Standardization of modified Limberg flap technique by using an acetate template for the treatment of pilonidal disease
Aksaray University School of Medicine, Department of General Surgery, Aksaray, Turkey
Corresponding author: Dr. Mehmet Eren Yuksel, E-mail: doctormehmeteren@yahoo.com
Submission: 12.11.2018; Acceptance: 30.01.2019
DOI:10.7241/ourd.20192.1
Cite this article: Yuksel ME. Standardization of modifi ed Limberg fl ap technique by using an acetate template for the treatment of pilonidal disease. Our Dermatol Online. 2019;10(2):112-115.
Citation tools:
BibTex | CSV | RIS | refer/BiblX | Endnote XML | Wikipedia Citation Templates
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Pilonidal disease is a common condition that usually affects young men. The disease presents with pain, cysts, abscesses, pits, sinus tracts, retained hairs and draining in the sacrococcygeal area. Various surgical techniques have been described in the treatment of pilonidal disease. Modified Limberg flap is a commonly used procedure, however, studies which compared the outcomes of modified Limberg flap technique have reported different results. Diverse geometric rhomboid excisions in shape and size, and varied lateralization distance can lead to differences in healing time, complication and recurrence rates. Standardization of the modified Limberg flap technique can help to compare the end results of the surgical intervention more accurately. Therefore, we developed an acetate template to draw a sketch map of Limberg/modified Limberg flap preoperatively, in order to standardize the procedure.
Materials and Methods: A Limberg/modified Limberg flap template was prepared by using an online drawing program. Rhomboid flaps with four different sizes were drawn. The template was printed onto an acetate sheet. With the help of a sewing needle, pin holes were performed on the acetate template. The borders of the rhomboid excision and the Limberg/modified Limberg flap were defined with the acetate template and drawn on the gluteal region by using a water resistant multi-purpose pen. The surgeon decided which rhomboid flap size to choose according to the dispersion of the pilonial sinus openings. All pilonidal pits and abscess orifices stayed within the resected area. The size of modified Limberg flap was standardized by the help of the acetate template.
Results: This study included 10 male patients with pilonidal disease between the ages of 20 to 35. The mean disease duration of the patients was 4.2 years. All the patients underwent modified Limberg flap surgery using an acetate template. The follow-up period was three months. We observed surgical site infection only in one patient within seven days, postoperatively.
Conclusions: We suggest that using a standardized template while performing a modified Limberg flap procedure for the treatment of pilonidal disease may help to evaluate and compare the outcomes of this surgical procedure more accurately.
Key words: Flap, Limberg, Modified Limberg, Pilonidal disease, Pilonidal sinus, Surgery
INTRODUCTION
Pilonidal disease is a common condition among young adults. The exact cause remains controversial. However, obstruction of hair follicles in the natal cleft has been implicated in the etiology of pilonidal disease. It is more common in men than in women. Pilonidal disease usually starts in patients under the age of 30. The risk factors in the development of pilonidal disease include male gender, obesity, sitting for long periods, chronic trauma to the sacrococcygeal area, excess body hair and poor hygiene [1].
Pilonidal disease clinically presents with cyst, abscess with retained hair, pits, sinus tracts with or without draining in the gluteal cleft [2,3]. Acute pilonidal abscess leads to erythema, edema, tenderness and pain while chronic pilonidal abscess is characterized by chronic pilonidal sinus cavity with recurrent drainage as a result of retained hair and infected residue [3].
The diagnosis of pilonidal disease is made based on typical clinical findings like inflammation adjacent to the gluteal cleft with associated midline pits [4]. Acute pilonidal abscess is treated with incision and drainage. Antibiotic use is not recommended except for the immunosuppressed or toxic appearing patients, and patients who have risk for endocarditis or methicillin-resistant Staphylococcus aureus infection [4].
Some pilonidal abscesses have been associated with a malignant change, which is called Marjolin’s ulcer [5]. Therefore, a biopsy should be performed in patients who do not respond to conservative management to rule out squamous cell carcinoma [4].
A definitive treatment should be performed following the regression of acute inflammation. Treatment options include excision and laying open/primary closure, minimally invasive procedures like crystallized phenol treatment, pit picking surgery and endoscopic sinus treatment, off-midline procedures like Limberg flap and Karydakis flap, advancement flaps like Karydakis procedure, Z flap and V–Y flap [6,7]. However, none of these procedures has been considered as the gold standard [7].
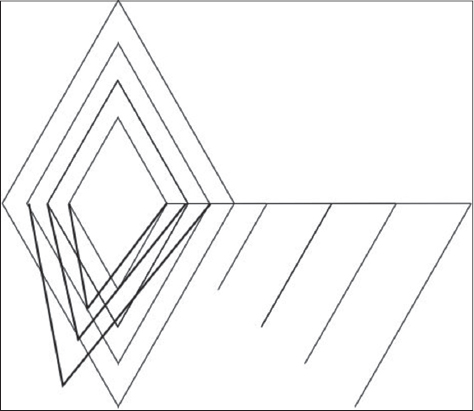
Modified Limberg flap procedure is a safe and effective technique in the treatment of pilonidal disease with low complication and recurrence rates [8]. However, there is no standardized rhomboid shape and excision style between general surgeons while performing modified Limberg flap surgery (Fig. 1). Hereby, a modified Limberg flap technique performed by using a template has been described.
MATERIALS AND METHODS
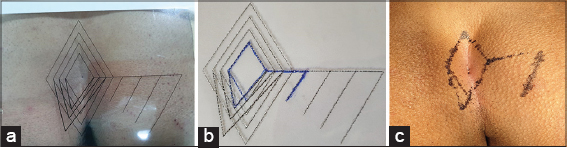
With the help of an online drawing program (https://www.draw.io/), a sketch was prepared. Rhomboid flaps with four different sizes were drawn (Fig. 2). Each rhomboid was an parallelogram with all equal sides. Inner angles of the rhomboid were 60° and 120°. In order to apply modified Limberg flap technique, shifting of the midline/intergluteal sulcus to the left was also drawn. The template was printed onto an acetate sheet (Canon Pixma, MG 2550). With the help of a sewing needle, pin holes were performed on the acetate sheet template (Figs. 3a – 3c). A water resistant multi-purpose pen (edding 149M, Japan) was applied onto the pin holes on the acetate template. Finally, the borders of the rhomboid excision and the Limberg/modified Limberg flap were defined and drawn onto the gluteal region by using the acetate template.
RESULTS
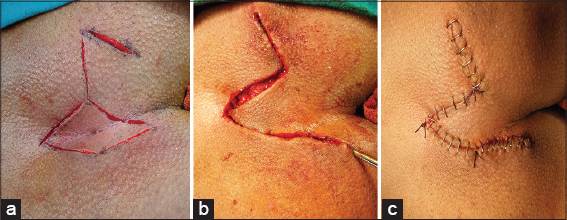
This study included 10 male patients with pilonidal disease at the age of 20 to 35. The mean disease duration of the patients was 4.2 years. Two patients were treated with crystallized phenol technique previously, however, the symptoms recurred within 12 months. Eight patients did not receive any prior treatment except for non-steroidal anti-inflammatory drugs to relieve pain. The past medical history and family history were both unremarkable. All the patients underwent surgery using the technique described above (Figs. 4a – 4c). No complications have been observed intraoperatively. The patients were discharged on postoperative day one. The follow-up period was three months. The surgical site infection was observed in a patient within seven days, postoperatively. The patient was treated with oral administration of ciprofloxacin 500 mg and metronidazole 500 mg twice daily for one week without any adverse effect.
DISCUSSION
Pilonidal disease can be treated with various surgical methods, however, risk of recurrence remains high [9]. Recurrence rate of 20-40% has been reported regardless of the surgical technique [10]. Flap techniques provide a flattened intergluteal sulcus, tension-free repair, less hairy tissue and reduced sweating [9]. The classic Limberg flap consists of symmetrical rhomboid shaped excision in which the apices are placed on the midline. Recurrence can be observed in the excision site at the lower midline apex of the rhomboid flap following the classic Limberg flap. Therefore, the classic Limberg flap was modified in 2004 to prevent this complication. The rhomboid-shaped excision is made asymmetrically to move away the apex of the flap1 to 2 cm lateral side to the inferior midline [11].
Modified Limberg flap is one of the most commonly used procedure with satisfactory outcomes, short healing time and good long-term results [12,13]. However, modified Limberg flap can lead to disfigurement in the sacrococcygeal area as a result of creating a geometric shaped flap. The procedure may not be appropriate for patients with extensive pilonidal disease which requires larger flaps [12]. Modified Limberg flap closure has been compared with other surgical techniques which are used in the treatment of pilonidal disease. Shabbir et al. reported that modified Limberg flap closure has less infection and recurrence rates, short hospital stay and better patient comfort when compared with excision and direct primary closure [13]. Khan et al. compared early outcome of modified Limberg and Karydakis flap procedures. Khan et al. reported significantly less wound infection and seroma formation in patients treated with modified Limberg procedure [14]. Sit et al. compared the Karydakis, modified Limberg and Limberg flap techniques in the treatment of pilonidal disease. Modified Limberg had significantly low maceration, recurrence, and hypoesthesia rates. Mean off-work period, time to walk without pain, and period to take the drainage off were shorter in modified Limberg compared to Karydakis and Limberg flap techniques [15].
However, Tokac et al. reported no significant difference in patient comfort and recurrence risk between modified Limberg flap and Karydakis flap surgeries. Patients treated with modified Limberg flap had shorter healing time, while better cosmetic results have been achieved in Karydakis flap procedure [16]. Can et al. compared modified Limberg flap and Karydakis flap procedures in the treatment of pilonidal disease. Complication and recurrence rates were similar in both techniques. Patients underwent Karydakis flap reported shorter healing time postoperatively [17]. Abdelnaby et al. compared the outcomes of modified Limberg flap and rotational gluteal flap. Both modified Limberg flap and rotational gluteal flap have low recurrence rates, however, rotational gluteal flap had shorter healing time, lower complication rate and better cosmetic appearance [12]. Studies that compared surgical techniques especially modified Limberg flap and Karydakis flap in the treatment of pilonidal disease had different results. Differences in shape and size of a geometric rhomboid excision and different lateralization distance can lead to controversy in healing time, complications rates and recurrence rates in comparing modified Limberg flap procedure to other techniques.
CONCLUSION
In conclusion, we have developed an acetate template to draw a sketch map of Limberg/modified Limberg flap preoperatively, in order to standardize the procedure. Using a standardized template while performing a modified Limberg flap surgery may help to evaluate the outcomes of this technique more accurately.
REFERENCES
1. Segre D, Pozzo M, Perinotti R, Roche B. Italian Society of Colorectal Surgery. The treatment of pilonidal disease:Guidelines of the Italian Society of Colorectal Surgery (SICCR). Tech Coloproctol. 2015;19:607-13.
2. Srihari RS, Naveen AM, Sreekar H. The Limberg flap reconstruction – the optimal surgery for pilonidal sinus disease. Our Dermatol Online. 2016;7:271-5.
3. Khanna A, Rombeau JL. Pilonidal disease. Clin Colon Rectal Surg. 2011;24:46-53.
4. Kuckelman JP. Pilonidal disease:Management and definitive treatment. Dis Colon Rectum. 2018;61:775-7.
5. Brzezinski P, Solovan C, Chiriac A. Malignant degeneration of scars in elderly people (Marjolin’s ulcers). Int Wound J. 2016;13:1047-8.
6. Iesalnieks I, Ommer A, Petersen S, Doll D, Herold A. German national guideline on the management of pilonidal disease. Langenbecks Arch Surg. 2016;401:599-609.
7. Boshnaq M, Phan YC, Martini I, Harilingam M, Akhtar M, Tsavellas G. Limberg flap in management of pilonidal sinus disease:Systematic review and a local experience. Acta Chir Belg. 2018;118:78-84.
8. Hussain SM, Farees SN, Abbas SJ, Vakati Raghavendra SK. Rhomboid excision with modified Limberg flap in the treatment of sacrococcygeal pilonidal disease. Arch Int Surg. 2015;5:74-7.
9. Singh PK, Gohil RK, Saxena N. Limberg flap procedure for sacrococcygeal pilonidal sinus:A prospective study. Int Surg J. 2017;4:2238-42.
10. Aithal SK, Rajan CS, Reddy N. Limberg flap for sacrococcygeal pilonidal sinus a safe and sound procedure. Indian J Surg. 2013;75:298-301.
11. Bessa SS. Comparison of short-term results between the modified Karydakis flap and the modified Limberg flap in the management of pilonidal sinus disease:A randomized controlled study. Dis Colon Rectum. 2013;56:491-8.
12. Abdelnaby M, Emile SH, El-Said M, AbdelMawla A, Elgendy H, Sakr A, et al. Rotational gluteal flap versus modified Limberg flap in treatment of sacrococcygeal pilonidal disease. J Surg Res. 2018;223:174-82.
13. Shabbir F, Ayyaz M, Farooka MW, Toor AA, Sarwar H, Malik AA. Modified Limberg’s flap versus primary closure for treatment of pilonidal sinus disease:A comparative study. J Pak Med Assoc. 2014;64:1270-3.
14. Khan KJ, Ghaffar A, Choudhry S, Irshad K. Comparison of early outcome between modified Limberg and Karydakis flap procedures in patients with sacrococcygeal pilonidal sinus. PJHMS. 2016;10:631-4.
15. Sit M, Aktas G, Yilmaz EE. Comparison of the three surgical flap techniques in pilonidal sinus surgery. Am Surg. 2013;79:1263-8.
16. Tokac M, Dumlu EG, Aydin MS, Yalc?n A, Kilic M. Comparison of modified Limberg flap and Karydakis flap operations in pilonidal sinus surgery:Prospective randomized study. Int Surg. 2015;100:870-7.
17. Can MF, Sevinc MM, Hancerliogullari O, Yilmaz M, Yagci G. Multicenter prospective randomized trial comparing modified Limberg flap transposition and Karydakis flap reconstruction in patients with sacrococcygeal pilonidal disease. Am J Surg. 2010;200:318-27.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-7110-0717 http://orcid.org/0000-0002-7110-0717
|




Comments are closed.