Necrotizing fasciitis after central venous catheter placement
Nassiba Zerrouki 1, Ounci Es-Saad2, Brahim Housni2, Siham Dikhaye1, 3, Nada Zizi1, 3
1, Ounci Es-Saad2, Brahim Housni2, Siham Dikhaye1, 3, Nada Zizi1, 3
1Department of Dermatology, University of Mohammed First, Faculty of Medicine and Pharmacy – Mohammed 6 University Hospital of Oujda, Morocco; 2Department of Anesthesiology and Reanimation, University of Mohammed First, Faculty of Medicine and Pharmacy, Mohammed 6 University Hospital of Oujda, Morocco; 3Laboratory of Epidemiology, Clinical Research and Public Health
Corresponding author: Dr. Nassiba Zerrouki, E-mail: zerrouki.nassiba@gmail.com
Submission: 01.10.2018; Acceptance: 05.12.2018
DOI: 10.7241/ourd.20193.18
Cite this article: Zerrouki N, Es-Saad O, Housni B, Dikhaye S, Zizi N. Necrotizing fasciitis after central venous catheter placement. Our Dermatol Online. 2019;10(3):289-291.
Citation tools:
BibTex | CSV | RIS | refer/BiblX | Endnote XML | Wikipedia Citation Templates
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Necrotizing fasciitis (NF) can appear after various penetrating or non-penetrating skin lesions. This is the second reported case in which NF occurred after a central venous line placement. A 60-year-old woman admitted to intensive care unit for the management of acute coronary syndrome complicated by cardiopulmonary arrest. Ten days after central venous placement in the left internal jugular vein, a reddening and swelling of the insertion site were observed. The evolution was characterized by aggravation of the local symptoms occurred, and the diagnosis of NF was made. The patient died before performing surgically debridement This report on NF in a critically ill patient due to a subclavian central intravenous line aims to encourage checking for iatrogenic soft tissue condition in sedated intensive care patients. These patients may have a greater risk of developing NF, because they often have predisposing factors such as diabetes, end-stage renal failure, and immune suppression.
Key words:Necrotizing fasciitis, Mortality, Central venous catheter
INTRODUCTION
Necrotizing Fasciitis (NF) is a rare. NF is a bacterial derma-hypodermitis affecting the soft tissue and muscular fascia. It is an uncommon and severe infection caused by microorganisms called ‘flesh eating bacteria’, mainly represented by group A beta-haemolytic streptococcus. NF remains a life-threatening condition associated with a high mortality rate [1,2]. Its location to the chest wall is extremely rare [1]. We report the second case in which NF occurred after a central venous line placement.
CLINICAL CASE
A 60-year-old patient, with a clinical history of poorly balanced diabetic, hypertension, and obesity, was admitted to the emergency department for the management of acute coronary syndrome complicated by left ventricular failure. Coronography revealed an atheromatous coronary network with a long tight stenosis of the first segment of the right coronary and a moderate lesion of the mean coronary. The patient underwent angioplasty of the right coronary with placement of an active stent.
During the post-angioplasty follow-up, the patient presented a haemorrhagic shock following a parietal and retroperitoneal hematoma by breach of the external iliac artery, complicated by Cardio-pulmonary arrest. She was hospitalized in intensive care unit, where she underwent cardiopulmonary resuscitation with placement of a central left internal jugular vein.
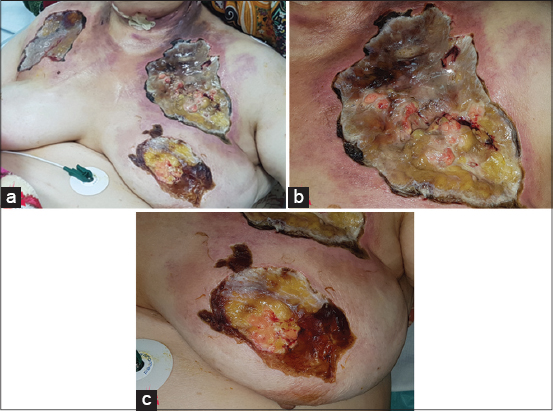
The evolution was marked by the appearance of a poorly circumscribed erythematous, hot, painful and infiltrated placard at the left jugular region rapidly extended to the breast region, contralateral jugular region and anterior chest wall, progressing to ulceration and necrosis with a fever at 39 ° C (Figs. 1a–c).
Biological assessment revealed an inflammatory syndrome (CRP: 405 mg/L), hyperleucocytosis (GB: 43,300 G/L); an increase of lactates to 4.4 mmol/L, CPK to 900 IU/L and transaminases (ASAT: 354 IU/L, ALT: 464 IU/L) and a deterioration of renal function (creatinine: 13 micromol/Glomerular filtration rate: 42 ml/min). The patient rapidly deteriorated hemodynamically, and required the introduction of vasoactive drugs. Disorders of consciousness appeared, and the patient was therefore sedated and intubated.
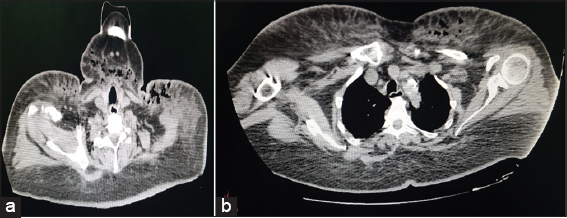
An AngioTDM demonstrated a regression of the right parietal hematoma with the appearance of a large infiltration of the cutaneous and subcutaneous soft tissues of the thoracic wall and multiple air bubbles (Figs. 2a and b). The bacteriological study showed Gram-positive Cocci and gram-negative bacilli. Histological study confirmed the diagnosis of necrotizing fasciitis. The patient was made under broad-spectrum ATB. She died of septic shock before surgical debridement
DISCUSSION
Central venous catheters (CVC) cause more than 90% of all catheter-associated infections. Typically, subclavian access is considered as the preferable approach for a CVC from an infectious point of view [3]. However, severe complications such as catheter-related blood stream infections or cellulitis are possible. Therefore, strict criteria for CVC placement must be met and daily monitoring of the insertion site must be performed [3]. Necrotizing fasciitis is a rare but severe soft tissue infection. The incidence is reported to be 0.4 cases per 100,000 populations [4]. NF is associated with a high mortality rate [1].
Three types are distinguished: Type I is caused by a polymicrobial infection consisting with at least one anaerobic or facultative anaerobic bacterium. Type II is monomicrobial, mainly triggered by b-hemolytic streptococci or staphylococci. Among those, a large variety of different bacteria causing NF is published in literature. Type III is reported to be induced by Vibrio species after minor injuries in salt water [5]. Necrotizing fasciitis can occur after different skin lesions and even in intact skin by hematologous spreading or by blunt trauma [6]. The first case of Necrotizing fasciitis after CVC placement has been described by N. Leibig et all. in 2014 [3]. Our case is the second case of NF after CVC placement.
A laboratory scoring system was created for NF, namely, the laboratory risk indicator for necrotizing fasciitis (LRINEC) [7]. C-reactive protein, WBC count, and hemoglobin, sodium, creatinine, and glucose concentrations, are integrated into the score. On the day of NF diagnosis, the patient had a LRINEC score of 10, which is believed to be high risk with a probability of ‡ 75% for NF.
Publications show that early diagnosis, within 24 h, is missed in 85%–100% of all cases. Late determination of NF is combined with increasing mortality. If the suspected diagnosis is made, surgical intervention in terms of radical and adequate debridement is required immediately [3].
Sufficient soft tissue coverage after stabilization reduces the rate of re-infection, and all techniques in reconstructive surgery are required including free flaps. In many cases patients should be transferred to specialized centers for plastic and reconstructive surgery, optionally with a burn intensive care unit, for coverage after initial debridement [3].
CONCLUSION
NF is a challenging and potentially lethal disease. Early diagnosis and aggressive multidisciplinary treatment is mandatory. Such rare complications can be avoided by following strict aseptic precautions when placing the Central Venous Catheter.
Acknowledgements
We would like to thank Pr RIMANI Mounia for her expertise in anatomopathology.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Safran DB, Sullivan WG, Necrotizing fasciitis of the chest wallAnn Thorac Surg 2001; 72: 1362-4.
2. Kalkat MS, Rajesh PB, Hendrickse C, Necrotizing fasciitis of chest wall complicating empyema thoracisInteract Cardio Vasc Thorac Surg 2003; 2: 358-60.
3. Leibig N, Hirche C, Schmidt VJ, Bigdeli AK, Kneser U, Kremer T, Necrotizing fasciitis after central venous catheter placementSurg Infect (Larchmt) 2014; 15: 850-2.
4. Lancerotto L, Tocco I, Salmaso R, Vindigni V, Bassetto F, Necrotizing fasciitis: Classification, diagnosis, and managementJ Trauma Acute Care Surg 2012; 72: 560-6.
5. Tsai YH, Huang TJ, Hsu RW, Weng YJ, Hsu WH, Huang KC, Necrotizing softt issue infections and primary sepsis caused by Vibrio vulnificus and Vibrio cholerae non-O1J Trauma 2009; 66: 899-905.
6. Morrison EJ, Wei BP, Hadj AK, Adlard RE, Choi WT, Don’t miss it: A rare case of multifocal necrotizing fasciitisANZ J Surg 2014; 84: 487-9.
7. Narasimhan V, Laboratory risk indicator for necrotizing fasciitis score for early diagnosis of necrotizing fasciitis in DarwinANZ J Surg 2018; 88: E45-9.j.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|


Comments are closed.