A rare diagnosis of idiopathic eruptive macular pigmentation with dermoscopy. A case report
Aaqib Aslam, Yasmeen Jabeen Bhat , Insha Latif, Najam U Saqib, Iffat Hassan Shah
, Insha Latif, Najam U Saqib, Iffat Hassan Shah
Department of Dermatology, Government Medical College Srinagar, Jammu and Kashmir, India
Corresponding author: Dr. Yasmeen Jabeen Bhat
Submission: 23.02.2020; Acceptance: 26.04.2020
DOI: 10.7241/ourd.20203.6
Cite this article: Aslam A, Bhat YJ, Latif I, Saqib NU, Hassan Shah I. A rare diagnosis of idiopathic eruptive macular pigmentation with dermoscopy. A case report. Our Dermatol Online. 2020;11(3):252-254.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Idiopathic eruptive macular pigmentation (IEMP) is a rare disease of the paediatric age group characterised by hyperpigmented brownish to black macules; they are asymptomatic and involve mainly the trunk, back and extremities with no preceding inflammatory condition or any previous exposure to drugs. We report a case of a 7-year-old healthy boy with brown to black asymptomatic macules on the back and chest. The lesions persisted for only a few months. The changes were discrete with individual lesions ranging from 1-2 cm. Histology showed prominence of the pigment layer with increase in the dermal collagen and sparse lymphocytic inflammation of the dermis.
Key words: Macules, Eruptive, Hyperpigmentation, Asymptomatic
INTRODUCTION
Idiopathic eruptive macular pigmentation (IEMP) is a rare condition with only a few cases published so far. It is characterised by the presence of pigmented asymptomatic macules which mainly involve the trunk, face and extremities and are usually found in the paediatric age group. These macules gradually resolve spontaneously over time and may take months to years for resolution. IN 1978 Degos et al. provided the first description of this condition. It was further described in English by Sanz De Galdeano in 1996 [1]. This laid the criteria for the diagnosis of the condition, with the following points:
- Eruption of brownish black, discrete, non-confluent, asymptomatic macules involving the neck, trunk and extremities in children and adolescents.
- Absence of any preceding lesions.
- No previous drug exposure.
- Epidermal hyperpigmentation of the basal layer with dermal melanophages without any basal cell damage
- Normal mast cell count.
In this report, we have a 7-year-old boy fulfilling the criteria for this condition.
CASE REPORT
We report a 7-year-old male patient who reported to the outpatient department of dermatology due to multiple hyperpigmented lesions on the back and chest (Fig. 1). There was gradual increase in size and number of these hyperpigmented macules. There was no history of any drug intake in this patient. On examination multiple asymmetrical hyperpigmented brown to black macules on the back and chest were observed. The size ranged from pin-point to 1-2 cm in diameter. These macules were asymptomatic with no preceding skin lesions. There was no history of itching and there was absence of scaling as well. Some lesions had a velvety surface. The patient also had multiple patches of hair loss on the scalp ranging 1-4 cm in diameter. The patient was in good health and no comorbidity was seen.
 |
Figure 1: Multiple asymmetrical hyperpigmented brown to black macules on the back of a 7-yeard-old male |
The patient was further investigated using dermatoscopy which revealed brown to black pigmented granules and dots scattered across an accentuated pigment network (Fig. 2).
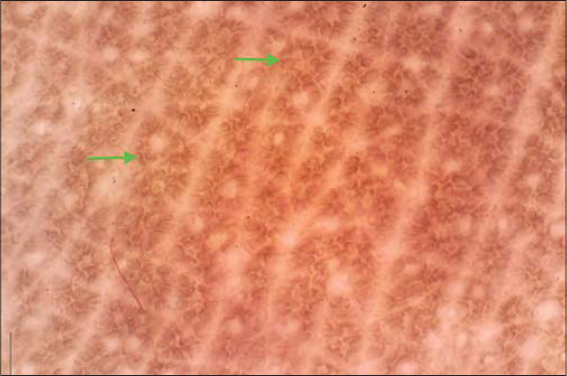 |
Figure 2: Brown to black pigmented granules and dots were seen scattered across an accentuated pigment network (green arrows) on dermoscopy (DL4, polarised). |
Trichoscopy of the scalp demonstrated the presence of black dots, cadaver hairs, an occasional exclamation point hair and a clinical diagnose of alopecia areata was made.
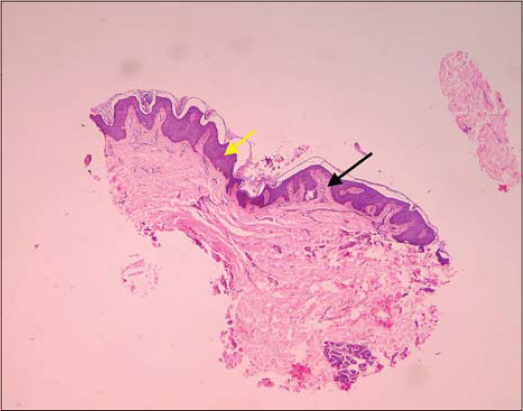
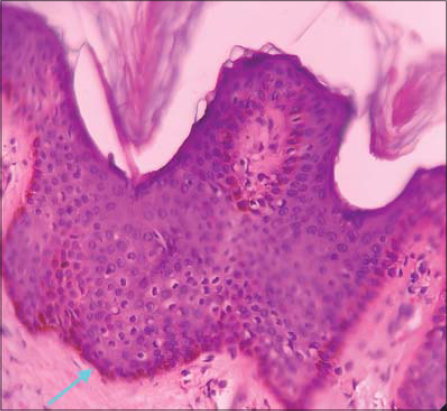
The patient was further evaluated with a skin biopsy which was taken from the back. Histological description showed epidermis with a prominent pigment layer due to basal cell hyperpigmentation. Moderate acanthosis could also be seen (Fig. 3). The underlying dermis showed insignificant inflammation with sparse lymphocytic infiltrate. There was also an increase in dermal collagen (Fig. 4).
Normal mast cell count was seen in this patient, further fulfilling the said criteria for this condition.
The patient was first treated with topical steroids on the back and chest with no response and was later sent for observation without any topical or systemic treatment and assurance. Spontaneous resolution began 3 months after stoppage of any topical medication.
Alopecia areata was treated with topical application of steroids and tacrolimus with a positive response.
DISCUSSION
Idiopathic eruptive macular pigmentation (IEMP), a rare disease of children and adolescents is a benign self-limiting condition where remission may take from months to years. Differential diagnosis of the condition includes lichen planus pigmentosus, erythema dyschromicum perstans and urticaria pigmentosa. On biopsy, IEMP could be differentiated from the other conditions. Lichen planus pigmentosus and erythema dyschromicum perstans show basal cell vacuolization with individually necrotic keratinocytes at the dermoepidermal junction with melanophages scattered in papillary dermis. Urticaria pigmentosum gives a positive Darier’s sign which is negative in IEMP. The condition has been underreported probably due to reluctance to perform biopsy in children and because of smaller awareness of the condition among the treating physicians. The pathogenesis of IEMP is unknown; however, hormonal factors may play a role as the condition is mainly present in the peripubertal age group. There has been a case report of this condition in a patient as young as 1 year old while a case of a 50-year-old has also been reported [2,3]. Most of the reported cases involve young patients. As already mentioned, the criteria for the diagnosis of this condition have been laid down by Sanz De Galdeano [1]. Our case fulfilled the above-mentioned criteria. It must also be mentioned that only a handful of cases of similar nature have been reported [4–6] among the Indian population. The indent of this case report is to create awareness about this condition among treating physicians of all specialties to avoid misdiagnosis and unnecessary management of this self-limiting condition.
Consent
Examination of the patient was conducted according to the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
1. Kumarasinghe SPW, Pandya A, Chandran V, Rodrigues M, Dlova NC, Kang HY, et al. A global consensus statement on ashy dermatosis, erythema dyschromicum perstans, lichen planus pigmentosus, idiopathic eruptive macular pigmentation, and Riehl’s melanosis. Int J Dermatol. 2019;58:263-72.
2. Jang KA, Choi JH, Sung KS, Moon KC, Koh JK. Idiopathic eruptive macular pigmentation:Report of 10 cases. J Am Acad Dermatol. 2001;44:351-3.
3. Mantovani L, Minghetti S, Ricci M, Zauli S, Marzola A, Corazza M. Idiopathic eruptive macular pigmentation in a 50-year-old man. Eur J Dermatol. 2010;20:633-4.
4. Vasani RJ. Idiopathic eruptive macular pigmentation – Uncommon presentation of an uncommon condition. Indian J Dermatol. 2018;63:409-11.
5. Ghiasi M, Kamyab K. Idiopathic eruptive macular pigmentation with papillomatosis. Clin Exp Dermatol. 2017;42:94-5.
6. Grabell D, Milgraum D, Naganathan S, Milgraum S. Idiopathic eruptive macular pigmentation with papillomatosis. Cutis. 2018;101:E4-E5.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.