Atypical scleromyxedema improved by immunoglobulins intravenous
Hanane Baybay 1, Amina Lamouaffaq1, Mounia Bennani1, Ghita Senhaji1, Zakia Douhi1, Sara Elloud1, Mounia Rimani2, Fatima Zahra Mernissi1
1, Amina Lamouaffaq1, Mounia Bennani1, Ghita Senhaji1, Zakia Douhi1, Sara Elloud1, Mounia Rimani2, Fatima Zahra Mernissi1
1Department of Dermatology, University Hospital Hassan II, Fez, Morocco; 2Hassan Center of Anatomo-Pathology, Rabat, Morocco
Corresponding author: Dr. Hanane Baybay, E-mail: Hananebaybay@gmail.com
Submission: 08.11.2018; Acceptance: 06.01.2019
DOI: 10.7241/ourd.20194.8
Cite this article: Baybay H, Lamouaffaq A, Bennani M, Senhaji G, Douhi Z, Elloud S, Rimani M, Mernissi FZ. Atypical scleromyxedema improved by immunoglobulins intravenous. Our Dermatol Online. 2019;10(4):352-354.
Citation tools:
BibTex | CSV | RIS | refer/BiblX | Endnote XML
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Scleromyxedema is a rare condition that occurs in middle-aged people. The association with a monoclonal gammopathy is a main criterion for the diagnosis of typical forms. Its pathogenesis is poorly understood. Clinically characterized by a generalized papular eruption with firm papules of 2-3 mm in diameter, waxy in appearance, localised in the hands, forearms, head, neck, upper trunk and thighs. The most frequent extra-cutaneous manifestations include haematological, neurological, cardiac, digestive, rheumatologic and respiratory disorders. Histological findings show fibroblast proliferation, mucin deposition, and fibrosis. The low number of cases and the lack of randomized study make the therapeutic choice difficult. There is currently no formal consensus regarding its therapeutic management. Several therapeutic modalities have been reported such as steroids, retinoids, PUVA, interferon, plasmapheresis, chemotherapy, electrotherapy, thalidomide or immunoglobulins. The efficacy of immunoglobulins intravenous and their lower toxicity make them a treatment of choice for scleromyxedema. We report a case of isolated scleromyxedema with favorable evolution under immunoglobulins and Thalidomide.
Key words: Cleromyxedema, Histology, Immunoglobulins intravenous
INTRODUCTION
Scleromyxedema is a variant of papular mucinosis affecting the skin and internal organs that occurs in middle-aged people [1,2]. The different therapeutic approaches proposed for scleromyxoedema are still unsatisfactory. Intravenous immunoglobulin (IVIg) has been successfully employed in this dermatosis which the evolution is unpredictable [1,2]. The low number of cases and the lack of randomized study make the therapeutic choice difficult. There is currently no formal consensus regarding its therapeutic management [1]. We report a case of isolated scleromyxedema with favorable evolution under immunoglobulins maintained by synthetic antimalarials and Thalidomide.
CASE REPORT
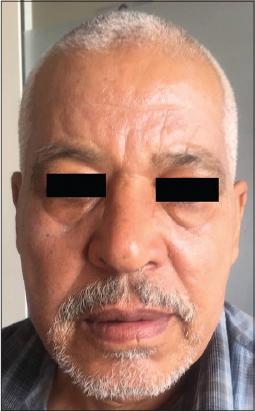
This is a 62-year-old patient, with no pathological history, who presented about 20 days, small papules with normal skin color in some sites and ivory by others, about 2-3 mm in diameter, interesting the face, hands, forearms, neck, upper back as well as retro-auricular, followed by the installation of bilateral palpebral edema with palpebral occlusion, as well as hands and feet (Figs. 1–3). The patient had benefited from a biological assessment showing a negative proteinuria of 24 hours, the assessment in search of monoclonal gammopathy was negative, a correct thyroid assessment. Abdominal CT scan showing digestive thickening of D2 of inflammatory origin. Minimal pericardial effusion at transthoracic echography.
The diagnosis of diffuse scleromyxedema was retained and the patient was placed on intravenous immunoglobulin at a dose of 21 g/day for 5 days/month for 6 months with good improvement after just two months. This regression was maintained by thalidomide at a dose of 100 mg/day combined with synthetic antimalarials at a dose of 200 mg/day (Figs. 4–6). The recoil without recurrence is two years.
Scleromyxedema is a rare disease, that usually affects adults between the ages of 30 and 80 years with no race or gender predominance. The pathogenesis remains unclear, the main hypothesis is that circulating cytokines such as IL-1, TNF-alpha and TGF-beta, which are known to stimulate glycosaminoglycan synthesis and fibroblast proliferation in the skin, could play a role [3,4]. It belongs to the spectrum of cutaneous mucinoses and is characterized by a generalized papular eruption [4]. The rash, very often itchy, consists of firm papules of 2-3 mm in diameter, waxy in appearance [5], closely spaced, dome-shaped or flattopped papules involving the hands, forearms, head, neck, upper trunk and thighs. Papules are often arranged in a strikingly linear array, and the surrounding skin is shiny and indurate (sclerodermoid) in appearance [3]. Evolution is unpredictable. The entire skin can be reached with functional prognosis. The mucous membranes are spared [5]. Extracutaneous manifestations include neurological signs that can lead to coma and death. Cardiac, gastrointestinal, rheumatologic, muscular, vascular specially Raynaud’s syndrome and respiratory manifestations are also described [1,4,5]. Hematologic involvement (monoclonal gammopathy) is very often associated. In 80% of cases, it is a IgG lambda monoclonal dysglobulinemia of undetermined significance, rarely evolving to a myeloma (less than 10%) [2,5]. Histological findings show fibroblast proliferation, mucin deposition, and fibrosis. Because of the rarity of the disorder, there are neither well-designed clinical trials nor consensus about an effective treatment [4].
The prognosis seems reserved with mortality around 30-40% at 2 years [1].
There is currently no formal consensus on therapeutic management, and the treatment is difficult despite the multiplicity of therapeutic possibilities: steroids, retinoids, PUVA, interferon, plasmapheresis, chemotherapy, electrotherapy, thalidomide or veinoglobulins [1,2]. Our patient has improved remarkably since the first treatment cure of immunoglobulins. The Thalidomide combined with synthetic antimalarials were interesting for maintenance treatment because of their immunomodulator and antiinflamatory effect.
CONCLUSION
Scleromyxedema remains a complex pathology that is difficult to treat. The initial efficacy with immunoglobulins is most often remarkable and the side effects are usually minor and transient. However, their use remains limited by their cost and availability. For maintenance treatment; Thalidomide and synthetic antimalarials sounds a good therapeutic modality.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Garcia B, Lasek A, Modiano P. Évolution favorable d’un scléromyxœdème d’Arndt Gottron sous immunoglobulines polyvalentes. Rev Méd Intern. 2017;38;A110–A225.
2. Rongioletti F, Baldari M, Cozzani E, Parodi A. Traitement du scléromyxœdème par immunoglobulines intraveineuses. Ann Dermatol Venereol. 2005;132:9S280-9.
3. Knobler R, Moinzadeh P, Hunzelmann N et al. European dermatology forum S1-guideline on the diagnosis and treatment of sclerosing diseases of the skin, Part 2:Scleromyxedema, scleredema and nephrogenic systemic fibrosisn. J Eur Acad Dermatol Venereol. 2017;31:1581-94.
4. Guarenti I, Sebastiani V, Pinto G, Ricardo de Souza P, De Almeida H. Successful treatment of scleromyxedema with oral thalidomide. Int J Dermatol. 2013;52:631–44.
5. Sillard L, Passeron T, Cardot-Leccia N, Perrin C, Lacour J. P, Ortonne P. Efficacy of intravenous immunoglobulin in the treatment of scleromyxoedema. Ann Dermatol Vénéréol. 2010;137:48-52.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/000-0003-3455-3810 http://orcid.org/000-0003-3455-3810 |







Comments are closed.