Can demodex incite pseudolymphoma?: A dermoscopic revelation
Subrata Malakar1, Ashwini R Mahesh 2
2
1Department of Dermatology, Rita Skin Foundation, Kolkata, India. 2Department of Dermatology, GSL medical college, Rajahmundry, India
Corresponding author: Dr. Ashwini R Mahesh, E-mail: therightdiagnosis@gmail.com
Submission: 04.07.2019; Acceptance: 05.09.2019
DOI: 10.7241/ourd.20202.28
Cite this article: Malakar S, Mahesh AR. Can demodex incite pseudolymphoma?: A dermoscopic revelation. Our Dermatol Online. 2020;11(2):204-205.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Pseudolymphoma (recently termed as benign Cutaneous lymphoid hyperplasia) is not a specific disease, instead it’s an exaggerated local immune response to known or unknown stimuli that results in a lymphomatous-appearing but benign accumulation of inflammatory cells [1]. The clinical presentation is a skin or red coloured nodule on the face or chest, at times multiple lesions maybe seen [2].
Implicated antigens include medications, vaccination, contact allergens, tattoo dyes, metal implants, although mostly they are idiopathic. Also, bite from arthropods that are infected with bacterial spirochetes such as Borrelia burgdorferi, bite of ixodes tick, medicinal leech can incite them [2–4].
A 70 year old man came to our outpatient clinic with an asymptomatic, solitary, well defined, oval shaped, reddish-brown, firm, nontender, indurated nodule measuring 1.5*1.5 cm on the right cheek. There were no clinical signs of infection, and the patient denied history of trauma, insect bite, scratching, or any medications, particularly anticonvulsants.
Skin biopsy (Fig. 1) from the nodular lesion show dense diffuse and nodular infiltrate of small and large lymphocytes and histiocytoid cells involving the whole of reticular dermis and extending to subcutis. The lymphocytes vary to an extent in size of their nuclei and some of them are in mitosis. Most of the nodules show formation of lymphoid follicles, the majority of the nodules are irregular and the number of blood vessels is increased within them. The subepidermal zone is completely spared by the lymphocytes. Some of the epidermal appendages are visualised. A few eosinophils are scattered within the infiltrate.The biopsy report was consistent with Pseudolymphoma.
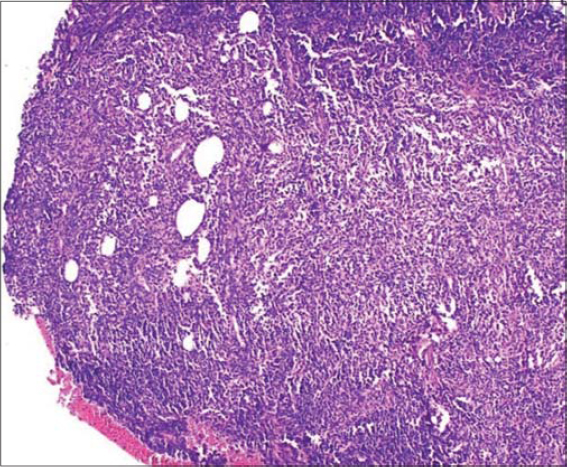 |
Figure 1: Skin biopsy showing dense diffuse and nodular infiltrate of small and large lymphocytes and histiocytoid cells involving the whole of reticular dermis and extending to subcutis. |
On dermoscopic examination (Fig. 2), the surface of the nodule is studded with white spicules at the root of the hair follicle (Demodex tails) and numerous coarse follicular openings (Demodex at follicular openings). Further examination revealed chrysalis structures, linear vessels which in some areas cross the white reticular network, few white scales, on a pinkish background.
A diagnosis of Pseudolymphoma was established on the basis of clinical examination, dermoscopy and histopathological evaluation.
Here, we are describing a case of Pseudolymphoma which on dermoscopy showed the presence of numerous white spicules at the root of hair follicle (Demodex tails) and coarse follicular openings containing Demodex, both specific features of Demodicidiosis [5,6], (Fig.2). The fact that the dermoscopy of the other parts of the facial skin did not reveal any Demodex suggests the association of the parasite with this condition (Fig. 2, purple arrow).
The other dermoscopic findings of chrysalis structures, linear vessels, and few vessels crossing the white reticular network were consistent with the findings of Pseudolymphoma (Fig. 2). Vascular patterns depicting linear vessels across white reticular line suggests the histopathological architecture of dilated blood vessels and thin fibrous septa [7]. Pinkish background suggests underlying vascular proliferation and hyperplasia [6].
Human Demodex, a widely known ectoparasite of pilosebaceous follicle and sebaceous gland resides mainly on the face and head. Symptoms may develop when the follicles become heavily infested (>5/cm2), or when the mites penetrate the dermal tissue [6,8].
The pathogenesis in this case could be chronic antigen stimulation due to profuse infestation with Demodex leading to proliferation of lymphoid cells.
As we could not elucidate any factors stimulating Pseudolymphoma in this case, we can infer that the dermoscopic finding of abundant Demodex is responsible for this pseudolymphatous proliferation.
To the best of our knowledge, we believe our report to be the first to represent a peculiar form of immunological reaction in the form of Pseudolymphoma to Demodex. Thus we feel that more case reports or studies are needed to consolidate the association between them.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Brodell RT, Santa Cruz DJ. Cutaneous Pseudolymphoma. Dermatol Clin. 1985;3:719-34.
2. Ploysangam T, Breneman DL, Mutasim DF. Cutaneous pseudolymphomas. J Am Acad Dermatol. 1998;38:877-95.
3. Altamura D, Calonje E, Liau J, Rogers M, Verdolini R. Diffuse cutaneous Pseudolymphoma due to therapy with medicinal leeches. JAMA Dermatol. 2014;150:783-4.
4. Maubec E, Pinquier L, Viguier M, Caux F, Amsler E, Aractingi S, et al. Vaccination-induced cutaneous Pseudolymphoma. J Am Acad Dermatol. 2005;52:623-9.
5. Segal R, Mimouni D, Feuerman H. Dermoscopy as a diagnostic tool in demodicidosis. Int J Dermatol. 2010;49:1018-23.
6. Malakar S:Dermoscopy. Text and Atlas. New Delhi, Jaypee Brothers Medical Publishers, 2019.
7. Namiki T, Miura K, Tokoro S, Tanaka M, Yokozeki H. Dermoscopic features of lymphocytoma cutis:a case report of a representative dermoscopic feature. J Dermatol. 2016;43:1367-8.
8. Hsu CK, Hsu MM, Lee JY. Demodicosis:a clinicopathological study. J Am Acad Dermatol. 2009;60:453-62.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.