Basal cell carcinoma of the leg: an unusual location
Anissa Zaouak 1, Leila Bouhajja1, Faten Rebhi1, Raja Jouini2, Houda Hammami1, Samy Fenniche1
1, Leila Bouhajja1, Faten Rebhi1, Raja Jouini2, Houda Hammami1, Samy Fenniche1
1Department of Dermatology, Habib Thameur Hospital, Tunis, Tunisia; 2Department of Pathology, Habib Thameur Hospital, Tunis, Tunisia
Corresponding author: Dr. Anissa Zaouak, E-mail: anissa_zaouak@yahoo.fr
Submission: 02.09.2018; Acceptance: 01.11.2018
DOI:10.7241/ourd.20192.30
Cite this article: Zaouak A, Bouhajja L, Rebhi F, Jouini R, Hammami H, Fenniche S. Basal cell carcinoma of the leg: an unusual location. Our Dermatol Online. 2019;10(2):211-212.
Citation tools:
BibTex | CSV | RIS | refer/BiblX | Endnote XML | Wikipedia Citation Templates
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
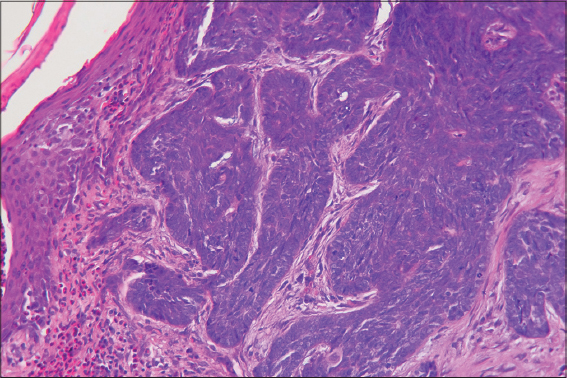
We report a 58-year-old man without a significant medical history presented to our clinic with a non-healing, slowly growing non tender ulcer on his right leg that he had for more than one year. The ulcer despite several would care measures progressively increased. Clinical signs of arterial insufficiency or venous insufficiency were not detected. Vascular studies with duplex ultrasonography failed to reveal any venous reflux. Dermatological examination revealed a well-demarcated 4×5 cm clean based ulceration with heaped-up borders located on his right leg. The base of the ulceration had normal granulation tissue (Fig. 1). Dermoscopic findings revealed arborizing vessels and short fine vessels. In addition, there were large blue grey ovoid nests. The chronic, poorly healing nature of the leg ulcer prompted us to perform a skin biopsy of the edge of the ulcer including the base which revealed large well-defined derma nodules, basaloïd cells with peripheral nuclear palisading and clefting between tumor and stroma (Fig. 2). Correlation of clinical, dermoscopic and histopathological findings allowed us to confirm the diagnosis of basal cell carcinoma of the leg. The patient was referred to an oncologist for a surgical excision of the tumor.
The patient’s informed consent was obtained.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
Basal cell carcinoma (BCC) is preferentially located in photo-exposed areas. Its occurrence on the legs is rarely reported in the literature and account for about 8% of BCCs [1]. It is more common in males than females and is a great masquerader. In fact, BCC can mimic many dermatoses as in our case where it was misdiagnosed with a venous leg ulcer and can appear in unsuspected areas as the lower limbs. In front of a chronic leg ulcer, differential diagnosis may include venous or arterial ulcers, malignancies such as squamous cell carcinoma, amelanotic melanoma, cutaneous lymphoma and basal cell carcinoma, infectious ulcers, pyodema gangrenosum, traumatic and factitial wounds [2–4]. In our case, the chronic leg ulcer was misdiagnosed as a venous leg ulcer in the absence of clinical and ultrasonographic signs of venous insufficiency leading to an important diagnostic delay. Hence, physicians should be aware that BCC could develop de novo and that the appearance of a granulation tissue with pearly indurated borders and central ulceration should prompt suspicion. Although these tumors rarely metastasize, delayed treatment may result in significant morbidity from local invasion leading to destruction of the skin and deeper tissues. Dermoscopy could be useful in raising the suspicion of malignancy but the definitive diagnosis relies mainly on skin biopsy in front of a non healing chronic leg ulcer. Dermoscopically, basal cell carcinoma of the lower extremity is characterized by the presence of polymorphous vessels and thin serpentine vessels with lower prevalence of arborizing vessels compared to other anatomic sites [5].
The correlation of history taking, clinical examination, dermoscopic findings and histopathological findings in our case allowed us to establish the diagnosis of basal cell carcinoma of the lower extremity. An early detection of these rare tumors in this rare localization is important in our case to avoid tumor extension and significant morbidity.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from the patient for publication of this article.
REFERENCES
1. Conde-Taboada A, De la Torre C, Flórez A, García-Doval I, Cruces M. Chronic leg ulcers and basal cell carcinoma. J Eur Acad Dermatol Venereol. 2006;20:359.
2. Hwang J, Wong E. Non-healing, non-tender ulcer on shin. J Fam Pract. 2015;64:421-24.
3. CelićD, LipozenčićJ, LjubojevićHadžavdićS, Kanižaj RajkovićJ, LončarićD, BorlinićT. A Giant basal cell carcinoma misdiagnosed and mistreated as a chronic venous ulcer. Acta Dermatovenerol Croat. 2016;24:296-98.
4. Tchanque-Fossuo CN, Millsop JW, Johnson MA, Dahle SE, Isseroff RR. Ulcerated basal cell carcinomas masquerading as venous leg ulcers. Adv Skin Wound Care. 2018;31:130-34.
5. Lombardi M, Pampena R, Borsari S, Bombonato C, Benati E, Pellacani G, et al. dermoscopic features of basal cell carcinoma on the lower limbs:a chameleon!Dermatology. 2017;233:482-88.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-2062-2256? http://orcid.org/0000-0003-2062-2256?
|



Comments are closed.