Unusual presentation of pyoderma gangrenosum in an infant
Ouiam El Anzi 1, Asmae Sqalli1, Safae Maouni1, Kaoutar Znati2, Mariame Meziane1, Nadia Ismaili1, Laila Benzekri1, Karima Senouci1, Badredine Hassam1
1, Asmae Sqalli1, Safae Maouni1, Kaoutar Znati2, Mariame Meziane1, Nadia Ismaili1, Laila Benzekri1, Karima Senouci1, Badredine Hassam1
1Department of Dermatology-Venereology, Ibn Sina University Hospital, Mohammed V University, Rabat, Morocco; 2Department of Anatomopathology, Ibn Sina University Hospital, Mohammed V University, Rabat, Morocco
Corresponding author: Dr. Ouiam El Anzi, E-mail: elanzi.ouiam@gmail.com
Submission: 18.11.2018; Acceptance: 25.01.2019
DOI: 10.7241/ourd.20193.26
Cite this article: El Anzi O, Sqalli A, Maouni S, Znati K, Meziane M, Ismaili N, Benzekri I, Senouci K, Hassam B. Unusual presentation of pyoderma gangrenosum in an infant. Our Dermatol Online. 2019;10(3):308-309.
Citation tools:
BibTex | CSV | RIS | refer/BiblX | Endnote XML | Wikipedia Citation Templates
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Pyoderma gangrenosum (PG) is a sterile neutrophilic disorder that rarely affects children [1], only 21 cases were reported in literature. It is often associated with a concomitant disease, although up to half of cases are considered idiopathic [2].
We report the case of a 12-year-old child, with no particular antecedent, who consulted for multiple painful and ulcerative lesions evolving for 8 months, he was initially treated for presumed bacterial and viral infections with oral antibiotics and antivirals, with no response.
Physical examination revealed 2 small ulcers and 3 large ulcers measuring 3 to 8 cm with irregular borders, undermined edges and indurated base following a linear distribution along the right leg (Fig. 1).
There was no lymphadenopathy. Hematological and biochemical examination did not reveal any abnormality.
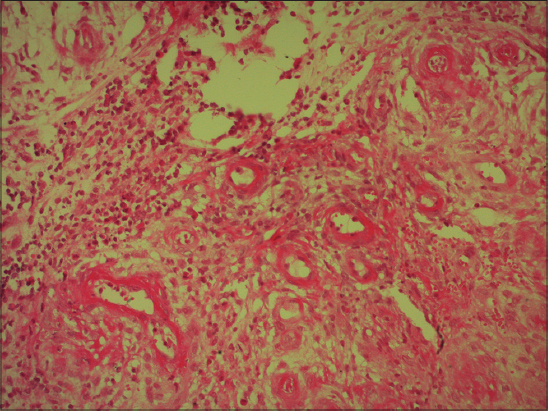
Biopsy was performed from the ulcer edge for histopathologic evaluation and tissue cultures for bacteria, fungi, and atypical mycobacteria.
The histological examination revealed A moderately dense superficial and deep lymphoplasmocytic infiltrate around the vessels (Fig. 2), confirmed the diagnosis of PG. A report looking for associated diseases revealed no anomalies. Oral corticosteroid therapy at a rate of 1 mg/kg/day allowed the healing of lesions with good progress.
Pyoderma gangrenosum is relatively rare in the pediatric population with only 4% of PG occurring in children.
The most common presentation of PG in children is disseminated ulcerative lesions with lower extremities most frequently affected when lesions are localized [1].
The cause of PG is unknown, but some studies have suggested that abnormal neutrophil chemotaxis is the primary process.
PG is an inflammatory condition of the skin first described by Brunsting and colleagues in 1930. PG begins as a pustule or vesiculopustule that progresses to an ulcer or deep erosion with violaceous overhanging or undermined borders [3].
In adults, an associated pathology is present in 74% of cases including a chronic inflammatory bowel disease, hemopathy or rheumatoid arthritis.
While in children, pyoderma gangrenosum is idiopathic in 50% of cases.
Our patient had no associated pathology.
The sporotrichoid character has never been described before, it may be explained in our patient by repeated trauma.
Optimal treatment for infantile PG is not established due to disease rarity and paucity of data. Treatment is based on systemic corticosteroids. In case of corticoresistance, the use of other immunosuppressors could be effective.
Through this observation, we report a new case of PG in children with no associated diseases and with sporotrichoid-like presentation which has never been described before.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Kechichian E, Haber R, Mourad N, El Khoury R, Jabbour S, Tomb R. Pediatric pyoderma gangrenosum:a systematic review and update. Int J Dermatol. 2017;56:486-95.
2. Crouse L, McShane D1, Morrell DS1, Wu EY. Pyoderma gangrenosum in an infant:A case report and review of the literature. Pediatr Dermatol. 2018;35:e257-61.
3. Agrawal S, Singhania B. Pyoderma gangrenosum, BMJ Case Rep. 2010;2010. pii:bcr0420102942.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.