Topical corticosteroid abuse – a prospective clinico-epidemiological study
Department of Dermatology, Treatwell Skin Centre, Jammu and Kashmir, India
Corresponding author: Dr. Mrinal Gupta, E-mail: drmrinalgupta@yahoo.com
Submission: 29.04.2018; Acceptance: 01.07.2018
DOI:10.7241/ourd.20192.7
Cite this article: Gupta M. Topical corticosteroid abuse – a prospective clinico-epidemiological study. Our Dermatol Online. 2019;10(2):142-144.
Citation tools:
BibTex | CSV | RIS | refer/BiblX | Endnote XML | Wikipedia Citation Templates
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Misuse of topical corticosteroids (TCs) is a rampant problem in India owing to the easy availability of topical corticosteroids as over the counter preparations. TCs are being widely misused for a wide variety of skin ailments ranging from their use as skin whitening creams to infections like dermatophytoses, acne and even as daily use moisturizing creams. This misuse of TCs can lead to a large number of cutaneous and systemic adverse effects.
Aims and objectives: This study was carried out to study the prevalence and patterns of self use of TCs by the general population.
Materials and methods: This was a prospective questionnaire based study carried out over a period of one year in our centre in which the patients were questioned and assessed for misuse of TCs in terms of indication, frequency, duration and source of recommendation.
Results: A total of 200 patients (M: F 56:144) were included in our study. The age range of patients varied from 18 to 69 years with a mean age of 31.35 years. The most common indication for TCs use in our study was fungal infections (33%), facial pigmentation (26%) and acne (21%), while the most commonly abused corticosteroids were clobetasol (31%), betamethasone (28%) and mometasone (26%). The most common cutaneous adverse effects to TCs seen in our study were tinea incognito (24%), steroid acne (16%), steroid rosacea (11%), hypertrichosis (6%) and striae (4%).
Conclusion: TCs misuse in patients is quite common, which can lead to serious adverse effects. Generating awareness among the general population is necessary to curb the menace.
Key words: Topical corticosteroids, Steroid abuse, Steroid rosacea, Steroid acne, Tinea incognito
INTRODUCTION
Topical corticosteroids (TCs) are one of the most commonly used preparations in dermatology practice. Their rapid anti-inflammatory, immunosuppressive and anti-pruritic activity has made them the drug of choice for a large number of dermatoses [1]. Apart from the well documented uses of TCs, they can also cause a wide array of adverse effects if used indiscriminately or for long duration without supervision which include steroid rosacea, acneiform eruption, hypertrichosis [2]. TCs misuse is a common problem in our country owing to their easy availability as over the counter medication and preparations and lack of awareness among the general population. TCs are commonly being used as fairness and anti acne medications by the general population without any dermatological consultation which has led to a significant number of patients presenting with cutaneous adverse effects of TCs to the dermatologists [2,3].
This study was carried out in a dermatology outpatient centre with the main aims of studying the clinic-epidemiological features of TCs misuse among the general population.
MATERIALS AND METHODS
This was a prospective, questionnaire based study carried out over a period of one year in our centre in which the patients were questioned and assessed for misuse of TCs in terms of indication, frequency, duration and source of recommendation. All the patients who had self-medicated with TCs or had used TCs beyond the prescribed time advised by the dermatologists were included in the study. The patients were assessed regarding the formulation, frequency, duration or indications of TCs use for different skin conditions and the various cutaneous adverse effects, wherever present, were also noted.
RESULTS
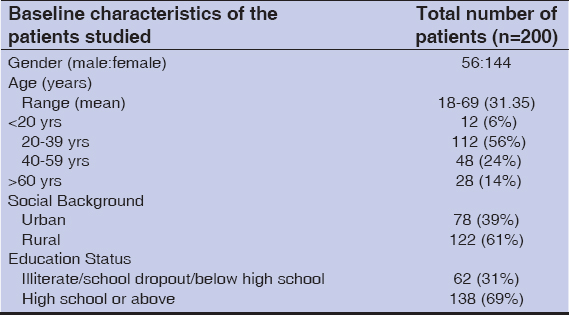
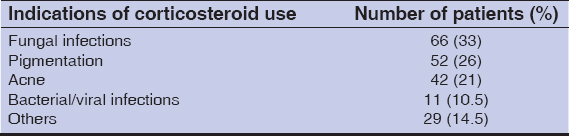
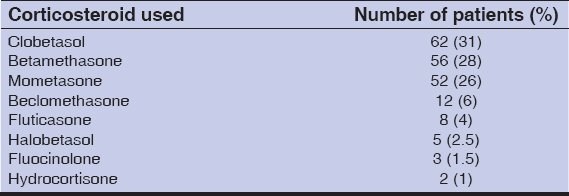
A total of 200 patients (M: F 56:144) were included in our study. The age range of patients varied from 18 to 69 years with a mean age of 31.35 years. Their baseline demographic featuresare shown in Table 1. The majority, 112 (56%) patients were of 20–40 years age group and 61% (n=122) patients belonged to a rural background and 31% (n=62) were illiterate or high school dropouts. The most common indications of TCs use in our study population were fungal infections in 66 patients (33%), facial pigmentation in 52 (26%) and acne in 42 patients (21%) (Table 2), while the most commonly abused corticosteroids were clobetasol (31%), betamethasone (28%) and mometasone (26%) (Table 3). The duration of TCs use varied from three days to eight years in our study group whereas the frequency of use varied from thrice a week to thrice a day.
The majority, 84 (42%) patientswere using topical corticosteroids on advice of pharmacists or paramedical personnel; 48 (24%) were advised by friends and relatives, 21 (10.5%) were advised by beauty parlors and beauticians. Thirty one patients (15.5%) were using the TCs advised by the dermatologists, but had been using them for a period beyond the advised time frame.
In our study group, 87 patients (43.5%) showed cutaneous adverse effects of TCs use, the most common ones being tinea incognito in 48 patients (24%), steroid acne in 32 (16%), steroid rosacea in 22 (11%), hypertrichosis in 12 (6%) and striae in 8 patients (4%).
The lack of awareness among the population can be gauged from the fact that only 16% patients (n=32) were aware of the adverse effects of TCs misuse.
DISCUSSION
The dermatological therapy underwent a sea change with the introduction of Hydrocortisone in 1952, which was followed by the development of a large variety of more potent topical corticosteroids. Owing to their potent anti-inflammatory, anti-proliferative, immunosuppressive, anti-pruritic and atrophogenic effect on the skin, TCs have become the most commonly used drugfor various hyperproliferative, inflammatory, and immunologic disorders of the skin [1]. But these properties of TCs have proven to be a double-edged sword as they provide rapid symptomatic relief in a large number of dermatoses, owing to which, they are commonly being sold over-the-counter and used by the patients irrespective of the underlying disease. Surprisingly, they are commonly being used as anti-acne and fairness creams by a large number of young patients. Their low cost and easily availability has added to growing menace [2,3].
The problem of TCs abuse has been widely reported from all over the developing world. A study from Iraq reported that 7.9% of our patient attendees in dermatology clinic had misused TCs [4]. In a similar study by Saraswat et al in India, 433 patients misusing TCs were studied. It was observed that the majority were females (n=321) and the most common age group was 21-30 years (36%), which was similar to our study group where the females outnumbered males (M: F 1:2.57) and the most common age group was 20-40 years (56%) [5]. This demographic feature could be attributed to the increased cosmetic concern in females and exposure to media among this age group. Most of the patients in our study belonged to a rural background which highlights the less availability of dermatologists in the rural setup and the easy availability of TCs and dispensing by the local pharmacists.The most common indications of TCs use in our study population were fungal infections (33%), facial pigmentation (26%) and acne (21%). Surprisingly, TCs are the not the first line drugs in any of these dermatoses. This was in concordance with the results of study by Saraswat et al where the most common indications of steroid abuse were face cream/fairness cream/after shave cream (29%), acne (24%), as a lightening agent in melasma (17%) [5]. In a study by Brar et al, acne was the most common indication of steroid use in 68% followed by melasma or skin lightening use in 22% [6]. This aspect can be attributed to the lack of awareness among the general population towards the use of TCs.
The most commonly abused corticosteroids in our study were clobetasol (31%), betamethasone (28%) and mometasone (26%), which are among the most potent of TCs. A significant number of patients (16%, n=32) were using the irrational over-the-counter three or four drug combinations which include a corticosteroid, an antibiotic and an antifungal, while 20% (n=40) were using the variants of Kligman’s formula (corticosteroid, hydroquinone, tretinoin) for pigmentation. The inappropriate use of TCs can lead to multiple side effects including atrophy, striae, telengiectasis, purpura, hypopigmentation, acneiform eruptions, rosacea-like perioral and periorbital dermatitis and hypertrichosis and even iatrogenic Cushing’s syndrome [5,7–9]. In our study, 43.5% (n=87) patients presented with cutaneous adverse effects of TCs, the most common ones being tinea incognito (24%), steroid acne (16%), steroid rosacea (11%), hypertrichosis (6%) and striae (4%). Similar observations were made by Hariharasubramony et al, who reported acneiform eruptions in 52% patients, followed by hypertrichosis, infections and telengiectasias [10].
Our study had several limitations. The small number of study population and the study being limited to the OPD of a single centre doesn’t characterize the whole population in general.
The study reveals the rampant problem of TCs abuse in our setup. The general public and the health care providers at the peripheral levels need to be made aware of the serious adverse effects of inappropriate TCs use and a strict regulation should be brought to control the unauthorized sale of TCs as over the counter preparations without proper prescription by the doctor.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Becker DE. Basic and clinical pharmacology of glucocorticosteroids. Anesth Prog. 2013;60:25–31.
2. Dey VK. Misuse of topical corticosteroids:A clinical study of adverse effects. Indian Dermatol Online J. 2014;5:436–40.
3. Jha AK, Sinha R, Prasad S. Misuse of topical corticosteroids on the face:A cross-sectional study among dermatology outpatients. Indian Dermatol Online J. 2016;7:259–63.
4. Al-Dhalimi MA, Aljawahiri N. Misuse of topical corticosteroids:A clinical study from an Iraqi hospital. East Mediterr Health J. 2006;12:847-52.
5. Saraswat A, Lahiri K, Chatterjee M, Barua S, Coondoo A, Mittal A, et al. Topical corticosteroid abuse on the face:A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160-6.
6. Brar BK, Nidhi K, Brar SK. Topical corticosteroid abuse on face:A clinical, prospective study. Our Dermatol Online. 2015;6:407-10.
7. Hengge UR, Ruzicka T, Schwartz RA, Cork MJ. Adverse effects of topical glucocorticosteroids. J Am Acad Dermatol. 2006;54:1-15.
8. Inakanti Y, Thimmasarthi VN, Anupama, Kumar S, Nagaraj A, Peddireddy S, et al. Topical corticosteroids:Abuse and Misuse. Our Dermatol Online. 2015;6:130-4.
9. Rustowska A, Wilkowska A, Nowicki R. Iatrogenic Cushing syndrome due to topical glicocorticosteroid therapy. Our Dermatol Online. 2013;4:503-5.
10. Hariharasubramony A, Sujatha VC, Harikishan Y, Raghunath N, Anagha RB. Topical corticosteroid abuse on the face:a prospective, study on outpatients of dermatology. Our Dermatol Online. 2014;5:5-8.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.