Linear IgA bullous disease presenting as a Hailey-Hailey disease associated with Hashimoto thyroiditis: a case report
Katarzyna Tomaszewska 1,2, Magdalena Oszukowska1, Anna Zalewska-Janowska2, Andrzej Kaszuba1
1,2, Magdalena Oszukowska1, Anna Zalewska-Janowska2, Andrzej Kaszuba1
1Department of Dermatology, Pediatric Dermatology and Oncology, Medical University of Lodz, Lodz, Poland; 2Department of Psychodermatology, Chair of Clinical Immunology and Rheumatology, Medical University of Lodz, Lodz, Poland
Corresponding author: Dr. Katarzyna Tomaszewska, E-mail: tomaszewska.katarzyna@o2.pl
Submission: 08.01.2019; Acceptance: 08.03.2019
DOI: 10.7241/ourd.20193.16
Cite this article: Tomaszewska K, Oszukowska M, Zalewska-Janowska A, Kaszuba A. Linear IgA bullous disease presenting as a Hailey-Hailey disease associated with Hashimoto thyroiditis: a case report. Our Dermatol Online. 2019;10(3):284-285.
Citation tools:
BibTex | CSV | RIS | refer/BiblX | Endnote XML | Wikipedia Citation Templates
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Linear IgA bullous disease (LABD) is a rare autoimmune subepidermal bullous disease characterized by linear deposits of IgA anti-basement membrane zone antibodies. The skin lesions are variable: papular, vesicular, bullous, erythematous, edematous, and erythema multiforme-like, mimicking bullous pemphigoid, dermatitis herpetiformis, toxic epidermal necrolysis, mucous membrane pemphigoid or in described case – Hailey-Hailey disease. We present a case of a 17-year-old female patient diagnosed with LABD associated with Hashimoto thyroiditis
Key words:Autoimmune disease, Bullous disease, Clinical dermatology
INTRODUCTION
Linear IgA bullous disease (LABD) is a rare autoimmune subepidermal bullous disease characterized by linear deposits of IgA anti-basement membrane zone antibodies. Most cases of LABD are idiopathic and the etiology of the disease remains unclear, but some cases are occasionally induced by drugs, internal malignancies, and infections [1].
CASE REPORT
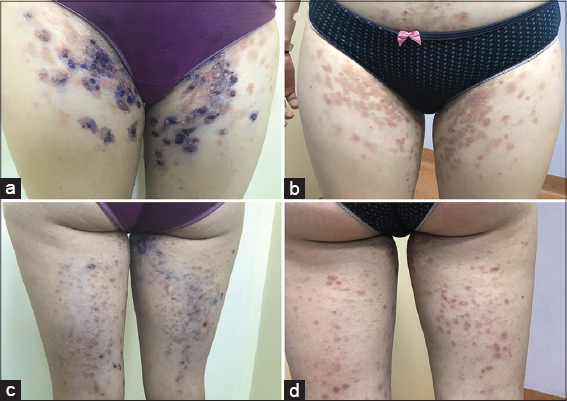
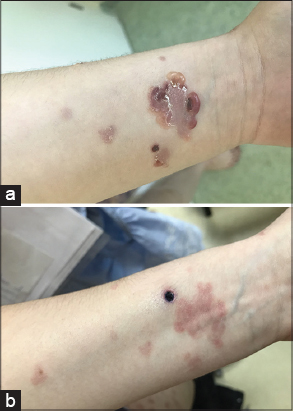
A previously healthy 17-year-old female patient presented with a 5-months history of vesicular eruptions. Physical examination revealed multiple vesicles and bullae on an erythematous base. First eruptions appeared in axillae and groins. The initial diagnosis was Hailey-Hailey disease. Topical treatment was established with gradual progression of the disease. The lesions spread on the lower trunk. back thigh surfaces, neck, facial skin around the mouth. The typical bullous eruption with a ‘string of pearls’ sign appeared on left forearm. Oral mucosa, eyes, and nails were spared. General condition was good.
The patient’s blood test revealed elevated antibodies against thyroid peroxidase (TPO) and antibodies against thyroglobulin (TG). The thyroid stimulating hormone (TSH) was 4,88 mU/L (0,27-4,2), with a free triiodothyronine (fT3) of 2,6 pmol/L (3,1–6.8) and a free thyroxine (fT4) of 9.6 pmol/L (12.0–22.0). Other laboratory studies including hematological examination, blood biochemistry, and urine analysis, antinuclear antibodies were normal. The family history of autoimmune diseases was negative.
Direct immunofluorescence (DIF) of biopsy specimens of normal skin demonstrated linear IgA-deposit pattern at the dermo-epidermal junction (DEJ) in the absence of other immunoglobulins and complement. Indirect immunofluorescence of serum was negative.
With the above findings, a diagnosis of LABD and Hashimoto thyroiditis was made. The patient was started on a course of oral dapsone 50 mg daily to which her skin lesions responded (Figs. 1 and 2). The treatment was well tolerated and produced no side effects. The patient is under the care of the Dermatology and Endocrinology Departments.
DISCUSSION
LABD is defined according to the three following clinical and histological criteria: vesicular or bullous eruption involving skin and mucous membranes (MMs), subepidermal blisters infiltrated predominantly by neutrophils in lesion biopsies and a linear IgA-deposit pattern at DEJ in the absence of other immunoglobulins on DIF [2].
The typical clinical picture is a bullous eruption with a ‘string of pearls’ sign, especially in childhood. The skin lesions in adult LABD are variable: papular, vesicular, bullous, erythematous, edematous, and erythema multiforme-like, mimicking bullous pemphigoid (BP), dermatitis herpetiformis (DH), toxic epidermal necrolysis or mucous membrane pemphigoid (MMP) [3].
In the described case, the symmetric distribution was confined to the areas typical of Hailey-Hailey disease (areas exposed to friction such as the sides of the neck, axillae, and groins) [4]. The adolescence-onset of disease was also similar to Hailey-Hailey disease.
Furthermore, the patient was diagnosed with Hashimoto thyroiditis which is also an autoimmune disease. Autoimmune diseases are common conditions which appear to develop in genetically susceptible individuals, with an expression of the disease being modified by permissive and protective environments [5].
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Ishii N, Prognostic factors of patients with linear IgA bullous dermatosisBr J Dermatol 2017; 177: 16-7.
2. Abreu Velez AM, Calle J, Howard MS, Autoimmune epidermal blistering diseasesOurDermatol Online 2013; 4: Suppl 3631-46.
3. Gottlieb J, Ingen-Housz-Oro S, Alexandre M, Grootenboer-Mignot S, Aucouturier F, Sbidian E, Idiopathic linear IgA bullous dermatosis: prognostic factors based on a case series of 72 adultsBr J Dermatol 2017; 177: 212-2.
4. Al Hamzawi NK, Hailey-Hailey disease presenting at unusualsiteOur Dermatol Online 2019; 10: 108-9.
5. Forabosco P, Bouzigon E, Ng MY, Hermanowski J, Fisher SA, Criswell LA, Meta-analysis of genome-wide linkage studies across autoimmune diseasesEur J Hum Genet 2008; 17: 236-43.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|


Comments are closed.