Epidemio-clinical, etiological, therapeutic and evolutive profile of hyperhidrosis: Moroccan experience
Mohamed El Amraoui 1, Abdelhafid Achbouk2, Rachid Frikh1, Naoufal Hjira1, Mohammed Boui1
1, Abdelhafid Achbouk2, Rachid Frikh1, Naoufal Hjira1, Mohammed Boui1
1Dermatology-Venereology, Mohammed V Military Teaching Hospital, Rabat, Morocco. 2Plastic Surgery, Mohammed V Military Teaching Hospital, Rabat, Morocco
Corresponding author: Dr. Mohamed El Amraoui, E-mail: med.elamraoui.dto@gmail.com
Submission: 17.07.2019; Acceptance: 29.09.2019
DOI: 10.7241/ourd.20202.25
Cite this article: El Amraoui M, Achbouk A, Frikh R, Hjira N, Boui M. Epidemio-clinical, etiological, therapeutic and evolutive profi le of hyperhidrosis: Moroccan experience. Our Dermatol Online. 2020;11(2):197-198.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Hyperhidrosis (HH) is an excessive production of sweat which is responsible for aesthetic and social discomfort with a major impact on the quality of life and an increased frequency of infectious complications [1,2]. Despite its relative rarity, it is sometimes a diagnostic and therapeutic puzzle for the dermatologist. We present this prospective descriptive study, conducted over a period of 12 months (June 2017-May 2018), within the dermatology-venereology department of the Mohammed V military training hospital, according to a pre-established operating file.
21 cases were reported, including 65% of women and 35% of men, age of patients ranged between 13 and 44 years with an average of 27.41 years, 59% were of average social class and 41% of class social low. 94% of HH were localized, 6% were generalized and no case of regional HH. The most frequent locations were: 65% palmar, 35% axillary and 29% plantar (Fig. 1). 80% of patients had HH that started with puberty, 41% had an anxiety state and 35% had family cases. The severity according to the HDSS score was: level I 0%, level II 35%, level III 41% and level IV 23%. The treatments used were antiperspirants 65%, Ionophoresis 29%, Oxybutynin 35%, Botulinum toxin 41% and thoracic sympathectomy 23%. The effectiveness of treatments ranged from none to 100% with an average of 64%, the most effective treatments were botulinum toxin and thoracic sympathectomy, the least effective treatments were antiperspirants and Oxybutynin, while ionophoresis is in the intermediate zone. Patient satisfaction ranged from 3/10 to 10/10 with an average of 7.17/10. Tolerance of treatments ranged from 7/10 to 10/10 with an average of 8.7/10. The side effects found were compensatory body sweating following thoracic sympathectomy in one patient.
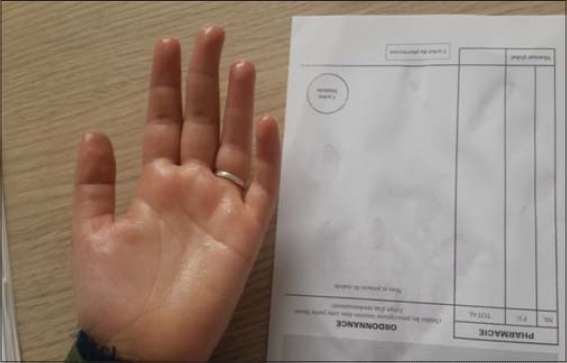 |
Figure 1: Palmar hyperhidrosis in a 16-year-old girl. |
HH in our context is characterized by: young age of onset, female predominance, prevalence of localized forms, frequency of familial forms, frequency of moderate to severe forms, ineffectiveness of antiperspirants and Oxybutynin, the efficacy of botulinum toxin and sympathectomy, a very good satisfaction and tolerance and the scarcity of side effects. HH profoundly impacts the psychic state of particularly young and adolescent patients [1–5]. The mild forms can be managed by antiperspirants, Oxybutynin and iontophoresis while moderate and severe forms justify the use of botulinum toxin or even thoracic sympathectomy and hence the value of multidisciplinary collaboration.
Consent
The examination of the patient wasconductedaccording to the Declaration of Helsinki principles.
REFERENCES
1. Maillard H, Lecouflet M. Management of hyperhidrosis. Ann Dermatol Vénéréol. 2015;142:252-61.
2. Kouris A, Armyra K, Christodoulou C, Karimali P, Karypidis D, Kontochristopoulos G. Quality of life in patients with focal hyperhidrosis before and after treatment with botulinum toxin A. ISRN Dermatol. 2014;2014:30?.
3. Menzinger S, QuenanS. Evaluation et prise en charge de l’hyperhidrose. Rev Med Suisse. 2017;13:710-4.
4. Mordant P, Castier Y, Maury JM, Karsenti A, Paraskevas N, Cerceau P, et al. Prise en charge de l’hyperhidrose primitive invalidante. Sang Thrombose Vaisseaux. 2010;22:302-10.
5. Kettle C, Freiberg A. Axillary hyperhidrosis treatment by simple skin excision and undermining. Can J Plast Surg. 1999;7:267-72.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-7687-0158 http://orcid.org/0000-0001-7687-0158 |



Comments are closed.