A new variant of endemic pemphigus foliaceus in Colombia South America
Ana Maria Abreu Velez 1, Yulieth Alexandra Upegui-Zapata2, Carlos Andres Valencia-Yepes3, Eduardo Upegui-Quiceño4, Hong Yi5, Adriana Vargas Florez6, Takashi Hashimoto7, Michael S. Howard1
1, Yulieth Alexandra Upegui-Zapata2, Carlos Andres Valencia-Yepes3, Eduardo Upegui-Quiceño4, Hong Yi5, Adriana Vargas Florez6, Takashi Hashimoto7, Michael S. Howard1
1Georgia Dermatopathology Associates, Atlanta, Georgia, USA; 2PECET, Medical Research Institute, School of Medicine, University of Antioquia, Medellin, Colombia, South America; 3Undergraduate student, Department of Education, University of Antioquia, Medellin, Colombia, South America; 4PECET Programa de Estudio y Control de Enfermedades Tropicales, Medical Research Institute, School of Medicine, University of Antioquia, Medellin, Colombia, South America; 5Robert P. Apkarian Integrated Electron Microscopy Core, Emory University Medical Center, Atlanta, GA, USA; 6Hospital Universitario Fundación Santa Fe de Bogotá, Bogotá, Colombia, South America; 7Department of Dermatology, Osaka City University Graduate School of Medicine, Osaka, Japan
Corresponding author: Ana Maria Abreu Velez, M.D., Ph.D.
Submission: 10.07.2020; Acceptance: 20.07.2020
DOI: 10.7241/ourd.20203.14
Cite this article: Abreu Velez AM, Upegui-Zapata YA, Valencia-Yepes CA, Upegui-Quiceño E, Yi H, Vargas Florez A, Hashimoto T, Howard MS. A new variant of endemic ipemphigus foliaceus in Colombia South America. Our Dermatol Online. 2020;11(3):284-299.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
A new variant of endemic pemphigus foliaceus in El Bagre and surrounding municipalities (El Bagre-EPF), also titled pemphigus Abreu-Manu, is a complex disease that has a genetic component and likely environmental triggering factors. The disease is present only in certain high-prevalence areas and affected individuals present in a unique cluster, that represent opportunities to study interactions of the environment and genetics with the immune system. The primary autoantibodies are directed to known cell junctions, but also directed to recently discovered ones that are formed via amalgamation of classic cell junctions. Besides desmoglein 1, main autoantigens are members of the p120 and plakin families, myocardial zonula adherens protein, and the armadillo repeat gene deleted in velo-cardio-facial syndrome. Other autoantibodies are directed to cell junctions in neurovascular bundles and neural receptors. A possible genetic founder effect in Indians may predispose individuals to this disease. El Bagre-EPF prevails in males after their forties and occasionally affects peri-postmenopausal females. Ultraviolet radiation is a main exacerbating factor of the disease, and seborrheic areas are most frequently affected. One third of the patients have a mild form of the disease with minimal clinical findings; one third of the patients show moderate clinical features with alterations in the skin and other organs, and one third of the patients show multiorgan systemic abnormalities, which are manifested clinically, histopathologically and immunologically. Mining, deforestation, environmental pollution and alterations in the ecosystem may partially trigger El Bagre-EPF.
Key words: Endemic pemphigus foliaceus in El Bagre (El Bagre-EPF), Autoimmune blistering diseases, Cell junctions
Abbreviations: Endemic pemphigus foliaceus (EPF), endemic pemphigus foliaceus in El Bagre, Colombia (El Bagre-EPF), fogo selvagem (FS), pemphigus foliaceus (PF), hematoxylin and eosin (H&E), direct immunofluorescence (DIF), indirect immunofluorescence (IIF), immunohistochemistry (IHC), confocal microscopy (CFM), basement membrane zone (BMZ), intercellular staining between keratinocytes (ICS), desmoglein 1 (Dsg1), myocardial zonula adherens protein (MYZAP), fluorescein isothiocyanate (FITC), kilodaltons (kDa), immunoblotting (IB), immunoprecipitation (IP), indirect immune electron microscope (IEM), complex segregation analysis (CSA), armadillo repeat gene deleted in velo-cardio-facial syndrome (ARVCF), bullous pemphigoid antigen I (BP230), desmoplakins I-II (DP I-II)
INTRODUCTION
One disease that belongs to the autoimmune blistering diseases group [1] is endemic pemphigus foliaceus (EPF), that afflicts rural populations in tropical low-income countries, with high-prevalence areas; affected individuals present in a unique cluster. He disease provides opportunities to study interactions of the environment and genetics with the immune system [2,3]. EPF is found in relatively well-defined regions of South and Central America and Africa [4–6].
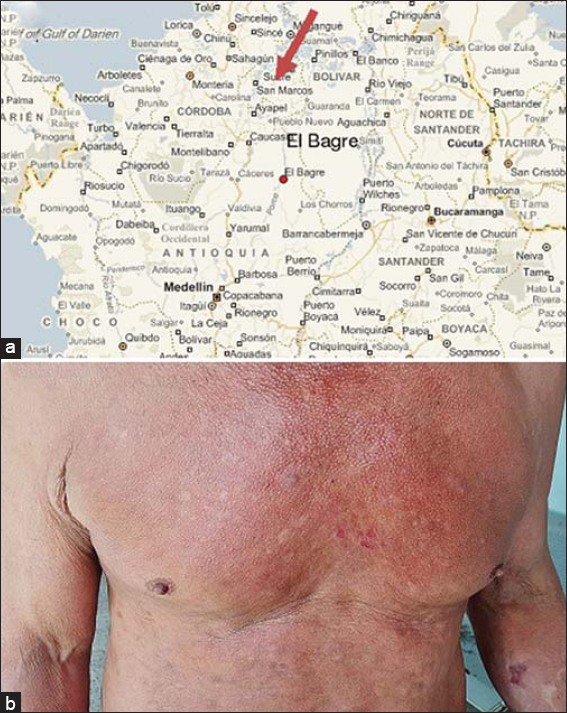
A retrospective study performed at the Hospital Universitario San Vicente de Paul in Medellin, Antioquia State, Colombia South America reported that between 1982 and 1986 21 patients were diagnosed with pemphigus foliaceus (PF) similar to the ‘fogo selvagem’ (FS) type [7]. The patients came from El Bagre and Nechi, rural towns in Colombia (See map upper panel, Figure 1), which were known for gold mining. The authors reported this disease as the first outbreak of South American pemphigus foliaceus (PF) reported in Colombia. The majority of the patients were mestizo men, who worked as farmers, miners or both [7]. These authors never visited the endemic area, and some of the data was retrospectively collected from the hospital files.
One of our authors has visited the endemic area since 1991 and was able to confirm that this disease was indeed a new variant of EPF in El Bagre (El Bagre-EPF). For the discovery of this new disease, we also named it pemphigus Abreu-Manu following the names of the author who discovered the disease and her daughter [8–38]. Patients affected by El Bagre-EPF live in an area rich in gold ore, and environmentally polluted with mercury. The endemic region of El Bagre-EPF is also rich in metals and metalloids [8–38]. Because of illegal mining of gold and the cocaine trade, the endemic area had suffered from ferocity, power struggles and significant fighting among the armed forces, the guerillas, paramilitary and common delinquents for over 50 years. The conditions has made our work difficult at times, but we have been respected by the polarizing groups for our humanitarian help to the patients, their families and the community.
Based on the fact that this malady highly differs from other types of pemphigus or EPF in clinical and epidemiological aspects, we further characterized this new variant of EPF as mentioned above [8–38]. EPF is characterized by the deposition of autoantibodies mainly directed to the ectodomain of desmoglein 1 (Dsg1) [2–8].
The lesions are usually blisters that easily denuded and show typical acantholysis on hematoxylin and eosin (H&E) staining [2–8]. The patient sera immunoprecipitates a 45 kDa ectodomain of Dsg1 and shows intercellular epidermal deposits of IgG4 mostly directed to the stratum granulosum of the epidermis using direct immunofluorescence (DIF) [2–8].
In 1991, we created a humanitarian volunteer program populated by medical researchers and volunteers to help the community and the patients affected by the new variant of EPF in El Bagre, Colombia [8–38]. Since then, we have had the opportunity to study a large cohort of the patients affected with this disease longitudinally for 30 years [8–38]. From the original 8 patients, we have found many other patients, many of whom had died due to complications of the disease and their precarious conditions. We found four to five new patients affected by this disease annually [8–38].
Investment in research in this disease has been extremely limited; unlike in the USA, the public health agenda for developing countries is not well funded. In addition, in some cases, the funds need to be associated with universities and are not given to the lead authors. The mechanisms and pathogenesis of El Bagre-EPF thus remain largely unknown, which precludes the development of effective prevention and therapeutic strategies. The pathogenesis might combine genetic and environmental factors, which would explain the distribution of the disease in specific geographic hot spots [8,9]. Untreated El Bagre-EPF conveys a very poor prognosis. However, the small local hospital does not have radiology equipment, and, when we visited the endemic areas, we had to carry a portable echocardiogram. The only tests available in the local hospital are studies for malaria and some basic chemical tests, as well as complete blood count (CBC) when the proper reagents are rarely available.
With our work, we demonstrated that in about one third of the patients showed a systemic morbidity not only in the skin but also in other organs. We also demonstrated the presence of autoantibodies against multiple organs using multiple immunologic techniques and case-controlled studies [15–17,20,21].
El Bagre-EPF differs from previously described forms of EPF in several aspects. In addition, this disease shares features with paraneoplastic pemphigus in terms of heterogeneous immunoreactivity, although it is not associated with malignant tumors. El Bagre-EPF clinically simulates Senear-Usher syndrome (pemphigus erythematosus) but occurs endemically.
El Bagre-EPF occurs either as a localized form with stable clinical course, or as a systemic form [15–17,20,21]. Our work has shown that the latter systemic form seems to affect organs and show the presence of autoantibodies to the molecules of the plakin family, which include desmoplakins I, II (DP I, II), periplakin, envoplakin, the 230 kilodaltons (kDa) bullous pemphigoid antigen 1 (BP230) and others to be determined [6–8], including Dsg1. Many of these plakin family molecules are located in most organs and are involved in both inherited and autoimmune diseases that affect the skin, neuronal tissue, and cardiac and skeletal muscle. The plakin family proteins, which are known as cyto-linkers, play a crucial role in orchestrating cellular development and maintaining tissue integrity.
Patients recruited to our comprehensive studies, fulfilled the following diagnostic criteria for El Bagre-EPF: (i) the patient presented the clinical and epidemiological features described for this disease [8–10]; (ii) they lived in the endemic area [8–10]; (iii) their sera displayed staining to epidermal keratinocyte cell surfaces and to the cutaneous basement membrane zone (BMZ) by DIF using fluorescein isothiocyanate (FITC)-conjugated monoclonal antibodies to human total IgG or to IgG4, as previously described [8–10]; (iv) their sera were positive for reactivity against Dsg1 and plakin molecules, confirmed by IB performed as previously described [9–11], (v) their sera immunoprecipitated a Concanavalin A affinity-purified bovine tryptic 45 kDa fragment of Dsg1 [9–11]; and (vi) the patient sera yielded a positive result using an ELISA when screening for autoantibodies to PF antigens [12].
All our studies were approved by a human quality assurance review board at the Hospital Nuestra Señora del Carmen in El Bagre. All participants signed informed consent forms, and we conducted multiple case control matched studies comparing El Bagre-EPF patients and healthy controls from the endemic area, matched by age, gender, demographics (including history of malaria, gastrointestinal infections or sexually transmitted diseases, dengue, tuberculosis; cohabitation with domestic animals; exposure to wild animals, living and working activities, distance to rivers; tobacco, marijuana or liquor habits; exposure to agricultural and jungle vegetation; exposure to rodents, mosquitoes, and snakes and other jungle animals during rest or work hours; basic diet, and employment activities). In all our studies we evaluated the cases and controls clinically, and biopsy samples were assessed by hematoxylin and eosin (H&E) staining, by DIF, immunohistochemistry (IHC), confocal microscopy (CFM), ELISA, IB and immunoprecipitation (IP), and indirect inmunoelectron microscopy (IEM), as previously described [8–15]. For DIF, biopsies were taken from perilesional skin on the chest, and control biopsies were also obtained from normal skin on the chest. Indirect immunofluorescence (IIF) used the skin samples obtained from cadaver donors with a proper institutional review board permit.
Epidemiological and Phenotypic Expression
Our work revealed that El Bagre-EPF is endemic in rural areas surrounding El Bagre and surrounding municipalities [8–11]. The disease appeared in 4.7% of middle-aged and older men and postmenopausal women from these rural areas. The long-term outcome from medical charts for the patients in advanced stages is very poor, with 75% mortality at 2 years [8–11]. The phenotypic expression is variable due to the stages at which the patients were diagnosed. Treatment usually requires systemic corticosteroids, which were administrated according to the patient’s weight. Clinically, the disease can manifest with several clinical forms, ranging from a fruste form, pigmentary form, ichthyosis-like form, and generalized form [8–17]. In general, the nature of this disease is chronic, the patients may present episodic relapses, and generalized form exhibits poor prognosis in comparison with the localized form [8–17]. The implementation of a program design only with local treatment decreased the morbidity and mortality significantly at the hospitals in the endemic areas.
Clinical Forms, Relapses, and Cure
El Bagre-EPF differs from previously described forms of EPF. El Bagre-EPF is a chronic inflammatory disease that has unique manifestations, including a fruste form (localized to the skin and resembling Senear-Usher syndrome (see Figure 1 lower panel), a combination of pemphigus and lupus erythematosus with photosensitivity). El Bagre-EPF also presents with relapsing episodes. Both a chronic form and a systemic form exist, and the latter affects multiple organs with a less favorable prognosis [5,6,12–19]. The disease prevalence is 4.7% of middle-aged and older men and postmenopausal women. The endemic focus has not changed during the 30 years we have been visiting the geographic area [8–10]. At this point in our understanding of El Bagre-EPF, we are uncertain why some patients present a stable localized form in the skin, and others present a systemic form with relapses [8–10]. In addition, a few patients may enter clinical remission for years.
Histopathology
Histopathological examination of El Bagre-EPF patient’s specimens following H&E staining establishes several patterns depending on the clinical form and the severity of the disease. By H&E, the blisters at the subcorneal epidermis are most commonly observed, although intra-spinous and subepidermal blisters were seen in some cases. Our results presented very diverse histopathologic patterns in non-glabrous skin, which seemed to associate with the clinical features [14]. The most common pattern was typical PF-like pattern, with some lupus erythematosus-like features. A non-specific, chronic dermatitis pattern prevailed in the clinically controlled patients taking daily corticosteroids. In the patients who had the most severe and relapsing disease, early sclerodermatous changes prevailed in their reticular dermis. In addition to the sclerodermoid changes, the reticular dermis showed a paucity of appendageal structures. The skin biopsies of the palms displayed a similar pattern in all cases, including thickening of the stratum corneum, hypergranulosis, edema in the papillary and reticular dermis and a dermal perivascular lymphocytic infiltrate [14].
Importance of the Autoantibodies
Human autoantibodies in autoimmune diseases of the skin and other organs have been instrumental in the identification of important new cell junction molecules and their function in physiologic conditions.
AUTOANTIGENS
Ectodomain of Dsg1
We obtained additional information about this disease by focusing on the characterization of some autoantigen profiles, using a case-control study with sera samples obtained from patients and the controls from the endemic area [10,11]. We were able to resolve the identity of the most significant antigenic moiety, a 45 kDa tryptic fragment which is recognized by all sera from patients with FS, PF and El Bagre-EPF patients, as well as half of PV sera [8–11]. We documented a conformational epitope on the 45 kDa peptide obtained by trypsin digestion of viable bovine epidermis, and glycosylated peptides were partially purified on a concanavalin A (Con-A) affinity column. This column fraction was then used as an antigen source for additional immunoaffinity purification [11]. A PF patient’s serum covalently coupled to a Staphylococcus aureus protein A column was incubated with the Con-A eluted products and the immuno-isolated antigen was separated by SDS-PAGE, transferred to a membrane, and visualized with Coomassie blue, silver and amido black stains. The 45 kDa band was subjected to amino acid sequence analysis revealing the sequence, EXIKFAAAXREGED, which matched the mature form of the extracellular domain of bovine Dsg1. Our discovery established the biological importance of the ectodomain of Dsg1, as well as the relevance of conformational epitopes in various types of pemphigus [11].
Other Autoantigens
We compared the El Bagre-EPF and the Brazilian-EPF FS by means of IB and baculovirus expression systems. By IB using normal human epidermal extracts, 38% of El Bagre-EPF sera and 25% Brazilian EPF sera showed IgG antibodies reactive to Dsg1. The sera of both types of EPF also showed protein bands co-migrating with plakin family proteins, particularly periplakin [15–21]. IB analyses also showed positive reactivity of El Bagre-EPF sera with recombinant proteins of various domains of envoplakin, periplakin and bullous pemphigoid antigen I (BP230) [8–10]. These finding indicate that a considerable number of El Bagre-EPF sera reacted with recombinant proteins of periplakin, while only few FS sera reacted with some of the recombinant proteins of any plakins. Enzyme-linked immunosorbent assays (ELISAs) for Dsg1 and Dsg3 showed that Dsg1 was reacted by almost all sera of both types of EPF [8–10]. However, unexpectedly, while none of El Bagre-EPF sera reacted with Dsg3, about half of FS sera reacted with Dsg3. Thus, we conclude that the El Bagre-EPF is basically similar to FS in that the major antigen is Dsg1, but there are significantly different antigen profiles between these two types of EPF [8–10].
We continued the characterization of other El Bagre-EPF antigens and found p0071, armadillo repeat gene deleted in velo-cardio-facial syndrome (ARVCF), plus BP230, periplakin, envoplakin, DP I-II (the 5 plakin family proteins) and myocardial zonula adherens protein, (MYZAP) as possible autoantigens. Other antigens need to further determined. Of interest, these molecules are present not only in the desmosomes but also in other multiple cell-junctions, including gap, tight and adherens junctions, as well as BMZs in several different tissues. Our discoveries present a molecular penetrance paradigm, because most of these molecules are ubiquitously present in the majority of organs [15–20].
Based on these findings, we had been continuously describing several systemic anomalies in the patients affected by El-Bagre-EPF, including alterations in their eyes, sudden death syndrome, kidney problems and others systemic anomalies. Indeed, before the steroid era, the systemic mortality associated with this disease was huge and the patient necropsies showed multiple anomalies [15–20]. We also focused on characterizing other antigens for protein bands, which were seen in the IB studies using different techniques, including radio-immune assay (RIA), enhanced chemiluminescence (ECL) and IP as well as sequential solubilization techniques, using several antigen sources (e.g.: human skin, MCF-12 mammary epithelial cell line (ATCC), cow snouts, rat, mice, veal, and other animal and human antigen sources [15–21].
Autoantibodies in the El Bagre-EPF Relatives
Susceptible individuals living in geographically defined rural areas develop the disease. In addition, their genetic relatives have increased levels of autoantibodies to EPF antigens, compared with controls from the endemic area. In the patient’s relatives, these autoantibodies do not seem to be pathogenic [8,9]. Upon leaving the endemic area, patients exhibit a milder clinical outcome or possibly a “clinical cure”. However, in most cases the autoantibodies are still detected in their sera [8,9].
Development of a Novel ELISA
We also established a cost-effective ELISA capable of distinguishing the heterogeneous antibody population observed in these El Bagre-EPF patients to confirm patients for epidemiological studies. We used the protein extract obtained from trypsin-digested fresh bovine cow snouts and further purified on a Concanavalin A (Con A) matrix as an antigen [13]. The inclusive sensitivity and specificity of the assay were resolute to be 95% and 72%, respectively, with reproducibility’s of 98% (intra-assay) and 95% (inter-assay), permitting testing of multiple serum samples; the assay correlated well with the clinical activity and extent of disease in patients with El Bagre EPF [13].
Cutaneous Test
Atopy is a common cause of an increase in serum IgE levels. We tested for a cutaneous response to different allergens by injecting allergen samples of Dermatophagoides (D. pteronyssinus and D. farinae). Approximately 20 to 30 ul of these agents (Abello ALK, Madrid) at a concentration of one biologic unit were applied intradermally (1 UI/ml I.D.) in the lateral area of the arm, using an insulin syringe. Positive (histamine chlorhydrate 1:10,000) and negative (saline solution) controls were also used. A positive result was indicated by erythema with a diameter of greater than 5 mm and/or edema. Only one El Bagre-EPF patient was positive for IgE for D. pteronyssinus and D. farinae, although no statistically significant difference was detected [8,9].
DIF and IIF
DIF for skin biopsies taken from the glabrous and the non-glabrous skin also showed some differences [8–20]. IIF with the use of human skin sections showed IgG anti-keratinocyte cell surface antibodies. In all, of 120 El Bagre-EPF patients whose skin biopsies were taken from perilesional areas, DIF showed positive results. Furthermore, 70% of the patient sera showed IgG anti–basement membrane zone (BMZ) antibodies by IIF. IIF with monoclonal antibodies to human IgG subclasses showed that 80% of El Bagre-EPF showed IgG4 anti-cell surface antibodies [8,9]. In addition, 22% of sera showed IgG1 anti–cell surface antibodies, but no sera showed either IgG2 or IgG3 antibodies. Some sera also showed IgG4 antibodies to the BMZ.
By DIF of biopsy skin, 90% of the El Bagre-EPF sera tested showed reinforcement of reactivity with the BMZ, resembling in several cases the pattern observed in lupus; mostly depositions of C3c, C1q, IgG, IgM, Kappa light chains, Lambda light chains, fibrinogen and albumin (90%), as well as positive reactivity for anti-human IgG3 mAb. On IIF using rat and human skin and anti-human IgA mAb, cell surface staining was observed mainly in the upper layers of the epidermal keratinocytes.
By IIF, positive staining was observed on rat smooth muscle. Positive staining for IgA, IgG and IgM was also detected in the papillary dermis [8–20]. The basal epithelial layer of the rat bladder was also positive IgA and IgM. These findings were observed in patients with the most active disease. The staining observed in these cases differs from that observed in paraneoplastic pemphigus. Presence of immune staining on cardiac tissue was also evident, mainly located at the intercalary level. We also detected immunoreactivity on gastric and intestine tissues from rat was present in the El Bagre-EPF sera. IIF using IgG2 mAb and human skin revealed immune staining against the intermediate filaments, similar to that produced with mAb directed against keratins. IIF using IgG, IgM and IgA mAbs and rat bladder shows immune staining, mainly in the basal layer of the epithelia. IIF on rat stomach using IgG, IgM, and IgA showed goblet cell staining. The antibodies displayed staining between the gastric glands, similar to that produced on smooth muscle. The pattern suggested that these antibodies were directed against endomysial proteins and reticulins 1 and/or 2. We also showed in this study that the immune response is polyclonal in patients affected by El Bagre-EPF, as previously described [8–20]. We concluded that most of El Bagre-EPF patients have autoantibodies to known and many unknown cell junctions, not only in the skin but also other organs. In summary, the autoimmune response is polyclonal in nature.
Most Common Histopathological Alterations in the Lesional Skin
We had performed a case-control matched study comparing the most frequent histopathologic patterns in non-glabrous skin and in glabrous skin observed and their clinical correlation in El Bagre-EPF. The study was performed on non-glabrous skin biopsies of 100 patients from the dominant clinically affected areas (either on the chest, arms or face). Simultaneously, biopsies from the palms were obtained in 10 randomly chosen patients of the 100 total patients [14]. The specimens were examined by H&E staining. The blisters most commonly observed in the subcorneal areas of the epidermis, although in some cases intra-spinous and subepidermal blisters were visualized. Our results showed a very heterogeneous histopathologic patterns in non-glabrous skin, which seemed to correlate with the clinical features. We conclude that the histopathologic features of this new variant of EPF are complex.
Subclinical Oral Involvement in Patients with El Bagre-EPF
We performed a case-control study for oral changes in 45 patients affected by El Bagre-EPF and 45 controls from the endemic area matched by demographics, oral hygiene habits, comorbidities, smoking habits, place of residence, age, sex, and work activity [21]. Oral biopsies were taken and evaluated via H&E, DIF, IIF, CFM, microarray staining and IHC [21]. We found radicular pieces and loss of teeth in in 43/45 El Bagre-EPF patients and 20 of the 45 controls (p < 0.001; confidence interval [CI] 98%). H&E staining showed that 23/45 El Bagre-EPF patients had corneal/subcorneal blistering and lymphohistiocytic infiltrates under the BMZ and around the salivary glands, the periodontal ligament, and the neurovascular bundles in all cell junction structures in the oral cavity; these findings were not seen in the controls (p < 0.001) (CI 98%) [21]. The DIF, IIF CFM, and microarray staining displayed autoantibodies to the salivary glands, including their serous acini and the excretory duct cell junctions, the periodontal ligament, the neurovascular bundles and their cell junctions, striated muscle and their cell junctions, neuroreceptors, and connective tissue cell junctions. The autoantibodies were polyclonal. IgA autoantibodies reactive with neuroreceptors in the glands were positive in 41/45 patients and in 3/45 controls. We concluded that the patients affected by El Bagre-EPF have some oral anomalies and an oral immune response, primarily to cell junctions. The intrinsic oral mucosal immune system, including IgA and secretory IgA, may play an important role in this autoimmunity. Our data contradicts the hypothesis that PF does not affects the oral mucosa due to the Dsg1 compensation theory [21].
Palm Tissue Displaying A Polyclonal Autoimmune Response in El Bagre-EPF Patients
On physical examination, the palms and soles of El Bagre-EPF patients revealed an edematous texture and mild hyperkeratosis, in comparison with the non-glabrous skin of the patients where blisters, pustules or other lesions are commonly found. Based on the preceding observation, we tested the palms of 20 El Bagre-EPF cases and 20 controls from the endemic area for any pathological alterations in the samples by DIF for palm skin biopsies [22]. Our DIF demonstrated pathological deposits of fibrinogen and albumin, as well as IgG, IgA, IgM, IgD and C3c at the epidermal basement membrane zone, around isolated areas in the epidermis, within the dermal vessels and nerves, and in areas surrounding dermal neurovascular structures and sweat glands [22]. Specific markers for blood vessels, including intercellular adhesion molecule 1 (ICAM-1/CD54) and junctional adhesion molecule (JAM-A), as well as specific markers for nerves, including glial fibrillary acidic protein (GFAP), and human neuron specific enolase (NSE) co-localized with the patients’ autoantibodies. Although no blisters, ulcerations, pustules or erosions were clinically observed on the palms of El Bagre-EPF patients, our DIF detected distinct immunoreactivity in palm tissue [22]. These alterations may contribute to the clinically edematous texture of the palms and the mild clinical hyperkeratosis found in most of these patients. We proposed that normal glabrous skin and non-glabrous skin may be different with regard to the expression of selected molecules, which may vary in number, size or structural organization depending on their anatomical site. Our findings may also partially explain the hyperkeratotic palms that have been clinically well documented in the chronic phase of Brazilian FS [22].
Sweat Glands
We examined the El Bagre-EPF patients, and noted several polymorphic clinical lesions around their axillary areas. Based on our clinical and on previous histopathological studies on the skin of these patients that showed abnormalities in their sweat glands, as well as the presence of mercuric selenides and iodine by autometallographic assays, we studied the sweat glands in these patients on the palms that are rich on sweat glands. DIF, IIF, IHC and H&E stains were also done. We visualized a specific autoreactivity to sweat glands in most of the patients and, using IHC using anti-human monoclonal antibodies to CD3, CD20 and CD68, we also detected deposits around the sweat gland’s indicative of specific immune responses in situ, and around the sweat glands. No healthy controls yielded positive findings [23]. In some chronic cases, a decrease or sometimes a complete absence of sweat glands and other skin appendices was found. In addition, sclerodermoid changes or early sclerodermatous changes sometimes extended into the adipose tissue as a membranous lipodystrophy [23]. Autoreactivity to the neurovascular components around the sweat glands were also observed. Our data demonstrate for the first time that there is immunoreactivity toward sweat glands in El Bagre-EPF patients that may destroy some of these structures [23].
Human Eyelid Meibomian Glands and Tarsal Muscle are Recognized by Autoantibodies from Patients Affected by El Bagre-EPF
We performed IIF studies using normal-appearing human eyelid skin from routine blepharoplasties as substrate tissue. We tested sera from 12 patients with El Bagre-EPF and ocular lesions, 5 patients with sporadic (nonendemic) PF, and 20 healthy control subjects (10 from the El Bagre-EPF endemic area and 10 from nonendemic areas). We used FITC-conjugated goat antiserum to human total IgG/IgA/IgM as a secondary antibody [24]. In addition, we used FITC-conjugated antibodies to human fibrinogen, albumin, IgG, IgE, C1q, and C3, Texas Red (Rockland Immunochemicals, Inc, Gilbertsville, PA), and Alexa Fluor 555, or Alexa Fluor 594(Invitrogen, Carlsbad, CA). Ki-67 (a cell proliferation marker) was used to determine the cell proliferation rate, and nuclear counterstaining was performed with either 49, 6-diamidino-2-phenylindole or Topro III (Invitrogen) [24]. We observed autoreactivity to multiple eyelid structures, including meibomian glands and tarsal muscle bundles at different levels, and some areas of the epidermis and the dermis close to the isthmus of the eyelids. Tarsal plate autoreactivity was seen in 10 of 12 of the El Bagre-EPF sera and in one control with pemphigus erythematosus. Furthermore, IP using an eyelid sample as a substrate with 1 mmol/L of sodium orthovanodate showed autoreactivity to several antigens, including some of possible lipid origin [24].
Antibodies to Pilosebaceous Units Along their Neurovascular Supply Routes in Patients Affected by El Bagre-EPF
We tested for El Bagre-EPF patient sera for autoreactivity to pilosebaceous units by utilizing DIF, IIF, CFM, IHC and IEM [25]. H&E staining of skin biopsies revealed that one third of the patients affected by El Bagre-EPF demonstrated some histologic alteration of the pilosebaceous units [25]. By IHC, most El Bagre-EPF biopsies demonstrated evidence of an autoimmune response along the neural and vascular supply routes of the pilosebaceous units. An active immune response was seen with antibodies against human mast cell tryptase, myeloid/histoid antigen, CD8, CD20, CD68, CD117/c-kit, ZAP-70 and vimentin. IEM demonstrated autoantibodies within the hair follicle and at the basement membrane area of the sebaceous glands. El Bagre-EPF patients had autoantibodies to pilosebaceous units and to their surrounding neurovascular packages. Our results may also explain the loss of hair described in severe Brazilian FS before the therapeutic steroid era [25].
Patients with El Bagre-EPF have Autoantibodies against Arrector Pili Muscle, Colocalizing with MYZAP, p0071, Desmoplakins 1 and 2 and ARVCF
We took skin biopsies from 30 patients with El Bagre-EPF and 30 healthy controls (HCs) matched by age, sex and occupation who were all from the endemic area, and tested these using DIF, CFM and IHC tests [26]. We detected that 27/30 patients had autoantibodies to against arrector pili muscle (APM) that colocalized with commercial antibodies to MYZAP, DP I-II, plakophilin 4, and ARVCF (P < 0.001, Fisher’s exact test). The positive staining also colocalized with JAM-A, a control antibody for gap cell junctions. No samples were positive in IHC studies.
In IB, sera of 27/30 patients that were APM-positive, also displayed colocalization with the protein bands shown by antibodies to MYZAP and ARVCF (Progen) (p < 0.001, Fisher’s exact test). We concluded that patients affected by El Bagre-EPF have autoantibodies to APM, colocalizing with the antibodies MYZAP, ARVCF, p0071, DP I-II, suggesting that these molecules are El Bagre-EPF antigens [26]. Further, all of these antigens represent components of cell junctions, indicating that the immune response is directed, at least partially, against cell junctions. We also verified that the immune response in patients affected by El Bagre-EPF is polyclonal, and affecting to B and T lymphocytes, mast cells, IgG, IgA, IgM, IgD, IgE, fibrinogen, albumin, complement/C1q, C3c and C4 [26].
HLA-DPDQDR is Expressed in Lesional Skin from Patients Affected by El Bagre-EPF
Human genes responsible for human antigen presentation and transplant rejection functions are located on the short arm of Chromosome 6, and are called the Major Histocompatibility Complex (MHC). Moreover, the primary physiologic function of MHC molecules is to present peptides to T lymphocytes [27]. MHC molecules are integral components of the ligands that most T cells recognize, since the T cell receptor (TCR) has specificity for complexes of foreign antigenic peptides, as well as self-MHC molecules. We investigated the presence of HLA-DPDQDR within lesional skin biopsies from patients affected by El Bagre-EPF, and compared with controls from the endemic areas [27]. Among patients with El Bagre EPF, 23/30 exhibited positive staining in the upper dermal blood vessels and perivascular inflammatory infiltrates with a significance of p<0.05. Also, positivity was seen around the neurovascular supply structures of sebaceous glands, and around dermal blood vessels surrounding eccrine ducts. Only two controls from the endemic area displayed positive staining, specifically in some upper dermal perivascular infiltrates (p<0.05) [27].
Ribosomal Protein s6-ps240 is Expressed in Lesional Skin from Patients with El Bagre-EPF
In autoimmune skin blistering diseases, autoantibodies seem to trigger several intracellular signaling pathways; we investigated the presence of the phosphorylated form of ribosomal protein S6-pS240 within autoimmune skin blistering diseases biopsies. Therefore, we utilized IHC staining to evaluate the presence of S6-pS240 in lesional skin biopsies of the El Bagre-EPF patients and matched controls from the endemic area [28]. We utilized monoclonal mouse anti-human ribosomal protein antibody S6-pS240; phosphorylation site specific, clone DAK-S6-240, Dako catalog No. M7300, at a dilution of 1:50. We found that the biopsies from the diseased skin showed positive staining for S6-pS240 around lesional blisters, including adjacent areas of the epidermis; in the corneal layer, stratum granulosum, epithelial layers of hair follicles, the sebaceous glands especially at their BMZ, within upper dermal inflammatory infiltrates, and/or mesenchymal-endothelial cell junctions within the dermis. We documented that S6-pS240 is expressed in lesional areas of skin biopsies from patients with El Bagre-EPF disease, as well as on eccrine glands and piloerector muscles [28].
Langerhans Cells, S100, HAM 56, CD68 and CD1a in Lesional Skin from Patients and Controls from the Endemic Area
We noted that populations of epidermal Langerhans cells were significantly decreased in lesional skin, when compared to perilesional skin in El Bagre-EPF patients [29]. In controls from the endemic area, CD1a positive Langerhans cells were quantified as ~1-2 cells/mm2. HAM56 antibody staining was very strongly positive in the EPF cases, especially around dermal neurovascular packages supplying sebaceous glands (a median of 15-18 cells/ mm2), compared to normal controls (~1-2 cells/mm2; p = 0.001) [29]. The HAM56 antibody was also positive in the epidermis above the blisters, and in the dermis under the blisters (1-5 cells/mm2), in comparison to normal skin controls (~1-2 cells/mm2). In regard to CD68 staining, it was also very strongly positive around dermal eccrine gland coils and ducts, and at the edges of the deep adipose tissue in El Bagre-EPF patients (a median of 15-18 cells/mm2), in comparison to normal controls (~1- 2 cells/mm2;( p<= 0.001) [29].
Autoreactivity to Neural Receptors and Nerves in Patients Affected by El Bagre-EPF
We tested the sera of 20 El Bagre-EPF patients, 20 normal controls from the endemic area, and 20 age- and sex matched normal controls from outside the endemic area for the autoreactivity to various nerve components [15]. Both normal human skin and bovine tail were used as antigens. As a result, we detected autoreactivity to neural structures, mechanoreceptors, nerves, perineural cell layers of the arachnoid envelope around the optic nerve, brain structures, and to neuromuscular spindles; these structures colocalized with several neural markers [15]. The patient antibodies also colocalized with DP I-II, ARVCF and p0071. The study also showed autoreactivity with neurovascular bundles innervating the skin, and IEM using gold conjugated-protein A showed that patient antibodies were positive against the nerve axons [15]. Paucicellularity of the intraepidermal nerve endings and defragmentation of the neural plexus were seen in 70% of the cases and not in the controls from the endemic area (p<0.005). Neuropsychological and/or behavioral symptoms were detected in individuals from the endemic area, including sensorimotor axonal neuropathy. Our findings may explain for the first time the “pose of pemphigus,” representing a dorsiflexural posture seen in EPF patient’s vis-a-vis the weakness of the extensor nerves, and furthermore, the autoreactivity to nerves in EPF could explain the “burning sensation” encountered in EPF disease [15].
El Bagre-EPF Patients have Autoantibodies against ARVCF
A critical cell junction protein is armadillo repeat gene deleted in velo-cardio-facial syndrome (ARVCF); we found that this molecule is expressed in the skin and colocalizes with autoantibodies of EL Bagre-EPF patients [30].
Mast Cells, Mast/stem Cell Growth Factor Receptor (C-KIT/CD117) and IgE may be Integral to the Pathogenesis of EPF
Forty-four skin biopsies from EPF patients (30 patients from El Bagre, Colombia, and 14 from the northeastern region of São Paulo State, Brazil), 48 control biopsies from Colombian and Brazilian endemic areas, and additional control biopsies from non-endemic areas in Colombia and the USA were studied. IHC was performed to evaluate skin biopsies with anti-mast cell tryptase (MCT), anti-c-kit and anti-IgE antibodies [31]. We also searched for serum IgE in 30 EPF and 30 non-atopic controls from the El Bagre region by ELISA. In our El Bagre patients and controls, we also searched for IgE in skin samples by DIF. All EPF biopsies showed MCT, c-kit and IgE expressions stronger than control biopsies, especially in the inflammatory infiltrates around upper dermal blood vessels and dermal eccrine glands. IgE staining was positive along the BMZ in some EPF skin samples [31]. Increased IgE serum levels were also noted in EPF patients relative to controls. We concluded that, in patients with EPF, the increased expression of MCT, c-kit and IgE in lesional skin is associated with higher serum IgE levels and may indicate IgE participation in the antigenic response [31]
Cyclooxygenase 2 (COX-2) in Lesional Skin in Patients affected by El Bagre-EPF; Quantitative Digital Morphometry and IHC Staining
We tested skin of 40 patients and 40 controls for the presence of COX-2 [32]. The staining intensity of the antibodies was also evaluated in a semiquantitative mode by an automated computer image analysis system, designed to quantify IHC staining in hematoxylin-counterstained histopathological sections. Slides were scanned with a ScanScope CS system, utilizing brightfield imaging. For IHC, we utilized a Dako monoclonal mouse anti-human COX-2 antibody, clone CX-294[32]. We noted that 26/30 patients with El Bagre-EPF were positive for COX-2 in the epidermis, particularly in spot areas of the corneal layers, around the neurovascular areas of eccrine and hair follicles. Only 2 controls from the endemic area showed some reactivity in the corneal layer (p<0.05) [32].
Proteinase and Proteinase Inhibitors in Patients and Controls
We also evaluated lesional skin of patients and matched controls from the endemic area to study for evidence of tissue damage, regeneration and/or modification using IHC. We tested lesional skin for α-1-antitrypsin, human matrix metalloproteinase 9 (MMP9), human tissue inhibitor of metalloproteinases 1 (TIMP-1), metallothionein and urokinase type plasminogen activator receptor (uPAR). uPAR and MMP9 were basically negative on lesional skin, and only 3 patients with chronic El Bagre-EPF were positive to MMP9 in proximity to telocytes in the dermis [33]. TIMP-1 and metallothionein were positive in several skin appendices in the dermal, inflamed blood vessel inflammation and dermal mesenchymal-epithelial cell junctions. All these findings led us to conclude that the immune response, at least in situ, seems to be more complex, and directed not only to the desmosomes or hemidesmosomes but also to the skin appendices and the junctions of the vessels and the dermal tissue [33].
C5b-9 in Skin Biopsies from Patients and Controls
We also performed a case-control study for the presence of complement/C5b-9 in lesional skin in 43 patients affected by El Bagre-EPF, as well as 43 matched healthy controls from the endemic area using IHC stains. We detected complement/C5b-9 in all cases of the patients affected by El Bagre-EPF, but not in the controls from the endemic area (p < 0.001) [34]. The patients’ IgG and IgM autoantibody titers in IIF were correlated to the intensity of complement/C5-b9 staining (p < 0.001). We concluded that patients affected by El Bagre-EPF have lesional deposition of complement/C5b-9, which links with disease severity and previously established serologies [34].
Rouleaux and Autoagglutination of Erythrocytes Associated with a Pink Material Resembling Fibrin-like Aggregates in Skin Biopsies from Patients Affected by El Bagre-EPF
We documented that rouleaux and the pinkish aggregates are present in within biopsies taken from lesional skin in the majority of patients with El Bagre-EPF; we speculated that this may be as result of the exocytosis of antibodies from inflammatory cells, that form when the cells exposed to the extracellular matrix in the edematous diseased skin. In addition, red blood cells in the presence of plasma proteins or other macromolecules may form aggregates [35]. Rouleaux, a type of autoagglutination of erythrocytes, along with a pink material that resembles fibrinoid aggregates, was observed in 24/30 biopsies from El Bagre-EPF. Skin biopsies from none of the 30 controls from the endemic area showed this positivity. The rouleaux, the aggregated erythrocytes and the pink material were uniformly seen under the blisters [35].
In situ Immune Response Evaluation by IHC in Skin Biopsies from Patients Affected by El Bagre-EPF
We tested by IHC for CD4, CD8, CD19, CD20, CD45, CD56/NCAM, PAX-5, granzyme B, myeloperoxidase, neutrophil elastase, LAT and ZAP-70 in 30 patients affected by El Bagre-EPF, in 15 controls from the endemic area, and 15 biopsies from healthy controls from the USA [36]. We found a predominantly CD8 positive/CD45 positive T cell infiltrate in El Bagre-EPF. El Bagre-EPF patients biopsies displayed negative staining for CD4 and B cell markers, and natural killer cell markers were also rarely seen. ZAP-70 and LAT were frequently detected. In El Bagre-EPF, a significant fragmentation of T cells in lesional skin was noted, as well as autoreactivity to lymph nodes [36]. The documented T cell and myeloperoxidase staining are indicative of the role of T lymphocytes and neutrophils in lesional biopsies in these patients in addition to previously documented deposition of B cells, immunoglobulins and complement in situ. In El Bagre-EPF, T cells could also target lymph nodes [36].
SYSTEMIC AUTOIMMUNITY IN PATIENTS AFFECTED BY EL BAGRE-EPF
Autoantibodies to Full Body Vascular Cell Junctions Colocalize with MYZAP, ARVCF, DP I-II and p0071
We investigated autoreactivity to vessels in all the organs/systems of the body. We compared 57 patients and 57 matched controls from the endemic area. We performed DIF, IIF, CFM, IHC, CFM, IEM, IB, and autometallographic studies [18]. We performed ultrasonography on large patient arteries to investigate vascular anomalies. In addition, we reviewed autopsies on seven patients who died of El Bagre-EPF. We immunoadsorbed positive vessel immunofluorescence with Dsg1 to investigate for new autoantigens. 57/57 patients affected by El Bagre-EPF displayed autoantibodies to vessels in all the organs/systems of the body by all methods (p < 0.01). The autoreactivity was polyclonal, and the patient’s antibodies colocalized with commercial antibodies to DP I-II, p0071, ARVCF, and MYZAP (all from Progen Biotechnik, Germany; p < 0.01; all present at cell junctions) (Fig. 2). Immunoadsorption with Dsg1 on positive vessel immunofluorescence showed that the immune response against the vessels was directed against non-Dsg1 antigen(s). Autometallographic studies showed deposits of metals and metalloids in vessel cell junctions and in erythrocytes of 85% of patients (p < 0.01). We concluded that the immune response to these vascular antigens is likely altering endothelial cells and vessel shapes, thus disturbing hemodynamic flow [18]. The flow alterations likely lead to inflammation and may play a role in the atherogenesis often seen in these patients.
Cardiac Rhythm and Pacemaking Abnormalities in Patients Affected by El Bagre-EPF
We investigated rhythm disturbances with the presence of autoantibodies and correlated them with ECG changes in these patients [19]. We performed a study comparing 30 patients and 30 matched controls from the endemic area. ECG as well as DIF, IIF IHC, CFM studies focusing on cardiac node abnormalities were also studied at autopsies of 7 patients. The main ECG abnormalities seen in the El Bagre-EPF patients were sinus bradycardia (in one-half), followed by left bundle branch block, left posterior fascicular block, and left anterior fascicular block compared with the controls. One-third of the patients displayed polyclonal autoantibodies against the sinoatrial and/or AV nodes, and the His bundle correlating with rhythm anomalies was delayed in the cardiac conduction system (p <.001) [19]. The patient antibodies colocalized with commercial antibodies to DP I-II, p0071, ARVCF, and MYZAP (the last one from Progen Biotechnik) (p <.01). We concluded that one-third of the patients affected by El Bagre-EPF have rhythm abnormalities that slow the conduction of impulses in cardiac nodes and the cardiac conduction system. These abnormalities likely occur as a result of deposition of autoantibodies, complement, and other inflammatory molecules. We demonstrated for the first time that MYZAP is present in cardiac nodes [19].
Autoreactivity to the Heart, Nodes, Conducting System
For autoreactivity to heart, IIF, CFM, IEM and IB were performed utilizing heart extracts as antigens. We found that El Bagre-patients had a polyclonal immune response to cell junctions of the heart, often colocalizing with known markers [18]. These colocalizing markers included the area compositae of the heart, such as DP I-II; markers for gap junctions, such as connexin 43, markers for tight junctions, such as ezrin and junctional adhesion molecule A, and markers for adherens junctions, such as pan-cadherin. We also detected colocalization of the patient antibodies with the blood vessels and with the cardiac sarcomeres [18]. The strongest patient serum autoreactivity was observed against the transverse tubule system of the heart. Reactivity to some nerves and the Purkinje fibers was also noted. We demonstrated that El Bagre-EPF patients display autoreactivity to multiple cardiac epitopes, and, further, that the cardiac pathophysiology of this disorder warrants further evaluation [18]. We also have shown preliminary studies on kidney, and had shown also autoantibodies to the proximal and distal collecting tubes of the kidney as well as against membranes of some mitochondria and cell junctions of these organs.
Patients Affected by El Bagre-EPF have Autoantibodies Colocalizing with MYZAP, p0071, DP I-II and ARVCF, which cause Renal Damage
We detected a systemic pathologic alteration in one third of El Bagre-EPF patients. In the current study, we focused on autoreactivity to the kidney and its pathologic correlations [17]. We investigated patients with El Bagre-EPF for renal compromise. We performed a case control study with 57 patients with El Bagre- EPF and 57 matched controls from the endemic area. We took skin and renal biopsies, performed DIF, IIF IHC, CFM, IB, direct and indirect IEM, and tested kidney function in all living patients. We also used IHC to study seven kidney autopsy samples [17]. Of the 57 patients, 19 had autoantibodies to kidney, with polyclonal reactivity (p < 0.01). Most cases were positive along the basement membrane of the proximal tubules, but in some cases, there was also positivity against the glomeruli and/or mixed patterns. Fifteen patients had increased serum urea and creatinine compared with controls (p < 0.01). The autoantibodies colocalized with DP I-II, p0071, ARCVF and MYZAP (p < 0.01). All of the kidney disease autopsies showed pathologic alterations, mostly in the vessels. We demonstrated for the first time that one third of patients with El Bagre-EPF have polyclonal autoantibodies to kidney. The kidneys showed a mixed histopathological pattern resembling lupus nephritis, with a diffuse proliferative Class IV (G) global diffuse pattern in active lesions, and additional interposition of membranoproliferativ glomerulonephritis [17].
Patients Affected by El Bagre-EPF Exhibit Autoantibodies to Optic Nerve Sheath Envelope Cell Junctions
The majority of the patients with El Bagre EPF experienced vision problems, and we have previously reported several ocular abnormalities. To investigate reactivity to optic nerves in these patients, we utilized bovine, rat and mouse optic nerves, and performed IIF and CFM to test optical nerve autoreactivity in 45 patients and 45 matched controls [37]. Overall, 37 of the 45 patient sera reacted to the optic nerve envelope that is composed of leptomeninges, and the reactivity was polyclonal and present mostly at the cell junctions (P < 0.001). The immune response was directed against optic nerve sheath cell junctions and the vessels inside it, as well as other molecules inside the nerve. No controls were positive. Of interest, all the patient autoantibodies co-localized with commercial antibodies to DP I–II, MYZAP, ARVCF, and plakophilin-4 (p0071) from Progen Biotechnik (p < 0.001) [37]. We conclude that the majority of the patients have autoantibodies to optic nerve sheath envelope cell junctions. These antibodies also co-localize with armadillo repeat gene deleted in ARVCF, p0071 and DP I–II. The clinical significance of our findings remains unknown [37].
Environmental Factors as Putative Triggers of the Disease
The main exacerbation elements are ultraviolet radiation, extreme heat, humidity, stress and well as decreased food intake. The disease has unique autoimmune response due to environmental and genetic factors with photosensitivity [38–42]. Colombia is the fourth largest producer of gold in South America, and is among the 20 major producers in the global ranking [38–45]. The exploitation of metallic and non-metallic minerals can be carried out in soil, sub-soil, or even in riverbeds. In regard to etiologic factors, the focus of El Bagre-EPF is located in a rural mining community that is exposed to high environmental levels of minerals, mercuric sulfides/selenides, metalloids and trace elements (e.g., quartz, rutile, granite, copper, lead, magnetite, and almenite). In the El Bagre area and near areas, municipal alterations of the environment and addition of toxic elements such mercury and cyanide are used to improve of gold extraction [38–45]. The El Bagre area is rich in elements including gold, quartz, micas (biotite and muscovite), potassium, Cu, Pb, Mn, Ni, Zn, Mo, Pu, Au, quartz, rutile, granite, magnetite, almenite, biotite, sulfurs and minerals such as pyrite, chalcopyrite and galena. El Bagre is also rich in metals, metalloids and trace elements based on geological studies that show igneous rocks of the Batholitic of Segovia (Jurassic) are in contact with shales belonging to the Cajamarca Complex (Paleozoic) [38–42]. Quartz veins with gold mineralization have been found embedded in igneous rocks, with grades up to 48 g/ton. Mining in alluvial deposits occurs and the endemic area is rich in quartz, potassium, feldspar (which gives it the pink color in some sectors) and plagioclase, what allows classifying the rock as a Gneiss Quartz-Feldspathic. Micas (biotite and muscovite), potassium feldspar sulfurs and minerals such as pyrite, chalcopyrite and galena are present, which were observed in major quantities in the cretacean sediments. The Bagre-Nechí mining district is known historically by its exploitations of gold in placer deposits associated with Neogene terraces and alluvial deposits formed by the Nechí River [38–42]. Currently, exploration campaigns are being carried out in lode gold manifestations. Two zones within the district will be referred, a northern zone, in the surroundings of the Nechí municipality, where quartz vein structures with thickness over 2m and strike persistence over 2 km, hosted by quartz-diorite intrusive rocks, migmatites and quartz-feldspar gneisses [38–42]. Towards the south zone of the district in El Bagre and Zaragoza municipalities, two vein structures are known, La Ye and El Carmen veins, characterized for presenting thicknesses between 1 and 3 m, they are hosted by intrusive rocks that locally present important igneous facies variations from diorites to granodiorites, intruded in some sectors by aphanitic dykes from basic to intermediate composition. Mineralizations are structurally controlled and this work suggests a direct association to shear zones parallel to the possible main stress responsible of the ancient dextral dynamic along Otú fault, supporting the idea that mineralization’s are of the Orogenic Gold Deposit type [38–42]. The endemic area has a high-grade metamorphic rock and although at this latitude the Otú fault is covered under the hazogen sediments, the rocks on the right bank of the Cauca River in front of Nechí are tentatively attributed to the Chibcha terrain. They are characterized by the dominant presence of quartz-feldespetic gneises with hornblenda and biotite [38–42].
The endemic area is rich in gold. Mercury is commonly used to amalgamate gold. The people in this rural mining community are exposed to high environmental levels of mercury, used for gold extraction, as well as other minerals, metalloids, and trace elements (e.g., quartz, rutile, granite, magnetite, and almenite) and ultraviolet radiation (UV). Metalloids, minerals, and trace elements (e.g., quartz, rutile, granite, magnetite, and almenite) are ubiquitous in El Bagre [38–42].
Mercury has been demonstrated to trigger autoimmune phenomena in rats and mice that possess the proper genetic background.We previously examined fifty control subjects and fifty El Bagre-EPF patients in the testing for the presence of mercury in skin biopsies and hair, using autometallographic and mass spectroscopic analyses, respectively. Simultaneously, serum levels of IgE were measured using and ELISA assay, and we also tested for skin hypersensitivity reactions [43]. We used autometallography; mercuric sulfides/selenides were detected in 14 of 51 skin biopsies distributed similarly in the control and patient groups. However, significantly higher serum IgE levels and mercury concentrations in hair, urine, and nails were found in patients compared with controls. Microscopic scrutiny exposed mercuric sulfides/selenides focused within and around the sweat gland epithelium, as well as in dendritic cells [43]. Five skin biopsies from El Bagre-EPF patients and five from controls that tested positive for the presence of mercuric sulfides/selenides by autometallography were arbitrarily selected for electron microscopic (EM) analysis [42]. This analysis revealed a mixed electron-dense and electron-light material closely associated with desmosomes in patients. Moreover, there were intracellular vesicles containing an amalgam of electron-dense and electron-light materials only in the El Bagre-EPF patients. Thus, El Bagre-EPF patients are exposed to high levels of environmental mercuric sulfides/selenides and other elements [43]. We reported mercuric sulfides/selenides in skin biopsies from people living in a focus of EPF, and we believe based on our evidence, that these compounds may play a role in the pathogenesis of this autoimmune disease.
Active Mine Exploitation Represents Challenging Environments for Microorganisms
The direct consequences of mining in the endemic area create pollution in water bodies, a decrease in biologic diversity, and health problems then emerge in the local communities. Areas with active mining represent challenging environments for microorganisms, due to their extreme conditions such as high pressure and temperature, elevated salt concentrations, a diverse range of acid and alkaline soils/water, and many others abiotic factors. However, a remarkable diversity of microorganisms has been found in these types of habitats including those associated with gold mining activity, where communities of Phylum Proteobacteria, Firmicutes and Actinobacteria, are predominant. Despite the fact that the most profuse organisms are bacteria, representatives of the Archea and Eukarya domains have also been found. The plentiful metabolic capacity of the organisms present in these endemic areas is obvious, and their capability to act as Fe, S, NH3, and CH4 oxidants and SO4 2− reducers has been proven [44]. We have to take into account that multiple microorganisms are present in the endemic area and have metabolic capacities, and we do not know if these can be part of the putative triggering factors. For example, it has been established that some of them accelerate the process of sulfur oxidation and, as such, can be used in biomining and bioleaching. Furthermore, acidophilic microorganisms have allowed the growth of different strategies for the remediation of important contamination problems in the exploitation of minerals; for example, the regulation and management of pH in the precipitation of iron in acid mine drainage. Also, microorganisms, especially bacteria, have great potential in terms of the immobilization and accumulation of heavy metals such as Cu, Pb, Cr, and Fe among others [44].
Genetic
Our studies indicate the model of inheritance in this disease to be mixed, with multifactorial effects within a recessive genotype and strong ancestral Amerindian tribes (such as the Zenues and Embera-Catios) that have historically lived in closed communities, and practiced interracial outbreeding due to the presence of guerilla, paramilitary and military warfare in the endemic area for least in the last forty years. We performed pilot genetic studies and reported that they are some possible models of inheritance in this disease using Complex Segregation Analysis (CSA) and short tandem repeats to distinguish between environmental and/or genetic factors in this illness. The CSA analysis was carried out according to the unified model, implemented using the transmission probabilities implemented in the computer program POINTER, and assessed by using a software package for population genetic data scrutiny, Arlequin [45]. We did pedigree analyses by using Cyrillic 2.1 software, with a total of 30 families with 50 probands (47 males and 3 females) tested. In parallel to the CSA, we tested for the occurrence of short tandem repeats from HLA class II, DQ alpha 1, linking the gene locus D6S291 by using the Hardy-Weinberg-Castle law. Our results show that the best model of inheritance in this disease seem to be a diverse model, with multifactorial effects within a recessive genotype [45]. Two types of conceivable segregation patterns were found; one with robust recessive penetrance in families whose phenotype is more Amerindian-like, and another of likely somatic mutations. We conclude that the penetrance of 10% or less in female patients 60 years of age or older directs that hormones could protect younger females. The highest risk factor for men being affected by the disorder was the NN genotype [45]. These findings were probably due to somatic mutations, and/or strong environmental effects. We also found a protective role for two genetic loci (D6S1019 AND D6S439) in the control group [45].
Treatment/Management
We treated the patients with topical and oral corticosteroids according to their weight, since most biologic therapies were not available due to their high costs. If the patients had a systemic disease and needed more than 40 milligrams of prednisone per day, we hospitalized the patients and added mycophenolate mofetil. We also used antiparasitic medications regularly, as well as calcium and various vitamins, including vitamin D oral supplements.
CONCLUSION
EL Bagre-EPF presents an excellent disease model to study the interactions between among environmental and genetic factors and autoimmunity, and the intricacy of the immune response in this disease is more multifaceted than considered before.
Acknowledgement
To the patients, to Mineros SA, to the Hospital Nuestra Senora del Carmen, to the El Bagre municipality and El Bagre community.
REFERENCES
1. Lever WF, Schaumburg-Lever G. Histopathology of the skin. 1975. Lippincott, Philadelphia.
2. Abréu-Vélez AM, Reason IJ, Howard MS, Roselino AM. Endemic pemphigus foliaceus over a century:Part 1. North Am J Med Sci. 2010:2:51-9.
3. Abréu-Vélez AM, Reason IJ, Howard MS, Roselino AM. Endemic pemphigus foliaceus over a century:Part II. N Am J Med Sci. 2010;2:114-25.
4. Diaz LA, Sampaio SA, Rivitti EA, Martins CR, Cunha PR, Lombardi C, et al. Endemic pemphigus foliaceus (fogo selvagem). I. Clinical features and immunopathology. J Am Acad Dermatol. 1989;20:657-69.
5. Ortega-Loayza AG, Ramos W, Gutierrez EL, Jimenez G, Rojas I, Galarza C. Endemic pemphigus foliaceus in the Peruvian Amazon. Clin Exp Dermatol. 2013;38:594-0.
6. Morini JP, Jomaa B, Gorgi Y, Saguem MH, Nouira R, Roujeau JC, et al. Pemphigus foliaceus in young women. An endemic focus in the Sousse area of Tunisia. Arch Dermatol. 1993;129:69-73.
7. Robledo MA, Prada S, Jaramillo D, Leon W. South American pemphigus foliaceus:study of an epidemic in El Bagre and Nechi, Colombia 1982 to 1986. Br J Dermatol. 1988;118:737-44.
8. Abreu-Velez AM, Hashimoto T, Bollag W, Arroyave ST, Abrèu-Velez CE, Londoño MML, et al. A unique form of endemic pemphigus in Northern Colombia. J Am Acad Dermatol. 2003;49:599-8.
9. Abrèu-Velez AM, Beutner EH, Montoya F, Bollag WB, Hashimoto T. Analyses of autoantigens in a new form of endemic pemphigus foliaceus in Colombia. J Am Acad Dermatol. 2003;49:609-14.
10. Hisamatsu Y, Abreu Velez AM, Amagai M, Ogawa MM, Kanzaki T, Hashimoto T. Comparative study of autoantigen profile between Colombian and Brazilian types of endemic pemphigus foliaceus by various biochemical and molecular biological techniques. J Dermatol Sci. 2003;32:33-41.
11. Abréu-Vélez AM, Javier Patiño P, Montoya F, Bollag WB. The tryptic cleavage product of the mature form of the bovine desmoglein 1 ectodomain is one of the antigen moieties immunoprecipitated by all sera from symptomatic patients affected by a new variant of endemic pemphigus. Eur Journal of Dermatol. 2003;13:359-66.
12. Abréu-Vélez AM, Yepes MM, Patiño PJ, Bollag WB, Montoya F Sr. A cost-effective, sensitive and specific enzyme linked immunosorbent assay useful for detecting a heterogeneous antibody population in sera from people suffering a new variant of endemic pemphigus. Arch Dermatol Res. 2004;295:434-41.
13. Abreu Velez AM, Villa-Robles E, Howard MS. A new variant of endemic pemphigus foliaceus in El-Bagre, Colombia:The Hardy-Weinberg-Castle law and linked short tandem repeats. North Am J Med Sci. 2009;1:169-79.
14. Howard MS, Abreu-Velez AM. Broad histopathologic patterns of non-glabrous skin and glabrous skin from patients with a new variant of endemic pemphigus foliaceus (Part 1). J Cutan Pathol. 2010;37:222-30.
15. Abreu-Velez AM, Howard MS, Yi H, Gao W, Hashimoto T, Grossniklaus HE. Neural system antigens are recognized by autoantibodies from patients affected by a new variant of endemic pemphigus foliaceus in Colombia. J Clin Immunol. 2011;31:356-68.
16. Abreu Velez AM, Yi H, Warfvinge G, Howard MS. Autoantibodies to full body vascular cell junctions colocalize with MYZAP, ARVCF, desmoplakins I and II and p0071 in endemic pemphigus in Colombia, South America. Int J Dermatol. 2018;57:291-98.
17. Abreu-Velez AM, Howard MS, Yi H, Florez-Vargas AA. Patients affected by a new variant of endemic pemphigus foliaceus have autoantibodies colocalizing with MYZAP, p0071, desmoplakins 1-2 and ARVCF, causing renal damage. Clin Exp Dermatol. 2018;43:692-2.
18. Abreu-Velez AM, Howard MS, Jiao Z, Gao W, Yi H, Grossniklaus HE, et al. Cardiac autoantibodies from patients affected by a new variant of endemic pemphigus foliaceus in Colombia, South America. J Clin Immunol. 2011;31:985-97.
19. Abreu Velez AM, Howard MS, Velazquez-Velez JE. Cardiac rhythm and pacemaking abnormalities in patients affected by endemic pemphigus in Colombia may be the result of deposition of autoantibodies, complement, fibrinogen, and other molecules. Heart Rhythm. 2018;15:725-31.
20. Abreu-Velez AM, Upegui-Zapata YA, Valencia-Yepes CA, Upegui-Quiceno E, Jiménez-Echavarría AM, Niño-Pulido CD, et al. Involvement of the Areae Compositae of the Heart in Endemic Pemphigus Foliaceus. Dermatol Pract Concept. 2019;9:181-86.
21. Abreu-Velez AM, Howard MS, Padilla HJL, Tobon-Arroyave S. Subclinical oral involvement in patients with endemic pemphigus foliaceus. Dermatol Pract Concept. 2018;8:252-61.
22. Abreu-Velez AM, Howard MS, Hashimoto T. Palms with a polyclonal autoimmune response in patients affected by a new variant of endemic pemphigus foliaceus in Colombia, South America. Eur J Dermatol. 2010;1:74-81.
23. Abreu-Velez AM, Howard MS, Hashimoto K, Hashimoto T. Autoantibodies to sweat glands detected by different methods in serum and in tissue from patients affected by a new variant of endemic pemphigus foliaceus. Arch Dermatol Res. 2009;301:711-8.
24. Abreu-Velez AM, Howard MS, Hashimoto T, Grossniklaus HE. Human eyelid meibomian glands and tarsal muscle are recognized by autoantibodies from patients affected by a new variant of endemic pemphigus foliaceus in El-Bagre, Colombia, South America. J Am Acad Dermatol. 2010;62:437-47.
25. Abreu Velez AM, Yi H, Gao W, Smoller BR, Grossniklaus HE, Howard MS. Antibodies to pilosebaceous units along their neurovascular supply routes in a new variant of endemic pemphigus foliaceus in Colombia, South America. Eur J Dermatol. 2011;21:371-75.
26. Abreu-Velez AM, Valencia-Yepes CA, Upegui-Zapata YA, Upegui-Quiceno E, Mesa-Herrera NR, Velazquez-Velez JE, et al. Patients with a new variant of endemic pemphigus foliaceus have autoantibodies against arrector pili muscle, colocalizing with MYZAP, p0071, desmoplakins 1 and 2 and ARVCF. Clin Exp Dermatol. 2017;42:874-80.
27. Abreu Velez AM, Calle-Isaza J, Howard MS. HLA-DPDQDR is expressed in lesional skin from patients with autoimmune skin diseases. Our Dermatol Online. 2014;5:125-28.
28. Abreu-Velez AM, Googe PB Jr, Howard MS. Ribosomal protein s6-ps240 is expressed in lesional skin from patients with autoimmune skin blistering diseases. N Am J Med Sci. 2013;5:604-8.
29. Abreu-Velez MA, Calle-Isaza J, Howard MS. CD1a, HAM56, CD68 and S-100 are present in lesional skin biopsies from patients affected by autoimmune blistering diseases. Our Dermatol Online. 2014;5:113-17.
30. Abreu-Velez AM, Yi H, Howard MS. Cell junction protein armadillo repeat gene deleted in velo-cardio-facial syndrome is expressed in the skin and colocalizes with autoantibodies of patients affected by a new variant of endemic pemphigus foliaceus in Colombia. Dermatol Pract Concept. 2017;7:3-8.
31. Abreu Velez AM, Roselino AM, Howard MS. Mast cells, mast/stem cell growth factor receptor (C-KIT/CD117) and IGE may be integral to the pathogenesis of endemic pemphigus foliaceus.Our Dermatol Online. 2013;4(Suppl. 3):596-0.
32. Abreu-Velez AM, Calle-Isaza J, Howard MS. Cyclooxygenase 2 is present in the majority of lesional skin from patients with autoimmune blistering diseases. Our Dermatol Online. 2013;4:476-78.
33. Abreu-Velez AM, Yepes-Naranjo MM, Avila IC, Londoño ML, Googe Jr. PB, Velásquez Velez JE, et al. Tissue inhibitor of metalloproteinase 1, Matrix metalloproteinase 9, ?lpha-1 antitrypsin, metallothionein and urokinase type plasminogen activator receptor in skin biopsies from patients affected by autoimmune blistering diseases. Our Dermatol Online. 2013;4:275-80.
34. Abreu Velez AM, Upegui-Zapata YA, Valencia-Yepes CA, Upegui-Quiceno E, Mesa-Herrera N-R, Jiménez-Echavarria AM, et al. Membrane attack complex (C5B-9 Complex or Mac), is strongly present in lesional skin from patients with endemic pemphigus foliaceus in El Bagre, Colombia. J Cutan Pathol. 2019;46:925-29.
35. Abreu Velez AM, Smoller BR, Howard MS. Rouleaux and autoagglutination of erythrocytes associated with fibrin-like material in skin biopsies form patients with autoimmune blistering diseases Our Dermatol Online. 2013;4(Suppl.3):613-15.
36. Abreu Velez AM, Googe PB, Howard MS. In situ immune response evaluation via immunohistochemistry in skin biopsies from patients affected by autoimmune blistering diseases. Our Dermatol Online. 2013;4(Suppl. 3):606-12.
37. Abreu Velez AM, Gao W, Howard MS. Patients affected by endemic pemphigus foliaceus in Colombia, South America exhibit autoantibodies to optic nerve sheath envelope cell junctions. Dermatol Pract Concept. 2018;8:1-6.
38. Londoño Herrera C, Montoya García JC, Ordóñez Carmona O, Restrepo Álvarez JJ. Characteristics of lode mineralizations in the Bagre- Nechímining district, Antioquia. Bol Cienc Tierra. 2009;26:29-3.
39. https://revistas.unal.edu.co/index.php/rbct/article/view/16567/ 17553. Accesed on June 30, 2020.
40. http://capitalgoldresources.com/projects/san-rafael-mine./ Accesed on June 30, 2020.
41. Cordy P, Veiga MM, Salih I, et al. Mercury contamination from artisanal gold mining in Antioquia, Colombia:The world’s highest per capita mercury pollution. Sci Total Environ. 2011;1:154-60.
42. Echeverry B. Genesis and thermal history of gold mineralization in the Remedios-Segovia Zaragoza Mining District of Norhern Colombia. Tesis de Maestría. Universidad de Shimane. Japón;2006.
43. Abreu Velez AM, Warfvinge G, Leon Herrera W, Abréu Vélez CE, Montoya FM, Hardy DM, et al. Detection of mercury and other undetermined materials in skin biopsies of endemic pemphigus foliaceus. Am J Dermatopathol. 2003;25:384–91.
44. Bustos MC, Ibarra H, Dussan J. The golden activity of Lysinibacillus sphaericus: new insights on gold accumulation and possible nanoparticles biosynthesis. Materials (Basel). 2018;11:1587.
45. Abreu-Velez AM, Villa-Robles E, Howard MS. A new variant of endemic pemphigus foliaceus in El-Bagre, Colombia:The Hardy-Weinberg-Castle law and linked short tandem repeats. N Am J Med Sci. 2009;1:169-79.
Notes
Source of Support: Georgia Dermatopathology Associates, Atlanta, Georgia, USA; Mineros SA; Municipality of El Bagre and Medellin, Antioquia, Colombia, Hospital Nuestra Señora de El Bagre (Antioquia, Colombia), and the Embassy of Japan in Colombia, Bogota, Colombia, South America,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-7692-4133 http://orcid.org/0000-0002-7692-4133 http://orcid.org/0000-0002-9348-6227 http://orcid.org/0000-0002-9348-6227 http://orcid.org/0000-0003-0430-6093 http://orcid.org/0000-0003-0430-6093 |




Comments are closed.