure [5].
- Icepick scars: narrow (less than 2 mm in diameter), deep, sharply marginated, and depressed tracks extending into the dermis or subcutaneous tissue.
- Boxcar scars: oval to round depressions with sharply demarcated vertical borders; wider at the surface than icepick scars; may be shallow (0.1–0.5 mm) or deep (≥ 0.5 mm), with its diameter varying from 1.5 to 4.0 mm.
- Rolling scars: occur from dermal tethering of otherwise relatively normal-appearing skin; usually wider than 4 to 5 mm in diameter.
Other clinical entities included in this classification are hypertrophic scars, keloidal scars, and sinus tracts.
Treatment of Acne Scars
The treatment of acne scars may be classified into topical, procedural, surgical, and laser.
Topical Agents for Acne Scars
- Topical retinoids: Topical retinoids, including tretinoin, tazarotene, and adapalene, work in several ways of anti-inflammatory action by decreasing the potential for the development of acne scars [6].
- Topical antimicrobial agents: These agents produce anti-inflammatory action through decreasing populations of Propionibacterium acnes. Benzoyl peroxide also exhibits moderate comedolytic action [7].
- Topical corticosteroids: Intralesional steroid injections treating hypertrophic and keloidal acne scars are well established [4].
Procedural Methods for Acne Scars
1. Peeling
The peeling methods for the treatment of acne scars include superficial peeling, medium-depth peeling, and deep peeling.
Superficial peels include salicylic acid (25% to 30%), glycolic acid (70%), pyruvic acid (40% and/or 50% to 60%), trichloroacetic acid (TCA) (20% to 30%), and the combination of salicylic acid or Jessner’s peel with TCA. Superficial peels are used to enhance destruction limiting it to the epidermis and upper dermal layers [8].
TCA is the most common chemical substance used as a medium-depth peel. A 35% concentration of TCA peels the skin down to the papillary dermis [8]. The mechanism of action of the TCA peel is not clear but the following mechanisms may be coming into play: decreasing the size of sebaceous glands involved in acne pathogenesis, altering the microflora of the skin by reducing the number of bacteria, mainly Propionibacterium acnes and others that have a role in the pathogenesis of acne vulgaris, and revising the immunological reaction correlated with the acne formation and scarring [9].
Sharquie et al. have used TCA peel 35% and 88 % lactic acid peel effectively in the treatment of active acne vulgaris with or without scarring without acne therapy [10–12].
2. Dermabrasion
Dermabrasion is a skin-resurfacing technique that surgically abrades or planes the epidermis and the upper part of the dermis with an abrasive surface. Dermabrasion completely removes the epidermis and reaches the level of the papillary or reticular dermis, enhancing the remodeling of the skin’s structural proteins [13].
The growing number of applications of dermabrasion have been accompanied by the development of the procedure from the utilization of sandpaper in the mid-twentieth century to electrically powered tools with wire-brush tips or diamond fraises of varying shapes, sizes, and textures. The technique has culminated in its application to a variety of lesions, including facial scars secondary to acne, trauma, and surgery [14,15].
It may also be employed to effectively manage surgical or traumatic scars, irregular scarring from skin grafts, photodamage, some benign tumors, rhinophyma, perioral rhytides, and actinic ketosis [16]. Dermabrasion has been used to manage superficial malignancies such as superficial basal cell carcinoma and squamous cell carcinoma in situ [17].
A novel and safe technique involving heat dermabrasion accompanied by needle diathermy was introduced by Sharquie for the treatment of different types of acne scars and nose volume plastic surgery for a bulky nose under local anesthesia within one session with minimal or no adverse effects [18–23].
3. Microdermabrasion
This is a type of mechanical exfoliation or micro-resurfacing procedure that uses a mechanical medium for exfoliation along with adjustable suction, removing the outermost layer of dead skin cells from the epidermis [24,25].
Laser for Acne Scars
Laser resurfacing includes devices employing ablative, non-ablative, and fractional ablative technologies. The three approaches differ widely in the way of inducing thermal damage, varying degrees of efficacy, downtime, and adverse effect profiles. The fractional laser technology, introduced by Manstein et al. in 2004, represents a major advantage over the older, conventional ablative methods (CO2 and Er:YAG lasers) [26]. Nonetheless, ablative lasers had the advantage of their predictability in the depth of tissue ablation and thermal denaturation [27].
Laser and Light for Acne Scars
The following are used in the treatment of acne scars [28,29].
- CO2 laser: 10,600 nm, ablative and fractional CO2.
- Er:YAG: 2940 nm, ablative and fractional Er:YAG.
- Er:Glass: 1540/1550 nm, non-ablative and fractional.
- Pulsed-dye laser: 585 nm for hypertrophic scars and keloids.
- IPL: for erythematous and hyperpigmented macular scars.
- Nd:YAG: 1064 nm for mild scarring.
- Diode laser: 1450 nm for mild scarring.
The aim of the present study is to find a new simple and effective technique for dermabrasion with direct diathermy heat combined with 35% TCA peeling.
PATIENTS AND METHODS
This clinical, interventional, therapeutic study took place from January 2013 through July 2020 and was conducted by one author (KS).
Two hundred fifty patients with acne scarring were enrolled in the study, 143 (57.2%) females and 107 (42.8%) males. Their age ranged from 20 to 45 years with a mean ± SD of 26 ± 5.101 years. Twenty-five (10%) patients had associated active acne lesions in addition to acne scarring.
Sharquie’s scoring [9,30,31] (Table 1) was used to grade the severity of the acne scars. These were divided into mild, moderate, and severe that involved most of the face, commonly the cheeks, sides of the face, nose, and forehead. No treatment for active acne lesions was administered. The common types of scars were boxcar, icepick, and mixed; five (2%) patients had undulating rolling scars.
 |
Table 1: Sharquie’s scoring to assess the scarring in acne vulgaris |
The study followed the principles of the Declaration of Helsinki and formal written consent was taken from each patient before starting the therapy and after explaining in full detail the nature of the disease, its course, the method of its treatment, the complications, the follow-up period, the prognosis, and the need for before-and-after photos with the twelve-megapixel camera of a Samsung Galaxy Note 9 smartphone at the same place and distance and in the same illumination. Statistical analysis was done with the chi-square test and t-test.
Sharquie’s scoring [11,12] was used to evaluate the reduction rate of acne scars (Table 2).
 |
Table 2: Sharquie’s scoring to assess the reduction rate of acne scarring |
Patient satisfaction from the response to treatment was assessed as follows:
- full satisfaction,
- partial satisfaction,
- no satisfaction.
All patients were of Fitzpatrick’s skin types III and IV.
The exclusion criteria were the coexistence of pregnancy and lactation, the use of any topical or systemic treatments in the previous one month, any other dermatoses involving the face, and an allergy to a medication, as well as a history of recurrent herpes simplex infection, diseases such as diabetes mellitus, and epilepsy, drugs interfering with the clotting system, immune-compromised patients, and unreliable patients.
A solution of 35% TCA consisting of 35 g (United States Pharmacopeia, USP, crystals) in 100 ml of 88% lactic acid was prepared and kept in amber glass flacons to be available for use.
The patients were prepared by cleansing and degreasing the whole face with 70% alcohol and waited several minutes for the alcohol to dry. The face was then wiped with an impregnated gauze with normal saline several times in two directions for further cleaning and sterilization. After local xylocaine anesthesia, direct heated needle diathermy was applied to the whole skin that included the scars and two passing were done superficial and deep until a smooth erythematous surface was reached, followed by two TCA coatings applied until uniform frosting. Immediately, frozen bag compresses were applied. The patients were told that a stinging sensation will peak for two to three minutes and vanish. The patients were given topical antiseptic washing agents with oral antibiotics and 10 mg prednisolone once a day to be seen again after two weeks. Then, the patients were given mild topical corticosteroid cream twice a day combined with oral propranolol 10 mg twice a day for one month to minimize post-inflammatory erythema. The patients were only advised to avoid sun exposure with no need to use sunblock and to be seen again for a follow-up to report on scar reduction, side effects, and relapses.
Follow-ups were scheduled at two weeks, one month, two months, four months, and six months after the interventional therapy.
RESULTS
The severity of the scars was as follows: mild in 15 (6%) patients, moderate in 50 (20%), and severe in 185 (74%).
Reduction rate scores are shown in Table 3. No important complications were observed apart from temporary hyperpigmentation that was noticed in several patients who had gone overtime. Otherwise, there was more hypopigmentation when compared with the non-dermabraded skin. The patients with active acne lesions also had a full remission following the dermabrasion, accompanied by scar reduction without anti-acne therapy. There was not much difference in the response to therapy in the different types of acne scars.
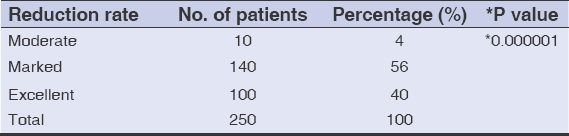 |
Table 3: Reduction rates of acne scarring according to Sharquie’s scoring system |
During the follow-up period, the following were observed:
- Two weeks: erythema still present, scar reduction.
- One month: the same scar reduction as at two weeks but with the erythema almost gone and with five (2%) patients showing hyperpigmentation.
- Two months: the same scar reduction as before and no more pigmentation.
- Four months: no change in scar reduction but improvements in skin texture, with the post-inflammatory hyperpigmentation vanished and with hypopigmentation in many patients.
- Six months: no change in scar reduction but with a further improvement in skin texture and a slight improvement in hypopigmentation.
Sixty patients were also seen after 6 to 12 months with continuous improvement and no relapse. Many patients were also seen accidentally after years and showed a marked improvement and no relapse or pigmentary complications.
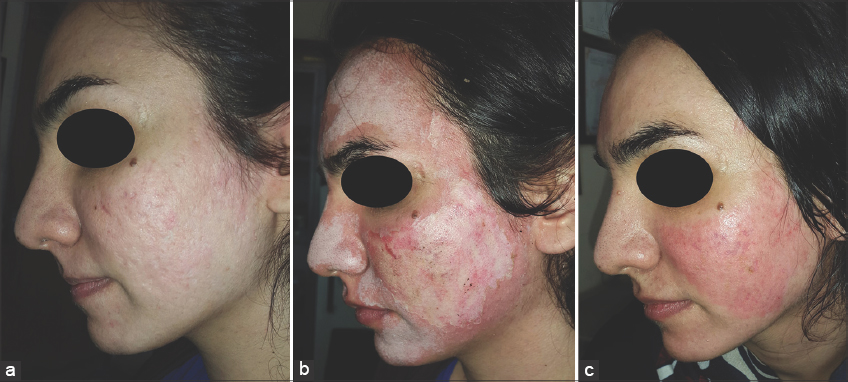
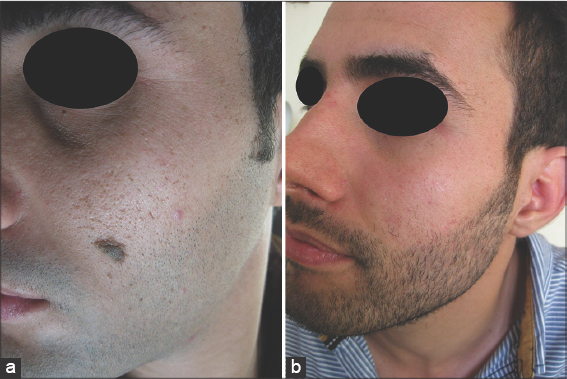
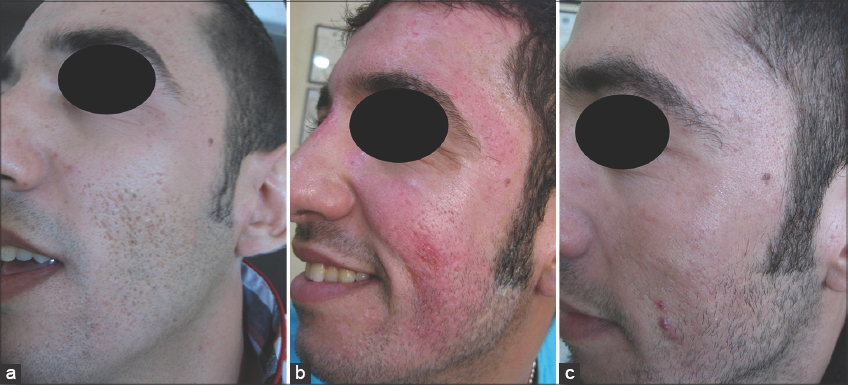
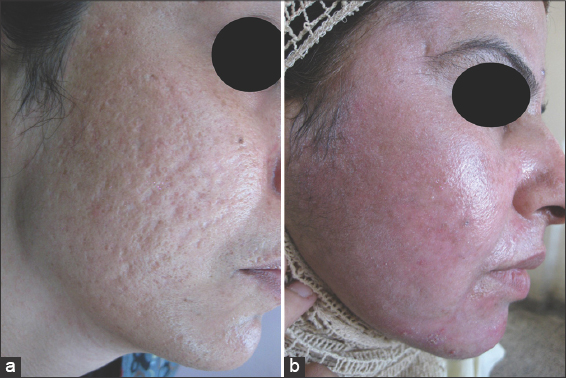
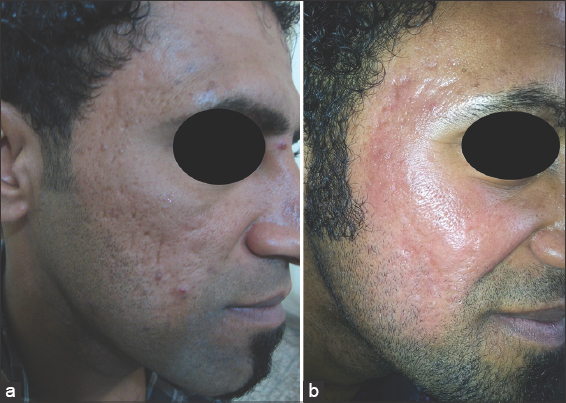
Figs. 1 – 6 show photos of the patients before, at the end of the session, and during the follow-up period.
Full satisfaction was expressed by 225 (90%) patients, while 25 (10%) expressed partial satisfaction. The downtime was around two weeks.
DISCUSSION
Acne is a common chronic inflammatory skin disease experienced by most adolescents and young adults with a prevalence of over 90% among adolescents [1]. The pathogenesis of acne lesion formation and scarring involves the interplay of a variety of factors, including follicular hyperkeratinization, excess sebum production, inflammation mediated by Propionibacterium acnes, and other normal skin flora and immunological reactions [2].
Inflammatory acne lesions may result in permanent scars, the severity of which may depend on the severity of the acne lesion and the delay in treating the acne. About 1% of people have had acne scars, although only 1 in 7 is considered to have “disfiguring scars” [32]. Severe scarring caused by acne is associated with substantial physical and psychological distress, particularly in adolescents [33].
Because acne vulgaris is a major health problem, in which scarring is the most common complication, early treatment is essential in order to prevent disfiguration. There exist numerous methods and techniques for treating and correcting acne scarring. The earliest and oldest technique is mechanical dermabrasion [14,15]. This technique may be effective but often needs general anesthesia. Also, this procedure is messy and bloody as using a brush causes blood contamination to the surroundings, even causing the transmission of infection from patients to the medical staff. Also, it is a costly procedure and may generate complications [34].
CO2 and other lasers have also been used as methods of dermabrasion for acne scars. This is, however, a risky procedure, as lasers require protection for the doctor’s and patient’s eyes, are costly, require significant experience, and may require many sessions to achieve the final cosmetically acceptable outcome [26]. Deep peeling has also been used to correct acne scars, but although this is a simple and cheap procedure on an outpatient basis, it requires many sessions and is not as effective as mechanical or laser dermabrasion, hence it might be reserved for mild scarring [8].
The present work demonstrated a new innovative technique that involves heat dermabrasion with heated needle diathermy combined with 35% TCA peeling.
This is the largest study in the world, achieving marked (56%) to excellent (40%) results, and was done on an outpatient basis under local anesthesia with only one session was needed. It is effective for all types of acne scars, whether icepick, boxcar, or rolling, while, with other procedures, rolling scars are difficult to treat. In all other types of dermabrasion and peeling, the most important complication to be afraid of is long-standing hyperpigmentation [35]. Although, in the present work, there was no permanent hyperpigmentation, the patients usually experienced hypopigmentation of the dermabraded area; all our patients, however, had a dark complexion and were of Fitzpatrick’s skin types III and IV [10–12].
In all techniques of dermabrasion, patients with active lesions of acne vulgaris should avoid this procedure, while 10% of the patients in our work had active acne vulgaris in addition to the scarring, and heat dermabrasion caused a long-term remission of the acne vulgaris in addition to the clearance of the scarring. This has recently been supported by Sharquie et al., who used 35% TCA and 88% lactic acid peeling in the treatment of active acne vulgaris, which induced a long-term remission without drug therapy for acne [11,12]. Some patients with active acne vulgaris express no wish to be treated because of the course of the therapy that was too long, the use of medications, the scarcity of time to be spared for the treatment, or the fear of side effects or complications. In these situations, we may recommend other therapies, such as TCA or lactic acid peeling, laser, or even heat dermabrasion [11,12,22].
The mechanism of action of TCA and lactic acid peeling has not been well documented but is assumed to work by minimizing the size of sebaceous glands involved in acne pathogenesis, by changing the microflora of the skin, which involves reducing the size of the bacterial flora in the acne lesions, and by changing the immunological reactions involved in acne formation and scarring [9]. The same mechanism may also be used in heat dermabrasion with TCA peeling, as shown in the present work.
Propranolol was used in the present work to reduce post-inflammatory erythema and to decrease the probability of hemangioma formation, which might theoretically have occurred because heat dermabrasion may create thermal burns, and this concept was used in the treatment of patients with burn hemangioma [36].
CONCLUSION
This is an innovative technique for treating moderate-to-severe acne scars with the direct contact of a diathermy needle followed by TCA peeling, which gave marked (56%) and excellent (40%) results within only one session. It is an easy, clean, and cheap procedure that may be used on an outpatient basis and without significant complications such as hyperpigmentation. Also, it may be used in the treatment of active acne vulgaris, with acne scarring leading to a long-term remission without acne therapy.
Additionally, this method of dermabrasion may be recommended in the therapy of xeroderma pigmentosum of the face, facial acanthosis nigricans, adenoma sebaceum, and severe facial wrinkling.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Tan JK, Bhate K. A global perspective on the epidemiology of acne. Br J Dermatol. 2015;172:3-12.
2. Williams HC, Dellavalle RP, Garner S. Acne vulgaris. Lancet. 2012;379:361-72.
3. Tan J, Kang S, Leyden J. Prevalence and risk factors of acne scarring among patients consulting dermatologists in the Unites States. J Drugs Dermatol. 2017;16:97-102.
4. Rivera AE. Acne scarring:A review and current treatment modalities. J Am Acad Dermatol. 2008;59:65976.
5. Jacob CI, Dover JS, Kaminer MS. Acne scarring:A classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109-17.
6. Liu P, Krutzik S, Kim J. Cutting edge:All-trans retinoic acid down-regulates TLR2 expression and function. J Immunol. 2005;174:2467-70.
7. Tanghetti E, Popp K. A current review of topical benzoyl peroxide:New perspectives on formulation and utilization. Dermatol Clin. 2009;27:17-24.
8. Goodman GJ. Management of post-acne scarring:What are the options for treatment?Am J Clin Dermatol. 2000;1:3-17.
9. Sharquie KE, Al-Hamdi KI, Noaimi AA, Al-Battat RA. Scarring and none scarring facial acne vulgaris and the frequency of associated skin diseases. Iraqi Postgrad Med J. 2009;8:332-8.
10. Al-Waiz MM, Al-Sharqi AI. Medium depth chemical peels in treatment of acne scars in dark-skinned individuals. Dermatol Surg. 2002;28:1-5.
11. Sharquie KE, Noaimi AA, Al-Janabi EA. Treatment of active acne vulgaris by chemical peeling using TCA 35%. J Cosm Dermatol Science Applications. 2013;3:32-5.
12. Sharquie KE, Noaimi AA, Al-Janabi EA. Treatment of active acne vulgaris by chemical peeling using 88% lactic acid. Our Dermatol Online. 2014;5:337-42.
13. Gozali MV, Zhou B. Effective treatments of atrophic acne scars. J Clin Aesthet Dermatol. 2015;8:33-40.
14. Kromayer E. Rotational instruments as a new tool in dermatologic surgery. Chir Dermatol Ztschr. 1905;12:26.
15. Campbell RM, Harmon CB. Dermabrasion in our practice. J Drugs Dermatol. 2008;7:124-8.
16. Baker TM. Dermabrasion. As a complement to aesthetic surgery. Clin Plast Surg. 1998;25:81-8.
17. Leyngold M, Leyngold I, Letourneau PR, Zamboni WA, Shah H. Basal cell carcinoma and rhinophyma. Ann Plast Surg. 2008;61:410-2.
18. Sharquie KE. Cosmetic therapy of different types of scars by different tools. IMCAS 2016;https://www.imcas.com/en/attend/imcas-world-congress-2016.
19. Sharquie KE. Heat dermabrasion of different types of scars. IMCAS 2018. http://www.imcas.com.
20. Sharquie KE. Nose volumeplasty. IMCAS 2019;https://www.imcas.com/en/attend/imcas-world-congress-2019.
21. Sharquie KE. Iraqi society of dermatology activities. https://www.imcas.com/en/attend/imcas-world-congress-2019.
22. Sharquie KE. Pearls in skin surgery and cosmetology 2019 28th EADV Madrid.eadvprogram.m-anage.com en-GB.
23. Sharquie KE, Al-Jaralla FA. Volumeplasty of bulky nose using heat dermabrasion as a minor therapy. Am J Dermatol Res Rev. 2020;3:18.
24. Spencer JM. Microdermabrasion. Am J Clin Dermatol. 2005;6:89-92.
25. Freedman BM, Rueda-Pedraza E, Waddell SP. The epidermal and dermal changes associated with microdermabrasion. Dermatol Surg. 2001;27:1031-4.
26. Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis:A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34:426-38.
27. Hu S, Chen MC, Lee MC, Yang LC, Keoprasom N. Fractional resurfacing for the treatment of atrophic facial acne scars in Asian skin. Dermatol Surg. 2009;35:826-32.
28. Hantash BM, Bedi VP, Sudireddy V, Struck SK, Herron GS, Chan KF. Laser-induced transepidermal elimination of dermal content by fractional photothermolysis. J Biomed Opt. 2006;11:041115.
29. Goel A, Krupashankar DS, Aurangabadkar S, Nischal KC, Omprakash HM, Mysore V. Fractional lasers in dermatology–Current status and recommendations. Indian J Dermatol Venereol Leprol. 2011;77:369-79.
30. Al-Dhalimi MA, Arnoos AA. Subcision for treatment of rolling acne scars in Iraqi patients:A clinical study. J Cosm Dermatol. 2012;11:144-50.
31. Khan S, Ghafoor R, Kaleen S. Efficacy of saline injection therapy for atrophic acne scars. J Coll Physicians Surg Pak. 2020;30:359-63.
32. Cunliffe WJ, Gould DJ, Prevalence of facial acne vulgaris in late adolescence and in adults. Br Med J. 1979;1:1109-10.
33. Halvorsen JA, Stern RS, Dalgard F, Thoresen M, Bjertness E, Lien L. Suicidal ideation, mental health problems, and social impairment are increased in adolescents with acne:A population-based study. J Invest Dermatol. 2011;131:363-70.
34. Kleinerman R, Armstrong AW, Ibrahimi OA, King TH, Eisen DB. Electrobrasion vs. manual dermabrasion:A randomized, double-blind, comparative effectiveness trial. Br J Dermatol. 2014;171:124-9.
35. Anitha B. Prevention of complications in chemical peeling. J Cutan Aesthet Surg. 2010;3:186-8.
36. Sharquie KE, Noaimi AA, Radhi SK. Burn hemangioma (scalded pyogenic granuloma) versus infantile hemangioma:Report of six cases of burn hemangioma and its effective therapy with oral propranolol. J Cosm Dermatol Scien Applicat. 2017;7:229-44.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-0265-2040 http://orcid.org/0000-0002-0265-2040 http://orcid.org/0000-0001-5197-4786 http://orcid.org/0000-0001-5197-4786 |




Comments are closed.