Psychotherapeutic methods in psoriasis
Aneta Gruchała , Konrad Marski, Anna Zalewska-Janowska
, Konrad Marski, Anna Zalewska-Janowska
Psychodermatology Department, Clinical Immunology and Rheumatology, Medical University of Lodz, Lodz, Poland
Corresponding author: Dr. Aneta Gruchała, E-mail: aneta.gruchala@stud.umed.lodz.pl
Submission: 11.09.2019; Acceptance: 15.11.2019
DOI: 10.7241/ourd.20202.1
Cite this article: Gruchała A, Marski K, Zalewska-Janowska A. Psychotherapeutic methods in psoriasis. Our Dermatol Online. 2020;11(2):113-119.
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Psoriasis is a chronic inflammatory disease, which is associated with genetic, environmental and lifestyle factors. It is characterized by periods of exacerbations and remissions. Psychological stress or an abnormal response to stressors is reported as an important trigger of exacerbation. The study attempted to systematize and evaluate the psychotherapeutic methods used in treatment of psoriasis based on relevant literature review and meta-analysis model.
Materials and Methods: We searched the PubMed database from its inception to August 2, 2019 and summarized studies based on guidelines outlined in the preferred reporting Items for Systematic Reviews and Meta–Analyses (PRISMA) statement.
Results: The number of articles concerning psychotherapeutic interventions in patients with psoriasis is rather limited. Before screening, seventy four potentially relevant articles were identified. In our study, we included 24 articles: 13 controlled trials, 5 reviews and 6 case reports. Following interventions are described in patients with psoriasis: cognitive behavioural therapy, biofeedback, psychotherapy, meditation, hypnosis, music therapy, exploratory and psychodynamic therapy, emotional writing, systemic family therapy, and support groups.
Conclusions: It can be concluded that in patients with frequent exacerbations of psoriasis, combination of both standard (topical agents, UV phototherapy, systemic agents) and psychotherapeutic intervention, could be of some benefit. More studies are required to show how these approaches could be used in clinical practice. However, at this stage more definite conclusions cannot be drawn.
Key words: Psoriasis; Treatment; Psychotherapeutic methods; Relaxation techniques; Cognitive behavioural therapy
INTRODUCTION
Psoriasis is a chronic immune–mediated inflammatory disease which affects around 2–4% of the population [1]. Occurrence of psoriasis is believed to be associated with genetic, epigenetic, environmental and lifestyle factors [2]. The course of the disease is punctuated by periods of exacerbations and remissions [3]. Psychological stress or an abnormal response to stressors is reported as a trigger of exacerbation and it might have a role in developing the disease in predisposed individuals [4–7]. Feelings of stigmatization, higher levels of social anxiety, negative emotional attitude towards the body and higher levels of depressive symptoms are observed in patients with psoriasis, especially when psoriatic lesions are present on the arms and hands, and on the head and neck [8]. Psychotherapy and stress relief techniques can be helpful in the treatment of the majority of dermatological disorders such as psoriasis, atopic dermatitis, acne vulgaris and alopecia [9,10]. Psychotherapeutic methods reduce stress and anxiety, which enhances the quality of everyday life. Moreover, psychological therapy could provide chances for longer remission in treatment of psoriasis and other chronic dermatological diseases. The aim of the study was to systematize and evaluate the psychotherapeutic methods which could be used in patients with psoriasis based on literature review and meta-analysis.
MATERIAL AND METHODS
We performed rapid literature review using streamlined approach to systematically identify and summarize studies based on guidelines outlined in the preferred reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [10].
We searched the PubMed database from its inception to August 2, 2019. PubMed search terms were as follows.
- (((psychotherapy[Title/Abstract]) OR psychological treatment[Title/Abstract]) AND psoriasis[Title/Abstract]) AND english[Language]
- (((CBT[Title/Abstract]) OR “cognitive behavioural therapy”[Title/Abstract]) AND psoriasis[Title/Abstract]) AND English[Language]
- (((((((((stress reduction[Title/Abstract]) OR stress management[Title/Abstract]) OR yoga[Title/Abstract]) OR meditation[Title/Abstract]) OR emotional disclosure[Title/Abstract]) OR hypnosis[Title/Abstract]) OR music[Title/Abstract]) OR biofeedback[Title/Abstract]) AND psoriasis[Title/Abstract]) AND english[Language]
We included controlled trials, reviews and case reports. Only publications in English were included.
RESULTS
We identified 74 potentially relevant publications. After screening, we included in our study 24 articles: 13 controlled trials, 5 reviews and 6 case reports (Fig. 1),i.e., PRISMA flow diagram for literature review (illustration adapted from official PRISMA website) [11]. In Table I there are presented studies investigating psychotherapeutic methods in psoriasis management. For each controlled trial and case report, we identified: the size of study group, type of intervention, time of intervention and assessment methods.
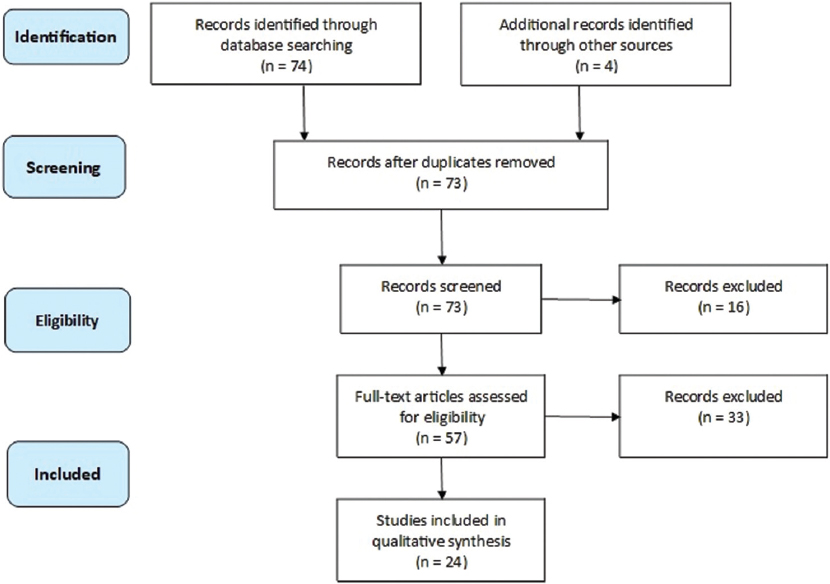 |
Figure 1: PRISMA flow diagram for literature review used in identifying articles about psychotherapeutic methods in psoriasis. n- number of publications (PubMed search) |
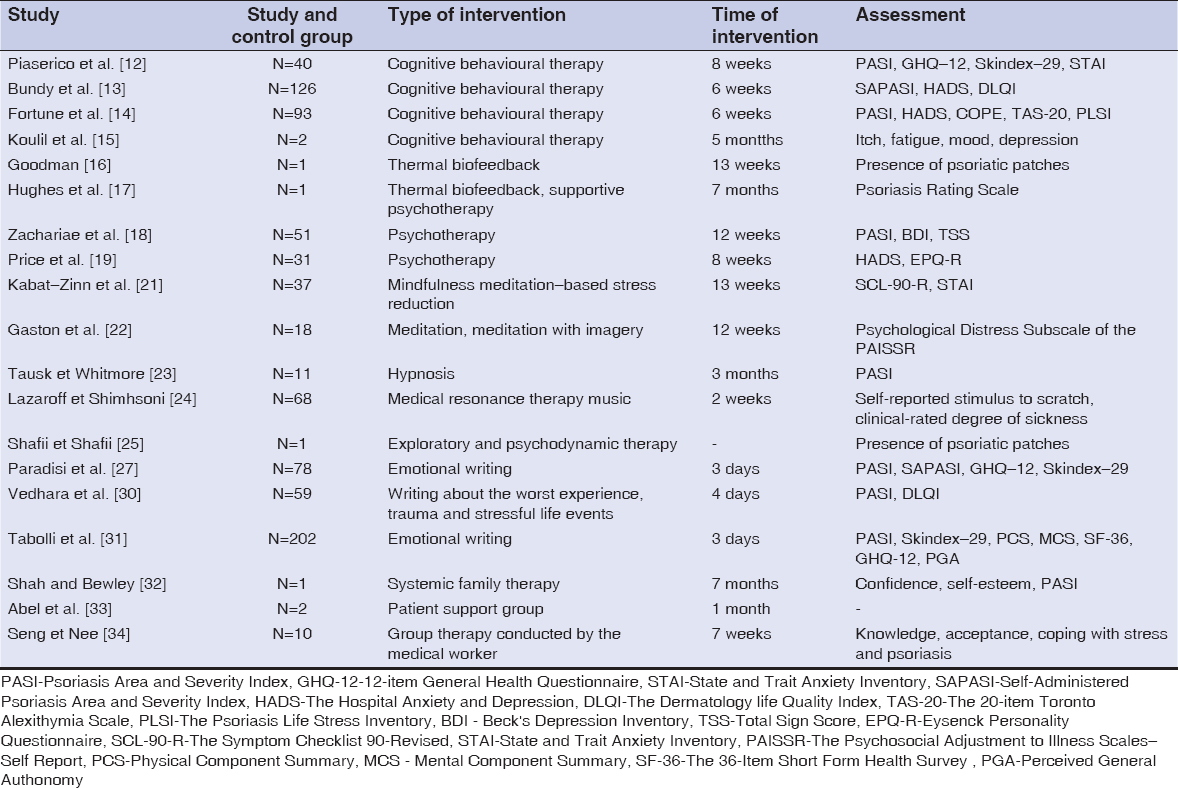 |
Table 1: Studies (controlled trials and case reports) investigating psychotherapeutic methods in psoriasis management |
Cognitive Behavioural Therapy (CBT)
A total of 4 controlled trials and 1 case report on the use of cognitive behavioural therapy in patients with psoriasis were assessed. Piaserico et al. [12] compared effects of 8–week cognitive behavioural therapy (with biofeedback) in patients with psoriasis. The study group consisted of 40 patients treated with narrow–band UVB therapy (20 patients: phototherapy + CBT, 20 patients: only phototherapy). At baseline and by the end of the study, they evaluated clinical severity of psoriasis (PASI), General Health Questionnaire (GHQ)–12 (measure of current mental health), Skindex–29 (life quality questionnaire), and State-Trait Anxiety Inventory (STAI). In the group using CBT, 65% patients achieved PASI75 compared with 15% patients using only phototherapy (p=0.007). GHQ–12 were reduced from 45% to 10% in the group with psychotherapeutic intervention and from 30% to 20% in the control group (p=0.05). The Skindex–29 showed a significant life quality improvement in the cognitive behavioural therapy group compared with control group (-2.8 points, p=0.04). The study shows that CBT increases the beneficial effect of standard therapy in the overall management of psoriasis, reduces the severity of psoriasis, improves life quality and decreases the number of minor psychiatric disorders.
Bundy et al. [13] conducted a study in a group of 126 patients with psoriasis to determine whether an electronic Cognitive Behavioural Therapy intervention for Psoriasis (eTIPs) would reduce distress, severity of the disease and improve the quality of life. The eTIPs program contained six modules of cognitive behavioural therapy tailored to psoriasis patients using a multimedia delivery format to illustrate core concepts. The content of the program focused on the following aspects: management of self–esteem, thinking styles, low mood and depression, stress and tension, enhancing coping with psoriasis, general information, and management of psoriasis. Self–assessed psoriasis severity (Self–Administered Psoriasis Area and Severity Index), distress (Hospital Anxiety and Depression Scale – HADS) and quality of life (Dermatology Life Quality Index – DLQI) were assessed before and after the intervention. Anxiety scores between groups were significantly reduced (p < 0.05) and quality–of–life scores improved (p < 0.05). Neither depression scores nor psoriasis severity scores were significantly lower.
A study by Fortune et al. [14] showed that participation in CBT in addition to standard therapy (n = 40 vs n = 53 for standard therapy) results in a reduction in clinical severity of psoriasis(p = 0.001), anxiety (p = 0.001), depression (p = 0.001), psoriasis–related stress (p = 0.001) and disability (p = 0.04) at 6 weeks and 6 months follow–up.
Koulil et al. [15] described two patients (one patient with psoriasis and one patient with rheumatoid arthritis) under internet–based cognitive–behavioural therapy (ICBT) tailored to their specific problems and treatment goals. The intervention resulted in improved physical and psychological well–being and these improvements were maintained at a 6–month follow–up.
Biofeedback
Goodman [16] described a case report of a 56-year-old Caucasian female who has failed standard medical treatment for psoriasis for seven years. Following 13 weekly one-hour finger/hand thermal biofeedback treatments, all 11 presenting psoriasis lesions (2-6 cm) had disappeared. Interestingly, patient was unmedicated for psoriasis during our treatment and continues to be unmedicated and asymptomatic at 12-month follow-up.
Hughes et al. [17] presented a case of a 31-year-old white male with multiple psoriatic plaques. It was resistant to previous dermatological treatments. During 7 months, each treatment session consisted of 20 minutes of skin temperature training at the target plaque site and following supportive psychotherapy. The photographs using the Psoriasis Rating Scale indicated marked improvement of the dermatological signs.
Relaxation and Meditation Techniques
Zachariae et al. [18] conducted a study in a group of patients (n = 51) with psoriasis. The treatment group participated in seven individual psychotherapy sessions in 12 weeks. Intervention techniques included stress management, guided imagery and relaxation. They observed slight but significant changes in Psoriasis Area Severity Index (PASI), Total Sign Score (TSS) and Laser Doppler Skin Blood Flow (LDBF) in the group of patients which attended psychotherapy sessions.
Price et al. [19] reported that patients with psoriasis are a noticeably anxious group compared to the general population. They conducted psychological meetings, in which the patients discussed among themselves problems caused by the disease. They were also taught specific relaxation techniques for use whenever they felt under stress. This reduced significantly the level of anxiety by the end of the study. Moreover, a modest trend towards physical improvement was also observed.
Bonadonna [20] highlighted that meditation is a good addition to conventional medical therapy in psoriasis. It reduces anxiety, pain, stress and enhances mood and self–esteem.
Kabat–Zinn et al. [21] conducted a study on 37 patients with psoriasis undergoing ultraviolet phototherapy (UVB) or photochemotherapy (PUVA). The study group took part in mindfulness meditation–based stress reduction intervention guided by audio–taped instructions during light treatment. The control group had light treatment alone without the audio–taped instructions. Results showed that patients in the tape group reached the Halfway Point (p = 0.013) and the Clearing Point (p = 0.033) significantly more rapidly than those in the no–tape situation, for both UVB and PUVA treatments. The findings of this research indicating that relaxation and meditation techniques increase the resolution of psoriatic lesions in patients with psoriasis are consistent with previous studies.
Gaston et al. [22] conducted a study in a group of 18 patients with psoriasis symptoms on the scalp. They assigned patients to four groups meditation (n = 5), meditation and imagery (n = 4), waiting list (n = 5) and no treatment control group (n = 4). The intervention lasted 12 weeks, with 4 weeks pre– and post–baseline periods. They confirm that stress reduction techniques can be beneficial in patients with psoriasis.
Hypnosis
Tausk et Whitmore [23] performed a 3-month randomized controlled trial of the use of hypnosis in adults with psoriasis vulgaris. They used highly or moderately hypnotizable subjects. Patients received either hypnosis with active suggestions of improvement (5 patients) or neutral hypnosis with no mention of their disease process (6 patients). Results of the study suggest that hypnosis may be a useful therapeutic methods in psoriasis.
Medical Resonance Therapy Music
Lazaroff et Shimshoni [24] measured the parameters of blood pressure, heart rate, stimulus to scratch and the degree of sickness in the group of 68 patients in total (two experimental groups – psoriasis and neurodermatitis and two control groups). The experimental groups were additionally treated with 3 x 30 minutes of Medical Resonance Therapy Music per day. In the experimental groups was observed a reduction of blood pressure and heart rate, reduction of the stimulus to scratch and reduction in the degree of sickness. Interestingly the effects of therapy were stronger for the patients with psoriasis than for patients with neurodermatitis.
Exploratory and Psychodynamic Therapy
Shafii and Shafii [25] report that the techniques of developing a therapeutic alliance, therapeutic confrontation, clarification, dynamic interpretation, and exploration of intrapsychic and interpersonal conflicts, which are in accord with concepts of exploratory and psychodynamic therapy, can be beneficial in patients with psoriasis.
Emotional Writing (EW)
There are 3 controlled trials evaluating emotional writing in patients with psoriasis.
Nyssen et al. [26] summarized the results of these studies. The main intervention for all studies was the emotional writing including disease–focused writing, including worst experience, trauma and stressful life events. All interventions were delivered in 3 to 4 consecutive days periods for 20 minutes each day and by handwriting.
Paradisi et al. [27] conducted a study on a group of 40 patients with psoriasis undergoing ultraviolet B (UVB) therapy. Besides emotional writing (according to Pennebaker [28]), they assessed one other active intervention based on the emotional positive writing technique focused on the best possible future self and achieving life goals (according to King [29]), Disease severity (PASI and SAPASI scores), psychological distress (GHQ–12 scores) and quality of life (Skindex–29) were assessed at baseline, halfway through and at the end of UVB treatment and 4 months after emotional disclosure intervention. Significant differences in Skindex–29 values between emotional writing group and others were reported. Furthermore, patients allocated to the EW group had a longer period of remission after phototherapy.
Vedhara et al. [30] conducted a study in a group of 59 patients with plaque–type psoriasis involving more 10% of the body area (mean age: 50 years, 32 men and 27 women, mean length of diagnosis: 22 years). Disease severity and quality of life improved in both groups over the follow–up period (at baseline and at 2, 8 and 12 weeks post–intervention).
Tabolli et al. [31] tested the efficacy of Pennebaker’s emotional writing intervention in 67 patients with psoriasis treated with systemic therapy. Total follow–up period for each individual was equal to 12 months. The intervention had little or no effect on the severity of the disease (psoriasis area severity index, Physician Global Assessment Score), as well as generic and dermatology–specific quality life questionnaires.
Systemic Family Therapy
Shah and Bewley [32] underlined that cognitive behavioural therapy (CBT) is not appropriate for everyone. They described a case report showing benefits of a psychological intervention using the principles of systemic family therapy (SFT). The key is the understanding of problems in the context of family and social relationships, and how reciprocal dynamics influence problems. Authors report that problems do not exist only within individuals, however, they are the product of the interactions between people and wider systems, e.g.,communities.
Support Groups
Abel et al. [33] described an experience of patient support group at Stanford, led by a psychiatrist, which is an integral part of the Psoriasis Day Care program. Common discussions topics include lifestyle changes, stressful relationships, associated emotional reactions, occupational limitations and treatment concerns. Psycho–social support systems, stress reduction and enhanced coping skills acquired through shared experiences enhance treatment response.
Seng et Nee [34] used a structured program in a group of 10 patients with psoriasis. The program covered knowledge of psoriasis, feelings of acceptance, stress management, and coping with daily living. Most patients found that the program helped them to cope better with the disease.
Moreover, there were two reviews in which there are described methods of psychological interventions in psoriasis based on literature. Winchell et al. [35] mention about relaxation, hypnosis and biofeedback. Qureshi et al. [36] show numerous methods which could be useful in patients with psoriasis: cognitive behavioural therapy, mindfulness-based therapies, motivational interviewing, educational and interdisciplinary interventions.
DISCUSSION
Despite an extensive review of literature, the number of published articles concerning psychotherapeutic interventions in patients with psoriasis turned out to be rather limited. What is more, issues concerning diagnostic strategies or small study groups in certain works are beyond the scope of this review.
We identify as promising the following psychotherapeutic intervention methods, which can be used in addition to standard therapy in psoriasis patients: cognitive behavioural therapy, biofeedback, psychotherapy, meditation, hypnosis, music therapy, exploratory and psychodynamic therapy, emotional writing, systemic family therapy, and support groups. Thanks to the application of these techniques, one can observe beneficial effects such as reduced severity of psoriasis, improved life quality and decreased incidence of minor psychiatric disorders. For this reason, it can be concluded that patients with frequent exacerbations of psoriasis should use both standard and psychotherapeutic treatment. That seems a good idea that future management of psoriasis should involve multidisciplinary teams that help patients to manage the physical and psychological aspects of psoriasis [37]. More studies are however required to show how these approaches could be used in clinical practice owing to, i.a., (i) the limited number of published works, (ii) small study group sizes, (iii) a lack of comparisons between various methods, (iv) a lack of formulated guidelines.
REFERENCES
1. Parisi R, Symmons DP, Griffiths CE, Ashcroft DM. Global epidemiology of psoriasis:a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133:377-85.
2. Albanesi C, Madonna S, Gisondi P, Girolomoni G. The interplay between keratinocytes and immune cells in the pathogenesis of psoriasis. Front Immunol. 2018;9:1549.
3. Gaikwad R, Deshpande S, Raje S, Dhamdhere DV, Ghate MR. Evaluation of functional impairment in psoriasis. Indian J Dermatol Venereol Leprol. 2006;72:37-40.
4. Heller MM, Lee ES, Koo JY. Stress as an influencing factor in psoriasis. Skin Therapy Lett. 2011;16:1-4.
5. Rousset L, Halioua B. Stress and psoriasis. Int J Dermatol. 2018;57:1165-72.
6. Hunter HJ, Griffiths CE, Kleyn CE. Does psychosocial stress play a role in the exacerbation of psoriasis?Br J Dermatol. 2013;169:965-74.
7. Malhotra SK, Mehta V. Role of stressful life events in induction or exacerbation of psoriasis and chronic urticaria. Indian J Dermatol Venereol Leprol. 2008;74:594-9.
8. Lakuta P, Marcinkiewicz K, Bergler-Czop B, Brzezinska-Wcislo L, Slomian A. Associations between site of skin lesions and depression, social anxiety, body-related emotions and feelings of stigmatization in psoriasis patients. Adv Dermatol Allergol. 2018;35:60-6.
9. Shenefelt PD. Mindfulness-Based Cognitive Hypnotherapy and Skin Disorders. Am J Clin Hypn. 2018;61:34-44.
10. Shenefelt PD. Use of hypnosis, meditation, and biofeedback in dermatology. Clin Dermatol. 2017;35:285-91.
11. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses:the PRISMA statement. PLoS Med. 2009;6:e1000097.
12. Piaserico S, Marinello E, Dessi A, Linder MD, Coccarielli D, Peserico A. Efficacy of biofeedback and cognitive-behavioural therapy in psoriatic patients a single-blind, randomized and controlled study with added narrow-band ultraviolet b therapy. Acta Derm Venereol. 2016;96:91-5.
13. Bundy C, Pinder B, Bucci S, Reeves D, Griffiths CE, Tarrier N. A novel, web-based, psychological intervention for people with psoriasis:the electronic Targeted Intervention for Psoriasis (eTIPs) study. Br J Dermatol. 2013;169:329-36.
14. Fortune DG, Richards HL, Kirby B, Bowcock S, Main CJ, Griffiths CE. A cognitive-behavioural symptom management programme as an adjunct in psoriasis therapy. Br J Dermatol. 2002;146:458-65.
15. Koulil SS, Ferwerda M, van Beugen S, van Middendorp H, van de Kerkhof PCM, van Riel PLCM, et al. Tailored therapist-guided internet-based cognitive-behavioural treatment for psoriasis and rheumatoid arthritis:two case reports. Acta Derm Venereol. 2018;98:225-33.
16. Goodman M. An hypothesis explaining the successful treatment of psoriasis with thermal biofeedback:a case report. Biofeedback Self Regul. 1994;19:347-52.
17. Hughes HH, England R, Goldsmith DA. Biofeedback and psychotherapeutic treatment of psoriasis:a brief report. Psychol Rep. 1981;48:99-102.
18. Zachariae R, Oster H, Bjerring P, Kragballe K. Effects of psychologic intervention on psoriasis:a preliminary report. J Am Acad Dermatol. 1996;34:1008-15.
19. Price ML, Mottahedin I, Mayo PR. Can psychotherapy help patients with psoriasis?Clin Exp Dermatol. 1991;16:114-7.
20. Bonadonna R. Meditation’s impact on chronic illness. Holist Nurs Pract. 2003;17:309-19.
21. Kabat-Zinn J, Wheeler E, Light T, Skillings A, Scharf MJ, Cropley TG, et al. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA). Psychosom Med. 1998;60:625-32.
22. Gaston L, Crombez JC, Lassonde M, Bernier-Buzzanga J, Hodgins S. Psychological stress and psoriasis:experimental and prospective correlational studies. Acta Derm Venereol Suppl (Stockh). 1991;156:37-43.
23. Tausk F, Whitmore SE. A pilot study of hypnosis in the treatment of patients with psoriasis. Psychother Psychosom. 1999;68:221-5.
24. Lazaroff I, Shimshoni R. Effects of Medical Resonance Therapy Music on patients with psoriasis and neurodermatitis-a pilot study. Integr Physiol Behav Sci. 2000;35:189-98.
25. Shafii M, Shafii SL. Exploratory psychotherapy in the treatment of psoriasis. Twelve hundred years ago. Arch Gen Psychiatry. 1979;36:1242-5.
26. Nyssen OP, Taylor SJ, Wong G, Steed E, Bourke L, Lord J, et al. Does therapeutic writing help people with long-term conditions?Systematic review, realist synthesis and economic considerations. Health Technol Assess. 2016;20:1-367.
27. Paradisi A, Abeni D, Finore E, Di Pietro C, Sampogna F, Mazzanti C, et al. Effect of written emotional disclosure interventions in persons with psoriasis undergoing narrow band ultraviolet B phototherapy. Eur J Dermatol. 2010;20:599-605.
28. Pennebaker JW. Writing about emotional experiences as a therapeutic process. Psychological Science. 1997;8:162–6.
29. King LA. The health benefits of writing about life goals. Personal Social Psychol Bull. 2001;27:798–807.
30. Vedhara K, Morris RM, Booth R, Horgan M, Lawrence M, Birchall N. Changes in mood predict disease activity and quality of life in patients with psoriasis following emotional disclosure. J Psychosom Res. 2007;62:611-9.
31. Tabolli S, Naldi L, Pagliarello C, Sampogna F, di Pietro C, Spagnoli A, et al. Evaluation of the impact of writing exercises interventions on quality of life in patients with psoriasis undergoing systemic treatments. Br J Dermatol. 2012;167:1254-64.
32. Shah R, Bewley A. Psoriasis:’the badge of shame’. A case report of a psychological intervention to reduce and potentially clear chronic skin disease. Clin Exp Dermatol. 2014;39:600-3.
33. Abel EA, Moore US, Glathe JP. Psoriasis patient support group and self-care efficacy as an adjunct to day care center treatment. Int J Dermatol. 1990;29:640-3.
34. Seng TK, Nee TS. Group therapy:a useful and supportive treatment for psoriasis patients. Int J Dermatol. 1997;36:110-2.
35. Winchell SA, Watts RA. Relaxation therapies in the treatment of psoriasis and possible pathophysiologic mechanisms. J Am Acad Dermatol. 1988;18:101-4.
36. Qureshi AA, Awosika O, Baruffi F, Rengifo-Pardo M, Ehrlich A. Psychological therapies in management of psoriatic skin disease:a systematic review. Am J Clin Dermatol. 2019;20:607-24.
37. Liluashvili S, Kituashvili T. Dermatology Life Quality Index and disease coping strategies in psoriasis patients. Adv Dermatol Allergol. 2019;XXXVI:419-2.4
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-6689-7354 http://orcid.org/0000-0002-6689-7354 http://orcid.org/0000-0001-8231-9485 http://orcid.org/0000-0001-8231-9485 http://orcid.org/0000-0001-9900-7680 http://orcid.org/0000-0001-9900-7680 |



Comments are closed.