Bleomycin-induced flagellate erythema in a patient with a germ cell tumor
Ganiou Adjade , Mohammed El Fadli, Leila Afani, Rhizlane Belbaraka
, Mohammed El Fadli, Leila Afani, Rhizlane Belbaraka
Department of Medical Oncology, CHU Mohammed VI, University Cady Ayyad, Marrakech, Morocco
Corresponding author: Dr. Ganiou Adjade
Submission: 23.01.2020; Acceptance: 29.03.2020
DOI: 10.7241/ourd.2020S3.6
Cite this article: Adjade G, El Fadli M, Afani L, Belbaraka R. Bleomycin-induced flagellate erythema in a patient with a germ cell tumor. Our Dermatol Online. 2020;11(Supp. 3):18-20.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Flagellated erythema is a rare skin toxicity specific to bleomycin caused by a low concentration of bleomycin hydrolase at the cutaneous level. Herein, we study a clinical case of flagellate erythema in a 37-year-old male followed for stageIIIA testicular seminoma of good prognosis. Eight days after administration of the first BEP chemotherapy treatment (bleomycin + etoposide + cisplatin), the patient presented a linear flagellate erythema on the trunk. The patient’s condition improved subsequently under symptomatic treatment.
Key words: Flagellated erythema; Skin toxicity; Bleomycin; Testicular Seminoma
INTRODUCTION
Bleomycin is an antitumor antibiotic derived from Streptomyces verticillus that, at low concentrations, produces a cytostatic effect by inhibiting mitosis and that, at high concentrations, blocks the incorporation of thymidine in the DNA. This way, the drug stops the S phase of the cell cycle and causes the cleavage of the DNA [1]. Discovered in Japan in 1966, it is generally used in combination with etoposide and cisplatin (the BEP protocol) for the treatment of germ cell tumors and lymphomas [2]. Bleomycin becomes inactivated in most tissues by the enzyme bleomycin hydrolase, which cleaves the ammonia group from the bleomycin. Its side effects are most often seen in the lungs and skin, due to the low concentration of bleomycin hydrolase, which leads to greater accumulation of the drug [3].
Herein, we study a clinical case of cutaneous erythematype toxicity secondary to the use of bleomycin.
CASE REPORT
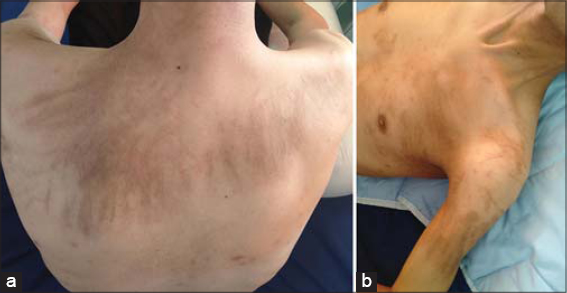
The following is a case of a 37-year-old male who consulted for an increased abdominal volume associated with constipation, pollakiuria, and a deterioration of the general state. On examination, the patient had a WHO performance status of 1 and a poorly defined hypogastric sensory mass. An abdominal CT scan revealed a large intraperitoneal hypogastric formation with right iliac and lateral aortic adenopathy. The tumor markers beta human chorionic gonadotropin (beta-hCG) and lactate dehydrogenase (LDH) were raised to 204 IU/mL and 714 U/L, respectively. Alphafetoprotein (AFP) was normal, at 1.05 ng/mL. The patient had an orchidectomy. A histological study revealed a malignant tumor proliferation infiltrating the conjunctivo-adipose tissue leading to a germinal tumor. Immunohistochemistry revealed a seminoma with the expression of PLAP+ (placental alkaline phosphatase) and CD117+. A postoperative assessment revealed the level of beta-HCG elevated to 12.7 IU/mL with other markers normal. A thoracoabdominopelvic CT scan revealed three pulmonary nodules and intraperitoneal lymphadenopathy of secondary appearance ranked stage IIIA (according to the updated 2009 AJCC classification) and of good prognosis (according to the International Germ Cell Cancer Collaborative Group classification). A multidisciplinary consultation meeting decided, then, to initiate BEPtype chemotherapy involving bleomycin (DT = 30 UI; J1, J8, J15), etoposide (100 mg/m2; J1 to J5), and cisplatin (20 mg/m2; J1 to J5) for testicular seminoma. After the administration of bleomycin, the patient reported persistent cutaneous pruritus of the thorax, limbs, and trunk with linear post-scratching lesions after the eighth day. An examination revealed flagellated erythema associated with linear hyperpigmentation of the thorax (predominant on the anterior surface of the left thorax and the posterior thoracic area), arms (predominantly proximal left), and nape with scratching lesions (Figs. 1a and b). The patient was placed on an oral corticoid and an antihistamine. The patient’s condition improved subsequently marked by a clear regression of the pruritus and erythema (Figs. 2a and b).
DISCUSSION
The main side effects of bleomycin are seen in the lungs and skin. This is explained by the absence of bleomycin hydrolase in these sites, an enzyme that rapidly inactivates bleomycin in most tissues [3].
Multiple skin toxicities have been reported: infiltrated purplish plaques, scleroderma lesions, erythema multiforme, and hyperkeratotic wart lesions of the knees and elbows. The specific skin toxicity of bleomycin is flagellated erythematous hyperpigmentation. Other rare skin manifestations, such as nail changes, alopecia, and stomatitis, have also been reported [4].
Flagellated erythema and linear pigmentation were first described by Moulin in 1970. This specific reaction to bleomycin occurs in approx. 8–20% of patients receiving treatment with bleomycin for lymphomas and germ cell tumors with doses between 15 mg and 285 mg in the cases reported [5].
In our patient, the lesions appeared after the administration of a dose of 60 mg. The average time between treatment and the onset of the rash varies from 12 to 24 hours to 6 months [6].
The diagnosis remains clinical. Lesions predominate in the trunk and proximal limbs [1]. The majority of patients initially develop generalized pruritus several hours to several weeks after the administration of bleomycin. Then, a linear erythematous streak appears, which eventually progresses to a typical flagellated hyperpigmentation [1]. This is the case of our patient, who initially showed persistent pruritus with a secondary appearance of a characteristic flagellated hyperpigmentation after scraping the week following the second injection of bleomycin. The lesions affected the neck, trunk, and arms. This is consistent with data from the literature.
There is no typical histopathological feature characterizing bleomycin-induced flagellated dermatitis. Lesions reported in the literature include melanophages in the skin capillaries, hyperkeratosis, parakeratosis, vesicular pustules, lymphohistiocytic dermal infiltrate, and sometimes lymphocytic vasculitis [1]. Occasionally reported on skin biopsy patches is inflammatory skin infiltration with a predominance of eosinophils. Thus, in the acute phase, one may observe vacuolization in the basal layers of the epidermis, melanin incontinence, and dyskeratotic keratinocytes dispersed. In the later stages, only a handful of postinflammatory changes are found [7].
The etiopathogenesis is uncertain. All the hypotheses are based on the histological or ultrastructural aspects found. Some authors have mentioned a traumatic mechanism by scratching due to intense pruritus or vasodilation responsible for an increase in the concentration of bleomycin in the skin. There follows a reduction in epidermal renewal, which causes prolonged contact between the melanocytes and the keratinocytes. However, studies have shown the clear appearance of linear streaks in the absence of direct trauma [7].
Regarding the treatment of flagellated erythema, opinions differ. On the one hand, it is reported that the erythema gradually improves six to eight months after stopping treatment. The characteristic residual hyperpigmentation may persist for several months [5]. On the other hand, an improvement in symptoms is observed after the application of topical corticosteroids or the use of systemic corticosteroids and an oral antihistamine. In addition, lesions may reappear with more intensity during a new treatment [8].
CONCLUSION
Flagellated erythema is a rare cutaneous toxicity related to the administration of bleomycin. The management of dermatitis is symptomatic with a good clinical evolution that may sometimes be marked by aesthetic sequelae.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Lahlou A, Gallouj S, Mernissi FZ. [Flagellate erythema as a bleomycin:specific adverse effect]. Pan Afr Med J. 2018;30:263.
2. Watson RA, De La Peña H, Tsakok MT, Joseph J, Stoneham S, Shamash J, et al. Development of a best-practice clinical guideline for the use of bleomycin in the treatment of germ cell tumours in the UK. Br J Cancer. 2018;219:1044–51.
3. Le A, Farmakiotis D, Reagan JL. Pruritic Rash in a Patient with Hodgkin’s Lymphoma. Cureus. 2018;10:e2450.
4. Verma SP, Subbiah A, Kolar Vishwanath V, Dutta TK. Bleomycin-induced skin toxicity:is it always flagellate erythema?. BMJ Case Rep. 2016;2016:bcr2014204575.
5. Cestari TF, Dantas LP, Boza JC. Hyperpigmentations acquises. Un Bras Dermatol. 2014;89:11-25.
6. Lu CC, Lu YY, Wang QR, Wu CH. Bleomycin-induced flagellate erythema. Balkan Med J. 2014;31:189-90.
7. Mota GD, Penna AM, Soares RC, Baiocchi OC. Bleomycin-induced flagellate dermatitis. Rev Bras Hematol Hemoter. 2014;36:297-9.
8. Verma SP, Subbiah A, Kolar Vishwanath V, Dutta TK. Toxicitécutanée induite par la bléomycine:est-ce toujours un érythème flagellé?. BMJ Case Rep. 2016;2016:bcr2014204575.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.