Meaning of microalbuminuria during the atopic dermatitis of the child
Ida Aurélie Lenga Loumingou 1, Richard Loumingou2
1, Richard Loumingou2
1Department of Dermatology, University of Brazzaville Medical Center, Brazzaville, Republic of the Congo; 2Department of Nephrology, University of Brazzaville Medical Center, Brazzaville, Republic of the Congo
Corresponding author: Dr. Ida Aurélie Lenga Loumingou, E-mail: idalengaloumingou@gmail.com
Submission: 14.04.2019; Acceptance: 01.05.2019
DOI:110.7241/ourd.20193.5
Cite this article: Lenga Loumingou IA, Loumingou R. Meaning of microalbuminuria during the atopic dermatitis of the child. Our Dermatol Online. 2019;10(3):251-254.
Citation tools:
BibTex | CSV | RIS | refer/BiblX | Endnote XML | Wikipedia Citation Templates
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Objectives: Advocate early diagnosis of vascular diseases in children with atopic dermatitis. Determine children at vascular risk during atopic dermatitis.
Method: The study is transversal and analytical; performed in the University of Brazzaville Medical Center in 18 months. It focuses on children from 0 to 15 years old with atopic dermatitis. The anthropometric, clinical, and antecedent data are collected on cards as well as the balance necessarily including: fasting blood glucose, serum immunoglobulin E (IGE) and microalbuminuria.
Results: 80 patients were selected, 47 girls and 33 boys. The mean age was 8.9 years SD ± 4.646. Obesity is found in 21.25% of cases. 82, 5% of children had hypertensive parents or diabetics in the first degree. Microalbuminuria was positive in 53.75% of cases. It was independent of age and sex and more common in children with hyper IgE.
Conclusion: The study reports arguments for a vascular predisposition and show the interest of achieving microalbuminuria in atopic dermatitis.
Key words:Atopic dermatitis, Arterial hypertension, Diabetes, Microalbuminuria, Child
INTRODUCTION
Atopic dermatitis (AD) is an inflammatory, pruritic and chronic condition of complex etiopathogenesis with implications for hereditary factors and environmental antigens [1]. Atopic dermatitis can be considered as a systemic disease [2], its clinical diagnosis is done by the criteria of the United Kingdom Working Party.
DA is a model of polygenic inheritance that is accompanied by stimulations of secretion of polypeptide substances and chemical mediators with vasoactive activity [1]. Some metabolic manifestations such as obesity and some idiopathic nephrotic syndromes are described in AD [3,4]. The occurrence of arterial hypertension during atopic dermatitis has been suggested [5].
The authors conducted a hospital study to look for a link between AD and common vascular pathologies such as diabetes, high blood pressure and obesity. The interest of this study is to advocate early detection and prevention of vascular diseases in children with AD.
PATIENTS AND METHOD
It is a transversal and analytical study, carried out in University of Brazzaville Medical Center in consultation from January 2015 to July 2016. The study is made by a Dermatologist and a nephrologist hospital-university.
Inclusion criteria were: patients aged 0-15 years with AD. Exclusion criteria were: urinary tract infection or other active infection, ongoing or long-term steroid therapy.
The clinical and laboratory parameters studied were: body mass index, personal and family history of diabetes, high blood pressure, asthma, ambulatory blood pressure measurement with a suitable cuff, fasting blood glucose, blood count, C reactive protein, cytobacteriological examination of urine, ADDIS count, serum immunoglobulin E (IGE), microalbuminuria.
Microalbuminuria was performed on urination, it was considered positive when it was greater than 20ml/g.
The diagnosis of AD was made thanks to the criteria of the United Kingdom Working Party. The severity of the AD was defined by the SCORAD index.
The information was recorded on cards. Data analysis was done by SPSS for calculating averages, standard deviations and correlations.
RESULTS
Epidemiological aspects
374 children were received during the study period among them, 87 had an AD (23.6%) and 80 met the criteria of the study. There were 33 boys and 47 girls. The M/F ratio was 0.7. The average age was 8.9 years SD ± 4.646 years. The average age of girls was 10.19 ± 4.08 and 7.24 ± 4.89 for boys (P = 0.099).
Clinical aspects
There was no diabetes or ongoing hypertension in the patients.13 children were asthmatic (16.25%), 17 obese children (21.25%), 66 children had parents with diabetes or hypertension (82.5%); distributed as follows: high blood pressure (n = 46), hypertension and diabetes (n = 12), diabetes (n = 8).
Biological aspects
Microalbuminuria was positive in 43 cases (53.75%). Mean microalbuminuria was 24.20 ± 21.40. This average was evaluated at 27.4 ± 28.57 for boys and 21.93 ± 14.35 for girls (P = 0.016). 80% of children with microalbuminuria had hypertensive or diabetic parents. IgE was elevated in 45% of patients. The average IgE was 339.2 ± 371.5.
Correlation between microalbuminuria and the different variables studied
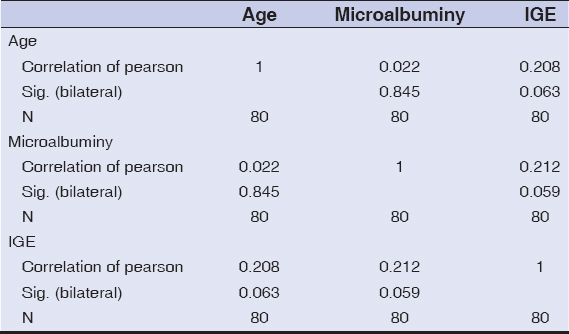
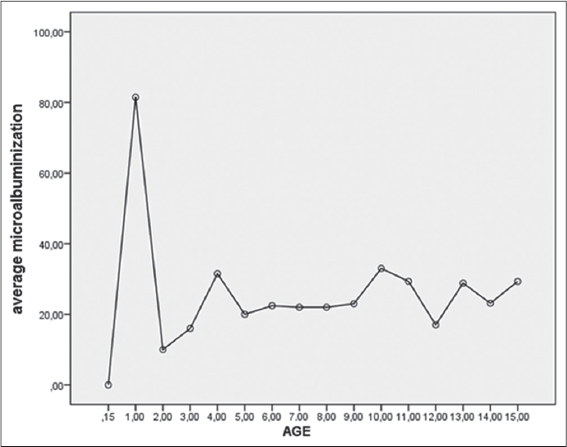
Positive microalbuminuria was found in 47.3% of children in the 0 to 4 age group, 50% had positive microalbuminuria in the age group of 5 to 9 years, and 60% between 10 and 15 years old. The Pearson correlation rate is 0.022, bilateral significance 0.845 (Table 1). The averages of microalbuminuria with respect to age are shown in Fig. 1.
Positive microalbuminuria was found in 45% of children who have hyper IgE. The Pearson correlation was 0.212; Bilateral significance 0.059. The microalbuminuria averages by age group are shown in Fig. 1. There were 13 asthmatic patients among whom 5 (38.4%) had microalbuminuria. Severe AD exist in 23.75% cases, 73.6% of whom had hyper IgE and positive microalbuminuria.
DISCUSSION
Atopic dermatitis is an inflammatory, pruriginous and spongiotic disease [6]. It is considered a systemic disease [2]. prevalence of AD is high but varies by study [7–9]. The classic feminine predominance is found in our study [10]. The penetrance of AD is variable, comorbidity is common [11] other manifestations of atopy are often associated. In the study, 16.25% of children were asthmatic, 24.7% had AD strict.
The physiopathology of AD is complex [1]; it is accompanied by stimulations, secretions of chemical mediators and a high cellular activity [12]. These mechanisms are arguments for an alteration of the endothelial tissue. There is a relationship between inflammatory mediators and vascular and metabolic risk factors: interleukin 6 induces insulin resistance [13], cytokines (TNF, IL6, interferon gamma) have a pro-inflammatory role [14], T h 1, T h 2 regulatory T lymphocytes, whose activity is crucial in AD, induce atherosclerosis [15], podocyte damage is found in the idiopathic nephrotic syndromes of atopic subjects [16].
The arguments for a vascular predisposition in our study are: 82.5% of first degree parents were diabetic and or hypertensive, the positivity of microalbuminuria in 53.75% of children.
The association of AD with obesity, diabetes and arterial hypertension is gaining acceptance [17,18]. The link between idiopathic nephrotic syndrome and atopic dermatitis has been suggested [4,16]. In our study 26.25% of children were obese. No child was hypertensive or diabetic. For Zhang [19], obesity is controversial in AD but is frequently reported in studies such as Kusunoki [3] and Lim [20]. The small sample in the study did not allow us to associate obesity with AD. Microalbuminuria reflects either a rise in capillary pressure or an alteration of the triple glomerular barrier or a generalized endothelial dysfunction it is a risk factor cardiovascular whose interest is established in the management of diabetes and high blood pressure [21]. Positive microalbuminuria appeared to exist independently of age, more than half of the patients had positive microalbuminuria. We did not find an explanation for the peak before the age of two. The positivity of microalbuminuria appeared to be related to the elevation of immunoglobulin E and the severity of AD.
CONCLUSION
The existence of pathological microalbuminuria in children with AD seems to be relevant. It seems important to systematically look for personal and familial vascular risk factors in children with AD, to ensure optimal prevention of common vascular diseases.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Barbarot S, Physiopathologie de la dermatite atopique et perspectives thérapeutiques systémiquesRéal Thér Dermato-Vénérol 2016; 256: 1-
2. Darlenski R, Kazandjeva J, Hristakieva E, Fluhr JW, Atopic dermatitis as a systemic diseaseClin Dermatol 2014; 32: 409-13.
3. Kusunoki T, Obesity and atopic dermatitis, allergic rhinitisArerugi 2017; 66: 984-9.
4. Audard V, Lang P, Sahali DIL, Pathogénie du syndrome néphrotique àlésions glomérulaires minimesMed Sci (Paris) 2008; 24: 853-8.
5. Silverberg JL, Becker L, Kwasny M, Menter A, Kordoro KM, Paller AS, Central obesity and high blood pressure in pediatric patient with atopic dermatitisJ Am Acad Dermatol 2015; 151: 144-52.
6. Misery L, Atopic dermatidis: new trends and persoectivesClin Rev Allerg Immunol 2011; 41: 296-7.
7. Baghoud S, Prévalence et profil clinique de la Dermatite atopique en AlgérieAnn Dermatol Vénérol 2012; 9: 13140-
8. Kay J, Gawkrodger DJ, Mortimer MJ, Jaron AG, The prevalence of childhood atopic eczema in a general populationJ Am Acad Dermatol 1994; 30: 35-9.
9. Xu F, Yan S, Li F, Cai M, Chai W, Wu M, Prevalence of childhood atopic dermatitis an urban and rural community-based study in Shanghai, ChinaPLOS One 2012; 7: e36174-
10. Charpin D, Vervloet D, Présentation générale de l’étude ISAACRev Françd’Allergol d’Immunol Clin 1998; 38: 375-382.
11. Davis D, Practice gaps. Pediatric atopic dermatitis and associated morbiditiesJ Am Acad Dermatol 2015; 151: 152-3.
12. Gittler JK, Shemer A, Suarez Farinas M, Fuentes-Duculan J, Gulewicz KJ, Wang CQ, Progressive activation of Th2 Th22 cytokines and selective epidermal proteins characterizes acute and chronic atopic dermatitisJ Allergy Clin Immunol 2012; 130: 1344-54.
13. Bastard J P, Feve B, Insulino résistance et Diabète: Quel rôle jouent les interleukinesSTV 2009; 21: 307-14.
14. Ait oufella H, Tedgui A, Mallat Z, L’athérosclérose: une maladie inflammatoireSTV 2008; 20: 25-33.
15. Robertson AK, Hansson GK, T cells in artherogenesis: for better or worseAterioscler Thromb Vasc Biol 2006; 26: 2421-32.
16. Wei CC, Lin CL, Shen TC, Sung FC, Occurrence of common allergic diseases in children with idiopathic nephrotic syndromeJ Epidemiol 2015; 25: 370-7.
17. Thyssen JP, Halling-Overgaard AS, Andersen YMF, Gislason G, Skov L, Egerberg A, The association between cardiovascular disease and type 2 diabetes in adults with atopic dermatitis: a systematic review and meta-analysisJ Dermatol 2018; 178: 879-88.
18. Andersen YMF, Egeberg A, Hamann CR, Skov L, Gislason GH, Skaaby T, Linneberg A, Thyssen JP, Poor agreement in questionnaire-based diagnostic criteria for adult atopic dermatitis is a challenge when examining cardiovascular comorbidityAllergy 2018; 73: 923-31.
19. Zhang A, Silverberg JI, Association of atopic dermatitis with bering overweight and obese: a systematic review and meta analysisJ Am Acad Dermatol 2015; 72: 606-16.
20. Lim MS, Lee CH, Sim S, Hong SK, Choi HG, Physical Activity, Sedentary Habits, Sleep, and Obesity are Associated with Asthma, Allergic Rhinitis, and Atopic Dermatitis in Korean AdolescentsYonsei Med J 2017; 58: 1040-6.
21. Sizinger H, Kritz H, La microalbuminurie est elle un facteur de risque en pathologie vasculaireSang Thromb Vaiss 1995; 7: 613-8.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|


Comments are closed.