Knowledge, attitude, and behavior in the prescription of topical steroid for dermatological disorders among medical practitioners
1Department of Medicine, Government Medical College, Jammu and Kashmir, India, 2Department of Dermatology, Government Medical College, Rajouri, Jammu and Kashmir, India
Corresponding author: Dr. Rohini Sharama
Submission: 01.03.2020; Acceptance: 25.05.2020
DOI: 10.7241/ourd.20204.5
Cite this article: Abrol S, Sharma R. Knowledge, attitude, and behavior in the prescription of topical steroid for dermatological disorders among medical practitioners. Our Dermatol Online. 2020;11(4):357-359.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: The misuse and abuse of topical corticosteroids have increased manifold and the occurrence of adverse effects has, simultaneously, shown an upward trend. This has further been aggravated by the irrational prescribing behavior on the part of non-dermatologists.
Aim: This study aimed to evaluate the knowledge, attitude, and behavior of medical practitioners in prescribing topical corticosteroids.
Material and Methods: This was a cross-sectional, questionnaire-based study conducted at a tertiary center in northern India among 110 medical practitioners.
Results: All of the medical practitioners had been routinely prescribing topical corticosteroids without a clear indication, being completely unaware of possible side effects. This study revealed gaps in knowledge and unhealthy attitudes toward the ethical aspects of the rational use of steroids.
Conclusion: Our study revealed huge gaps in the knowledge and awareness about the potencies, side effects, and rational use of steroids. This further highlights the need to involve dermatologists in contributing and providing medical knowledge.
Key words: Knowledge, Medical practitioners, Topical steroids, Side effects
INTRODUCTION
Ever since the discovery of hydrocortisone, also known as Compound F, in 1952, topical corticosteroids have come a long way and established their indispensable role in the medical field. The armamentarium has expanded with the discoveries of novel drugs, ranging from low-potency to high-potency corticosteroids [1]. They are highly efficacious owing to their anti-inflammatory, immunosuppressive, and antiproliferative effects and have become the mainstay of therapy in a wide array of dermatological conditions [2]. However, various side effects and complications have emerged due to the rampant unethical use and abuse of topical corticosteroids. The various factors contributing to their misuse include the dearth of stringent laws regarding their sale, ignorance among patients, and even medical practitioners regarding their proper dosage, indications, and side effects, imprecise prescription, lack of coordination between dermatologists and other medical practitioners, and their difficult accessibility to dermatologists. The situation is further compounded by incorrect information provided by manufacturers. The repercussions can be seen in the form of various complications, such as the rising menace of resistant and recalcitrant dermatophyte infections, Topical Steroid Damaged/Dependent Face (TSDF), cutaneous atrophy, and hypertrichosis [3]. The following study was, thus, conducted to investigate the knowledge about and the attitude toward topical corticosteroid prescription by various specialists and medical practitioners for various dermatological disorders, as well as their behavior in patient counseling.
MATERIAL AND METHODS
This was a cross-sectional, questionnaire-based study conducted at a tertiary center in northern India among various medical practitioners to assess the knowledge, attitude, and steroid prescribing behavior of medical professionals in various dermatological disorders.
All medical graduates with an M.B.B.S degree, a postgraduate degree, or a diploma in various specialties were included in the study and a written informed consent was taken from each of them. A total of 110 participants were willing to participate in a survey in questionnaire form. The questionnaire was self-designed in view of lack of any such questionnaire available (Table 1). Following the distribution of the questionnaires and their completion, feedback was taken on whether the study helped in creating more awareness regarding the menace of topical corticosteroid abuse.
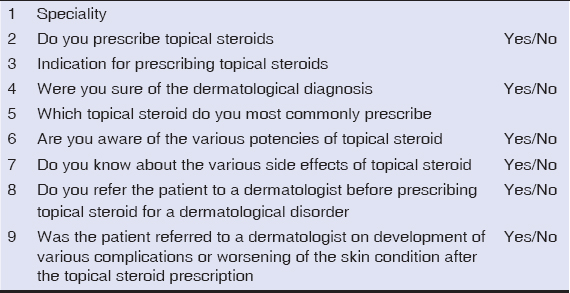 |
Table 1: Study questionnaire. |
Statistical analysis was performed using the software Epi Info. Wherever necessary, Fischer’s exact test was used to compare variables. A p value below 0.5 was interpreted as statistically significant.
RESULTS
A total of 110 medical professionals participated in the study, among which 64 (58.1%) were M.B.B.S graduates, and the other 46 (41.8%) were either postgraduates or diploma holders. Table 2 shows the distribution of their medical specialties. All of the participants had, in their practice, prescribed topical steroids to patients with various dermatological indications. Only 21 (19%) were most often sure about the dermatological diagnosis, whereas the other 89 (80.9%) were most often unsure. The most common indication for which 55 (50%) of the practitioners prescribed topical steroid was tinea, followed by general-purpose/fairness creams (37%/33.6%). Out of the 110 practitioners, 32 (29%) prescribed steroids even in an uncertain diagnosis. Various indications for topical steroid application are listed in Table 3. The most commonly used topical steroid was betamethasone, which was used by 32 (29%) of the medical practitioners in their routine practice, followed by mixed-combination creams used by 29 (26.3%); the rest is listed in Table 4. Only 27 (24.5%) were aware of the potencies of steroids. Out of the 110 medical practitioners, only 7 (6.3%) and 24 (21.8%) were aware of the various side effects of topical steroids. Unfortunately, only 11 (10%) referred a patient suffering from a dermatological disease to a dermatologist at the first visit, and a meager 27 (24.5%) did so following the absence of improvement of a skin disease, its worsening, or development of side effects.
 |
Table 2: Distribution of medical specialties. |
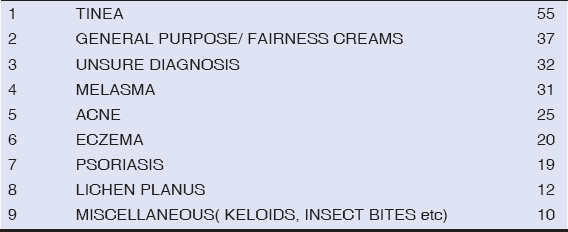 |
Table 3: Distribution of indications for the use of topical steroids. |
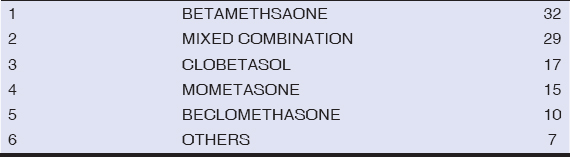 |
Table 4: Most commonly used steroids. |
DISCUSSION
Since their discovery, the use of topical steroids has revolutionized the treatment of various dermatoses, which can be attributed to their immediate relief from the various modes of action, such as immunosuppression, antiproliferation, antiangiogenic, and anti-inflammatory effects [4]. Over the years, they have become the epitome of treatment of all dermatological manifestations and the magic wand in the hands of practitioners [5].
However, the rapid onset and the immediate relief perceived by patients have led to their rampant misuse by patients and even non-dermatologists and practicing physicians, leading to a wide array of side effects, such as tinea incognito, erythema, and TSDF. The problem is further compounded by the dearth of stringent laws relating to their sale, and the easy availability of over-the-counter drugs for fairness and general cosmetic creams [6]. Some of the side effects are permanent and irreversible, having huge psychological morbidity upon the patients. The rising resistance of dermatophytes to antifungals is one such dreaded complication due to the inadvertent prescription of steroids by non-dermatologists reported by various studies [7].
Our study focused on medical practitioners and aimed to assess their knowledge and attitude toward steroid prescription, finding an alarming rate of topical steroid prescriptions by various medical practitioners. In 80.9% of these cases, prescriptions were made without a proper diagnosis. The most common indication was tinea treated with general-purpose creams. However, other studies reported acne as the most common indication [1,8]. Only 6.3% of the medical practitioners were aware of the side effects and a meager 10% referred their patient to a dermatologist for proper diagnosis. A study from Saudi Arabia drew similar conclusions, whereby the knowledge of topical steroid use in general practitioners was inadequate [9]. These findings have a greater significance in present-day scenarios. Similar alarming results were reported in another study [10].
Our study showed a clear lapse in the knowledge about topical steroids and the prescription behavior of medical practitioners, thus reaffirming the need to address this issue through a concerted and thorough approach. Similar findings have been reported by various other studies [11,12].
CONCLUSION
This survey clearly illustrates the knowledge gaps prevalent among various non-dermatologists and medical practitioners regarding the potency, usage, and side effects of topical steroids. This assumes great significance against the backdrop of the rising menace of antifungal resistant dermatophyte infections and TSDF. Thus, serious efforts at all levels are imperative to bridge these gaps, while advocating the correct and rational use of topical steroids by various medical practitioners needs to be encouraged.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Dey VK. Misuse of topical corticosteroids:A clinical study of adverse effects. Indian Dermatol Online J. 2014;5:436-40.
2. Becker DE. Basic and clinical pharmacology of glucocorticosteroids. Anesth Prog. 2013;60:25-31.
3. Meena S, Gupta LK, Khare AK, Balai M, Mittal A, Mehta S, et al. Topical corticosteroids abuse:A clinical study of cutaneous adverse effects. Ind J Dermatol. 2017;6:675.
4. Becker DE. Basic and clinical pharmacology of glucocorticosteroids. Anesth Prog. 2013;60:25-31.
5. Coondoo A. Topical corticosteroid misuse:The Indian scenario. Indian J Dermatol. 2014;59:451-5.
6. Lahiri K, Coondoo A. Topical steroid damaged/dependent face(tsdf):an entity of cutaneous pharmacodependence. Indian J Dermatol. 2016;61:265-72.
7. Gupta M. Topical corticosteroid abuse among pediatric population –a prospective study. Our Dermatol Online. 2020;11:194-6.
8. Makhija D, Shah H, Tiwari C, Dwiwedi P, Gandhi S. Outcome of topical steroid application in children with non-retractile prepuce. Dev Period Med. 2018;22:71-4.
9. Alsukait SF, Alshamlan NM, Alhalees ZZ, Alsuwaidan SN, Alajlan AM. Topical corticosteroids knowledge, attitudes, and practices of primary care physicians. Saudi Med J. 2017;38:662-5.
10. Verma P, Pathania S, Suvirya S, Shukla P. Knowledge attitude and practice survey in medical graduates regarding topical corticosteroids:A cross sectional study conducted at medical university of North India. Indian J Clin Exp Dermatol. 2019;5:133-6.
11. Song SY, Jung SY, Kim E. Steroid phobia among general users of topical steroids:a cross-sectional nationwide survey. J Dermatolog Treat. 2019;30:245-50.
12. Nagesh TS, Akhilesh A. Topical steroid awareness and abuse:a prospective study among dermatology outpatients. Ind J Dermatol. 2016;66:618.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.