Anaplastic transformation in a classic Kaposi’s sarcoma
Sara Mai 1, Siham Mansouri1, Mustapha Outznit2, Kaoutar Znati3, Karima Senouci1, Meriem Meziane1
1, Siham Mansouri1, Mustapha Outznit2, Kaoutar Znati3, Karima Senouci1, Meriem Meziane1
1Department of Dermatology, University Hospital Ibn Sina, Rabat, Morocco; 2Department of Radiology, Ibn Sina University Hospital, Rabat, Morocco; 3Department of Histopathology, Ibn Sina University Hospital, Rabat, Morocco
Corresponding author: Dr. Sara Mai
Submission: 18.09.2019; Acceptance: 23.11.2019
DOI: 10.7241/ourd.20203.29
Cite this article: Mai S, Mansouri S, Outznit M, Znati K, Senouci K, Meziane M. Anaplastic transformation in a classic Kaposi’s sarcoma. Our Dermatol Online. 2020;11(3):329-330.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
A classic Kaposi’s sarcoma (KS) is a low-grade vascular tumor with a benign course that affects mostly the skin and oral mucosa. Uncommonly, KS can have a more aggressive evolution leading to local deep invasion and systemic involvement. This particular form is called anaplastic KS. We report a case of an anaplastic transformation in a classic KS in an immunocompetent patient.
A 50-year-old man presented with a large, painful tumefaction of the left foot evolving for over 6 years and resulting in a complete deformation of the forefoot and toes and painful ulcerations. Physical examination revealed an enlarged left foot with multiple violaceous nodules resulting in a massive enlargement and deformation of the whole foot and destruction of the toes. The patient also presented multiple painful ulcerations with permanent serous exudate (Figs. 1a and 1b). The rest of the examination revealed ipsilateral inguinal lymphadenopathies.
 |
Figure 1: (a and b) An enlargement and deformation of the left foot with multiple confluent violaceous nodules and ulcerations. |
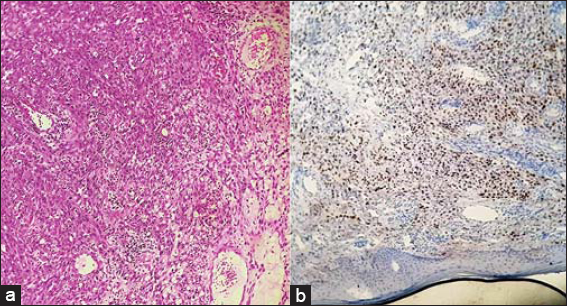
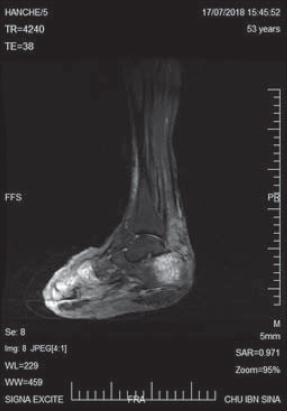
A skin biopsy of a nodular lesion was performed. Histological examination revealed a dermal proliferation of spindle cells exhibiting moderate to marked cytonuclear atypia with a high mitotic rate. Immunohistochemical staining for HHV8 was positive, confirming the diagnosis of Kaposi’s sarcoma (Fig. 2). An HIV test was negative. An MRI of the affected foot showed deep infiltration and massive bone destruction (Fig. 3). A CT scan revealed micronodules in the lungs, a hypodense lesion in the liver, and lomboaortic and pelvic lymphadenopathies. The patient had been on liposomal doxorubicin for 6 months, which resulted in a reduction in the size of the foot, a complete healing of the ulcerations, and a decrease in the size and number of the nodules.
Kaposi’s sarcoma (KS) was first described in 1872 by Moritz Kaposi as an «idiopathic, multipigmented sarcoma of the skin » [1]. Four epidemiologic variants of KS are known: classic, endemic (African), iatrogenic, and AIDS-associated.
First described in 1959 by Cox and Helwig, a malignant transformation of Kaposi’s sarcoma (KS) is characterized by an increase in the number of mitotic figures and marked cellular pleomorphism [2]. Since then, anaplastic transformations have more frequently been observed in African KSs, and rarely in classic KSs.
Clinically, anaplastic KS is characterized by its high local aggressiveness and invasive capacity, along with its metastatic potential. It generally presents itself as rapidly growing nodules or tumors with ulcerations usually associated with lymphedema [3].
Less frequent manifestations include subcutaneous tumors and exophytic lesions. Deep tissue invasion is usually observed, sometimes with bone infiltration. However, none of these clinical aspects is specific to anaplastic KS [3,4].
Histopathologically, anaplastic KS is characterized by a dense proliferation of endothelial, epithelioid, and spindle cells with a significantly greater degree of nuclear and cellular pleomorphism, an increased mitotic index (5–20 mitoses per 10 high-power fields), and atypical mitoses. Necrosis is occasionally observed [5]. Identification of HHV8 by immunohistochemistry is important to the distinction between anaplastic KS and other malignant vascular tumors, especially angiosarcoma.
The causes of an anaplastic transformation of KS are unclear, and different potential inducers, such as a long course of the disease, lymphedema, chemotherapy, and immunological defects in AIDS-related KS, have been proposed [3,4].
Given the extreme rarity of this clinical form, there is no consensual treatment regimen. Paclitaxel and liposomal doxorubicin seem to be the most effective chemotherapeutical agents according to some authors. Others suggest that a more aggressive approach involving nonconservative surgical treatment with systemic chemotherapy is the most appropriate for the treatment of anaplastic KS [4].
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients have given consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Kaposi M. Idiopathisches multiples Pigmentsarkom der Haut. Arch f Dermatol u Syph. 1872;3:265–73.
2. Cox FH, Helwig EB. Kaposi’s sarcoma. Cancer. 1959;12:289-98.
3. Sanjay N. Agrawal, Anuprita A. Rawal, Subodhkumar D. Jane. Classic Kaposi’s sarcoma:a rare case with unusual presentation. Our Dermatol Online. 2014;5:68-70.
4. Tourlaki A, Recalcati S, Boneschi V, Gaiani F, Colombo A, Mancuso R, et al. Anaplastic Kaposi’s sarcoma:a study of eight patients. Eur J Dermatol. 2013;23:382-6.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-7584-8442 http://orcid.org/0000-0001-7584-8442 http://orcid.org/0000-0002-5140-7607 http://orcid.org/0000-0002-5140-7607 |



Comments are closed.