Improvement of linear scleroderma of the limbs after treatment with long-pulsed 1064 nm Nd:YAG laser: A case report
César Bimbi1, Dimitra Koumoundourou2, Georgia Kyriakou 3, Piotr Brzezinski4
3, Piotr Brzezinski4
1Brazilian Society of Dermatology, Dermatologia–Laser Clinic Porto Alegre, 2Department of Pathology, University General Hospital of Patras, Greece, 3Department of Dermatology, University General Hospital of Patras, Greece, 4Department of Physiotherapy and Medical Emergency, Faculty of Health Sciences, Pomeranian Academy, Slupsk, Poland
Corresponding author: Georgia Kyriakou MD, MSc, cPhD
Submission: 27.12.2019; Acceptance: 27.04.2020
DOI: 10.7241/ourd.20204.11
Cite this article: Bimbi C, Koumoundourou D, Kyriakou G, Brzezinski P. Improvement of linear scleroderma of the limbs after treatment with long-pulsed 1064 nm Nd:YAG laser: A case report. Our Dermatol Online. 2020;11(4):376-378.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Linear scleroderma is a variant of localized scleroderma characterized by longitudinal bands of dense scleroatrophic skin sometimes causing deformities of the upper and lower extremities. Some case reports on small groups of patients suggest benefits of lasers in patients with localized scleroderma. We report a case of a twelve-year-old female with a two-year history of linear scleroderma on the right lower limb treated with 1064-nm long-pulsed Nd: YAG laser with successful results. Laser therapy may be a promising tool in the treatment of linear scleroderma.
Key words: Linear scleroderma Nd:YAG 1064 nm laser
INTRODUCTION
Linear scleroderma is a rare variant of localized scleroderma involving the superficial and deeper layers of the dermis usually beginning in childhood [1]. Fibrosis of the dermis and subcutaneous tissue leads to induration and shrinking of the skin. Depending on the extent of the lesions and the level of fibrosis, muscle and underlying bone may be affected and flexion contractures may occur. Changes in collagen tissue in these localized cases are very similar to cases of scleroderma but without visceral involvement.
No specific treatment is available for linear scleroderma.
CASE REPORT
A twelve-year-old female presented herself at our office with a two-year history of skin hardening on the right lower limb with pigmentary changes (Fig. 1). Complete blood count, the erythrocyte sedimentation rate, urinalysis, and liver and kidney function were normal. Antinuclear antibodies were negative. A physical examination revealed a firm diffuse sclerotic band with blotchy hyperpigmentation extending from the anterior aspect of the thigh to the lower part of the right leg.
 |
Figure 1: A wide, thick sclerotic band with blotchy hyperpigmentation extending from the anterior aspect of the thigh to the lower part of the right leg. |
A biopsy of the lesions showed a histological pattern of scleroderma with bundles of eosinophilic collagen throughout the reticular dermis and intimal thickening, narrowing, and obliteration of vessels (Fig. 2).
The patient and the patient’s relatives were informed of the self-limiting character of the disease, but all insisted on treatment, considering the disfiguring aspect of the disease. Still, no treatment protocol for linear scleroderma exists. Several topical treatments, such as corticosteroids and pimecrolimus, were unsuccessful, with the plaque continuing to increase in area and becoming increasingly hardened. Taking into consideration the patient’s young age, treatments based on methotrexate, systemic corticosteroids, and PUVA therapy were not recommended.
Sessions of 1064-nm YAG laser (Genesis) 14 J/cm2 with a 5-mm spot started with monthly intervals associated with pulsed light (LimeLight) 8–11 J/cm2, especially for hyperchromic parts (handpiece part of the Xeo Laser portable platform). Five laser sessions were performed (Table 1).
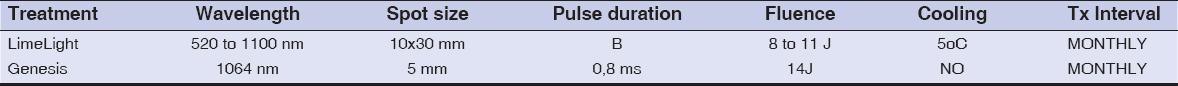 |
Table 1: Comparison of two treatment methods |
DISCUSSION
Although patients often receive good prognoses and spontaneous remission, linear morphea of the extremities may be accompanied by physical disability and limb length discrepancies when the underlying soft tissue and bone are involved. With the passage of time, the sclerotic bands may become thicker affecting the underlying tissues, specifically the fascia and musculature. In these cases, flexion contractures may occur resulting in the unaffected leg growing faster than the other. MRI of children with unilateral scleroderma sometimes shows fascia thickening and deep tissue abnormalities in the extremities [2]. Any change in the size of the limbs may be permanent.
Presently, there is still no single, reliable, and effective treatment protocol for linear scleroderma. Given that physiotherapy may be effective in limiting disease progression and prevent the appearance of contractures, the young patient was advised to engage in physical fitness activity [3,4].
Although the use of laser is not yet enshrined in linear sclerosis, it has already been demonstrated to be very effective in organizing collagen tissue in scars, being also an effective modality in the treatment of morphea [5,6]. 1064-nm long-pulsed Nd:YAG laser suppresses collagen production and flattens keloids, as demonstrated by Abergel on cultures of keloid fibroblasts [7].
We started sessions of 1064-nm Nd:YAG laser 15 J/cm2 with a 5-mm spot. After a total of five treatments with this technique, the patient showed a good improvement (Figs. 3 and 4). The treated skin became more pliable, while the plaques softened and restored their mobility nearly to that of normal skin. Pulsed light was immensely effective and was also used especially in the treatment of the hyperchromic parts. Pigmented cells are denatured and epidermal melanin first darkens and, after three days, tends to diminish.
The patient has been followed up now for two years since the procedure. In this report, we investigate the benefits of 1064-nm Nd:YAG laser (Genesis, Cutera Inc.) applied in a noncontact mode on linear scleroderma resulting in visible clinical improvement.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Figueiroa CM, Ricardo R. Localized scleroderma:clinical spectrum and therapeutic update. An Bras Dermatol. 2015;90:62-73.
2. Eric P. Eutsler, Daniel B. Horton, Monica Epelman Musculoskeletal MRI findings of juvenile localized scleroderma. Ped Radiol. 2017;47:442.
3. Jampani K, Nagaraja A, Peddireddy S, Kumar VS. Linear scleroderma:a series of all clinical variants. Our Dermatol Online. 2014;5:185-7.
4. Ruiz-Mejía O, Pimentel-Rangel J, Oribio-Gallegos JA, Valle de Lascuraín G, Esquivel-Vallejo A, Vega-España EA. [Orthopedic management of localized linear scleroderma in children:a case report]. Acta Ortop Mex. 2019;33:261-4.
5. Kineston D, Kwan JM, Uebelhoer NS, Shumaker PR. Use of a fractional ablative 10.6-μm carbon dioxide laser in the treatment of a morphea-related contracture. Arch Dermatol. 2011;147:1148.
6. Shalaby SM, Bosseila M, Fawzy MM, Abdel Halim DM, Sayed SS, Allam RS. Fractional carbon dioxide laser versus low-dose UVA-1 phototherapy for treatment of localized scleroderma:a clinical and immunohistochemical randomized controlled study. Lasers Med Sci. 2011;31:1707–15.
7. Abergel RP, Dwyer RM, Meeker CA, Uitto J, Lask G, Kelly AP. Laser treatment of keloids:A clinical trial and an in vitro study with Nd:YAG laser. Lasers Surg Med. 1984;4:291–5.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-6396-7767 http://orcid.org/0000-0002-6396-7767 http://orcid.org/0000-0001-6817-606X http://orcid.org/0000-0001-6817-606X |






Comments are closed.