|
Get Citation
|
|
|
Niyaz A, Viswanath BK. Atypical presentation of pemphigus vulgaris – A rare case report. Our Dermatol Online. 2019;10(1):88-90. |
|
|
Download citation file:
|
Atypical presentation of pemphigus vulgaris – A rare case report
1Final year pg student, Dermatology, JJM Medical College, Davangere, India, 2Department of Dermatology, JJM Medical College, Davangere, India
Corresponding author: Dr. Asifa Niyaz, E-mail: asifanz26@gmail.com
Submission: 19.03.2017; Acceptance: 28.11.2017
DOI: 10.7241/ourd.20191.25
ABSTRACT
Pemphigus vulgaris is an autoimmune blistering disorder affecting the skin and mucous membrane with characteristic intraepithelial blistering. It commonly involves the oral mucosa and skin, Oral mucosal involvement may proceed the skin involvement. We here in report a case, where in the oral and skin lesion occurred concurrently in a 20 year old male with a 1 month history of multiple fluid filled lesions over the body, who is a known case of psychosis and epilepsy treated at many places as case of drug rash finally diagnosed in our hospital as case of pemphigus vulgaris.
Key words: Pemphigus vulgaris, Auto immune, Blisters, Drug rash
INTRODUCTION
Pemphigus derives its name from greek ‘pemphix’ means blister or bubble. It is an auto immune blistering disorder affecting the skin and mucous membrane of oral cavity, characterised by supra basal split in the epidermis. Nearly all patients have mucosal involvement and pemphigus vulgaris presents as oral lesions in 50 to 70% patients [1–3]. These may precede the cutaneous lesions by months or may be the only feature of the disease. Pemphigus vulgaris is most common form of pemphigus accounting for 70% cases of cases [3]. It is the commonest auto immune blistering disorder in Eastern countries like India, Malaysia, China and Middle east. It is a disease of the middle age, but patients are at a younger age at presentation in India compared to western countries and both sexes are equally affected.
CASE REPORT
A 20 year old male patient since 1 month presented complaints of multiple filled lesions on the body. Patient was dumb and mentally retarded. History was obtained from parents. Initial lesions started in both upper limbs followed by oral cavity and lower limbs for which medication was taken but was not relieved. There is no history of constitutional symptoms. Patient is a known case of psychosis and epilepsy since the age of 7 years. Patient was on anti epileptic drug phenobarbitone 60 mg, has stopped taking medication since 8 months as he developed aggression. Patient was taken to various hopitals where he was treated as a case of drug rash, with intravenous antibiotics, anti histaminics, topical antibacterial cream.
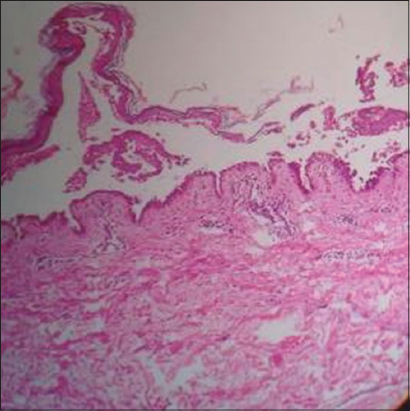
His vital signs were temperature 99º F, pulse 90 beats per min, respiration 16 cycles/min, blood pressure 110/70 mm Hg, height 5’3”, weight 50 kg. On examination, patient was ill, moderately built and moderately nourished. Skin is characterised with multiple tense fluid filled lesions over the upper limbs, lower limbs abdomen, chest and back were spared and erosions were present over the oral cavity as shown in Fig. 1 and 2. Conjunctiva were congested. Routine laboratory examination revealed Haemoglobin 11g/dl, ESR 40 mm/hr, PCV 24%, RBS 92.8 mg/dl, Albumin 3.09g/dl, Blood urea 13.1mg/dl, Serum creatinine, Serum bilirubin, Alkaline phosphatase levels were with in normal limit. Tzanck smear was done for the patient which showed few giant cells, Biopsy was done from the lesion and histopathology report revealed the following features: On microscopy (Fig. 3), epidermis shows suprabasal clefting with vesicle formation and tomb stone appearance, Vesicle is filled with neutrophils, eosinophils and acantholytic cells. Dermis shows mild perivascular lymphocytic infiltrate, Features are suggestive of Pemphigus vulgaris.
Patient was given given started on Steroids, Antibiotics, Saline compresses, Topical Antibacterial cream, H2 receptor blockers, Multivitamin capsules, Antihistaminics Tetracycline mouth gargles, Antioxidants, Topical steroid for lips, Oral analgesic gel, Ophthalmic eye drops. On follow up patient was responding well to the treatment.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
Pemphigus vulgaris is a blistering disorder of skin and mucous membrane. Predisposition to pemphigus is linked to genetic factors. The diagnosis of this disease is clinical and confirmed by histopathological examination. Nearly all patients may have mucous membrane involvement and oral cavity is commonly involved, more commonly patients have ill defined, irregularly shaped buccal or palatal erosions which are slow to heal lesions are painful which affects the appetite of the patient. Intact bullae are rare in oral cavity. Other mucous membranes involved are conjunctiva, nasal, pharynx, larynx, oesophagus, urethra, vulva and cervix [4]. Most patients develop cutaneous lesions which may remain localised or more commonly wide spread. The disease has a predilection for scalp, face, axilla, groin and pressure points. Flaccid blisters with clear fluid either arise on a normal or an erythematous base. The blisters are easily broken forming epidermal rings. Histopathological examination reveals eosinophilic spongiosis, suprabasal split with groups of acantholytic cells in the cavity, basal layer keratinocytes shows loss of adhesion with adjacent keratinocytes and characteristic row of tomb stone appearance. The basic therapy options consists of local or systemic corticosteroid therapy. Adjuvant therapies like cyclophosphamide and azathioprine are commonly used, dapsone, cyclosporine, mycophenolate mofetil and methotrexate have also been tried. Other drugs like colchicine, thalidoamide and retinoids have also been used in mild to moderate cases. Recent trials have shown an advantage that with use of low dose methotrexate to be more efficacious and relatively few side effects. Intralesional injections of corticosteroids have also been used in treatment of persistent oral lesions [5]. Traditional drugs combined with antioxidants, calcium and vitamin supplements should be given, antiseptic mouth washes should be given to improve local oral hygiene.
CONCLUSION
Pemphigus vulgaris is an autoimmune disorder the mucous membrane and skin, that is often misdiagnosed, there is an increase in morbidity rate. The diagnosis is confirmed by clinical and histopathological examination. Therapeutic and adjuvant treatments help the patients to relieve from symptoms.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Arpita R, Monica A, Venkatesh N, Atul S, Varun M. Oral Pemphigus Vulgaris:Case Report. Ethiop J Health Sci. 2015;25:367-72.
2. Matias AB, Ferreira Roselino AM. Pemphigus:a disease stamped in the skin. Our Dermatol Online. 2013;4(Suppl.3):601-5.
3. Rama Rao GR, Koteswara Rao NR, Sridevi M, Amareswar A, Chowdary AP. Pemphigus vulgaris with squamous cell carcinoma of the tongue:An uncommon association. Our Dermatol Online. 2017:8:286-8.
4. Kabra V, Pai K, Pai S, Shenoi S, Rao R. Pemphigus vulgaris masquerading as subcorneal pustular dermatoses-a case report. Our Dermatol Online. 2014:5:157-9.
5. Benhiba H, Hamada S, Guerouaz N, Saidi A, Senouci K, Hassam B. Pemphigus vulgaris:an unusual clinical presentation. Ann Dermatol Venereol. 2013:140:116-9.
Notes
Source of Support: Nil
Conflict of Interest: None declared.


Comments are closed.